Chapter 2 Anatomy of the Reproductive Tract
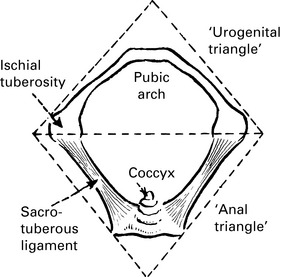
THE PERINEUM (Gk. ‘around the natal area’)
The perineum
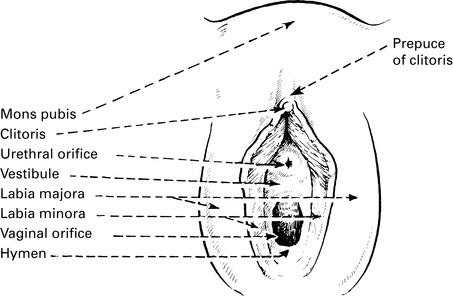
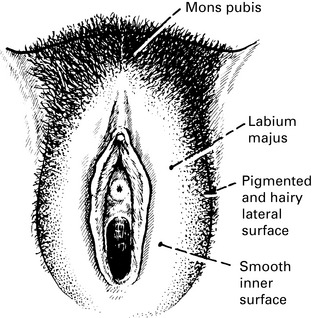
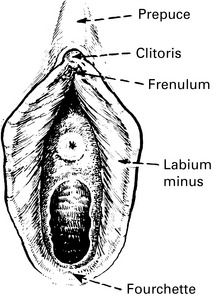
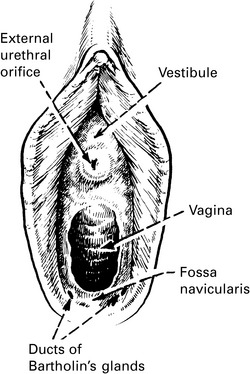
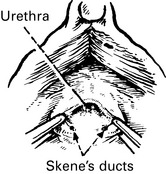
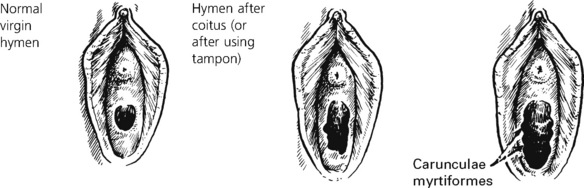
The VULVA consists of the following:
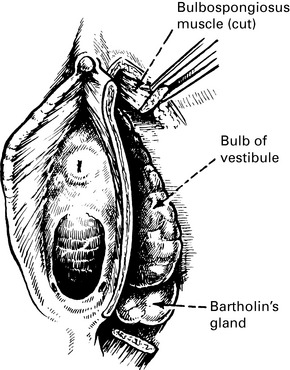
Subcutaneous: the bulb of the vestibule and the greater vestibular (Bartholin’s) glands.
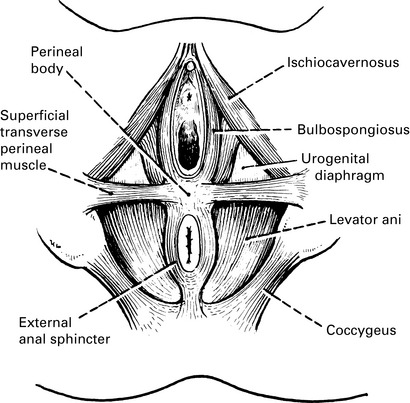
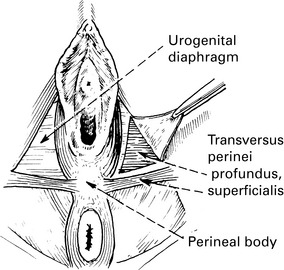
Muscles of the perineum
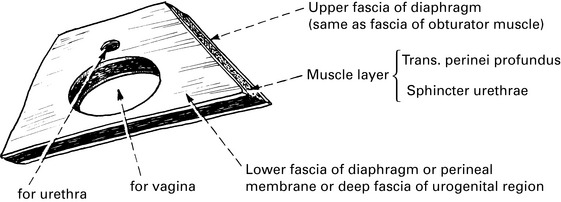
The urogenital diaphragm
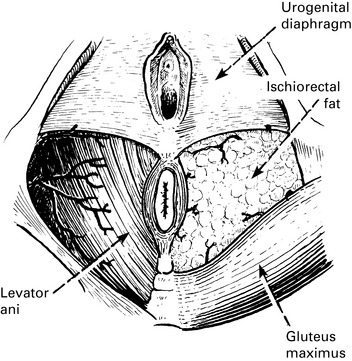
Ischiorectal fossa
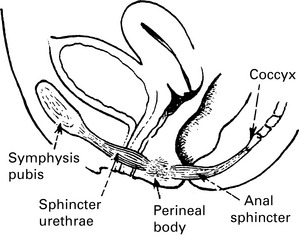
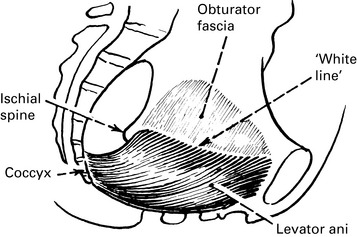
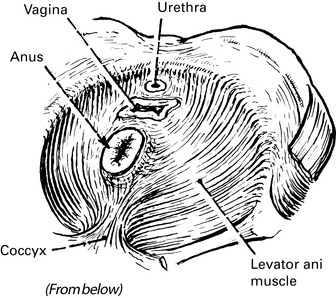
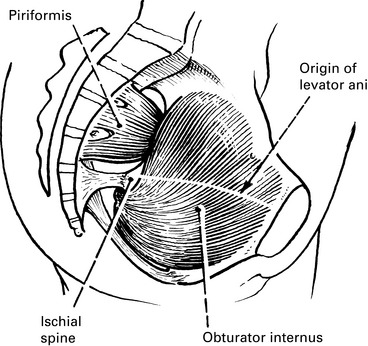
Pelvic diaphragm
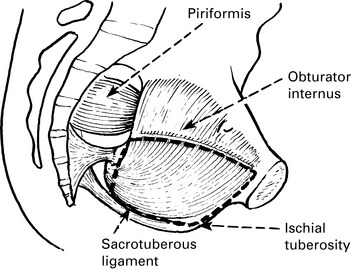
These muscles are primarily lateral rotators of the hip and postural muscles.
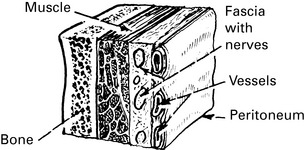
Pelvic fascia
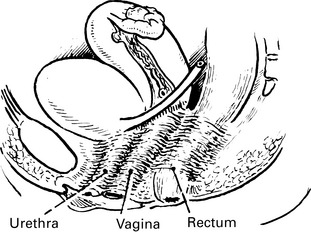
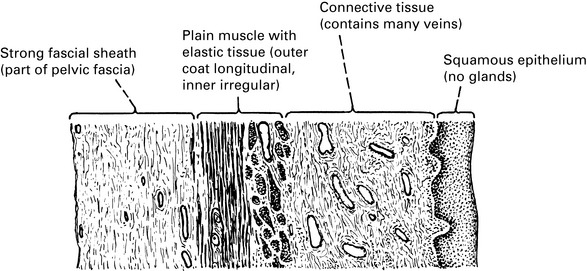
The vagina
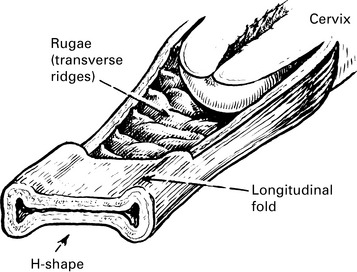
The vagina is a tubular structure extending from the vulva to the uterus.
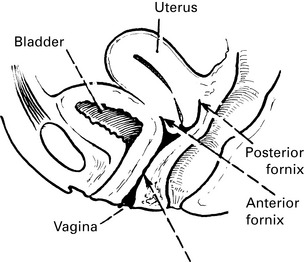
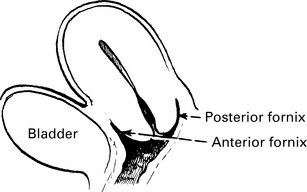
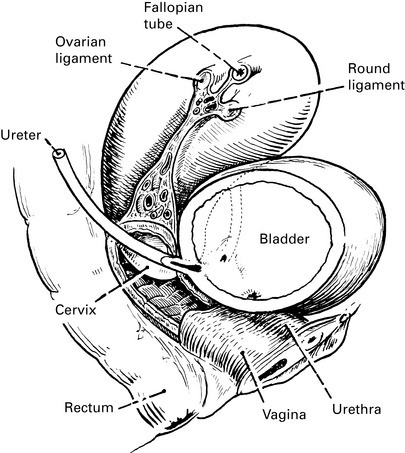
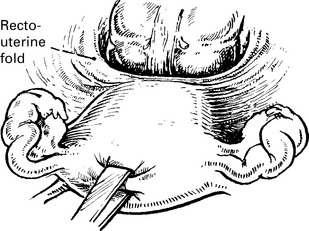
Lateral view. Note the close relationship to urethra, bladder and rectum.
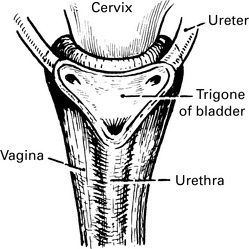
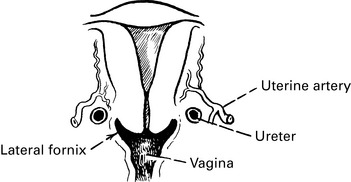
Anterior view shows the very intimate relationship with the bladder base and ureters.
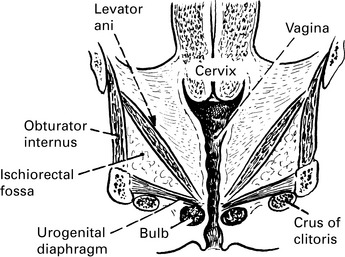
Coronal section shows the relationship of vagina and pelvic floor.
These are gutters at the top of the vagina, surrounding the cervix.
Anterior fornix – related to the bladder base and the uterovesical fossa.
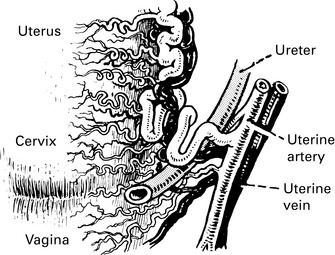
Lateral fornices – related to the ureters and the uterine vessels.
Uterus
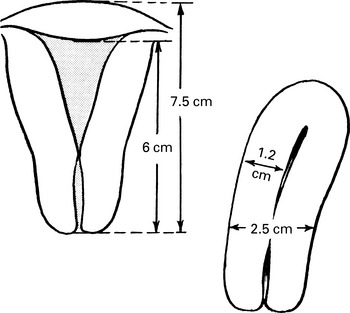
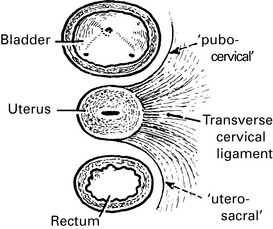
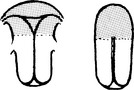
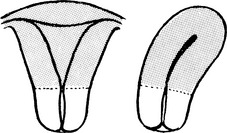
The uterus is a hollow viscus composed of smooth muscle, whose sole function is gestation.
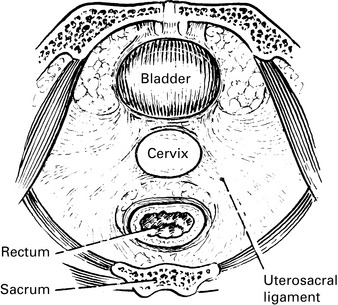
It lies between the rectum and the bladder and is continuous with the vagina.
Thickness of muscle wall is about 1.2 cm
Vaginal ultrasound can be used to measure the uterine dimensions.
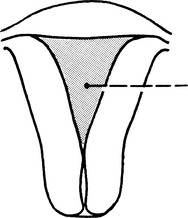
Cavity of the corpus
The anterior and posterior walls are almost in contact, but in coronal plane the cavity is triangular.
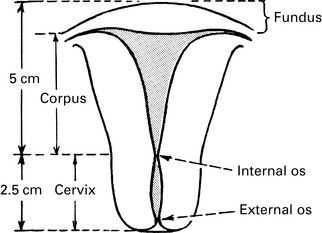
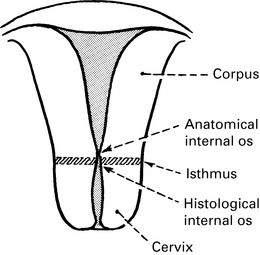
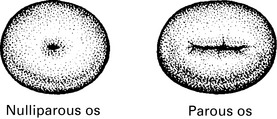
Cervix
The cervical canal is fusiform and marked by curious folds called the ‘arbor vitae’.
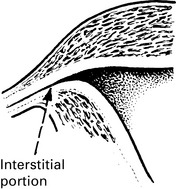
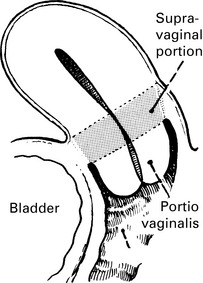
The cervix is divided into supra- and infravaginal portion by the attachments of the vagina.
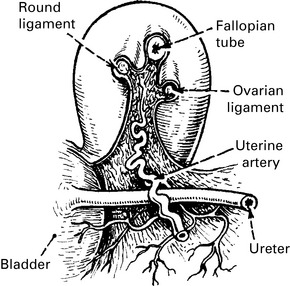
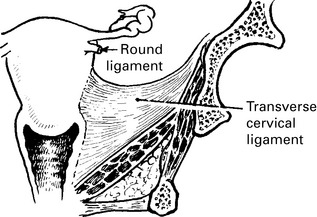
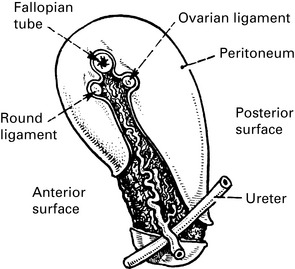
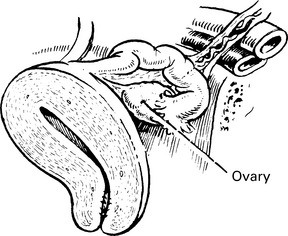
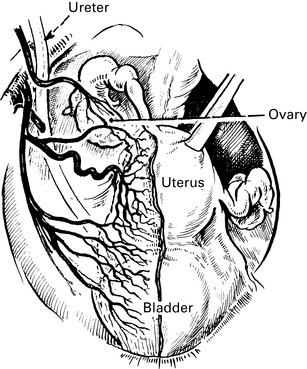
Relationship of uterus and ureter
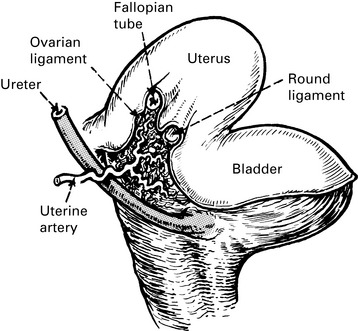
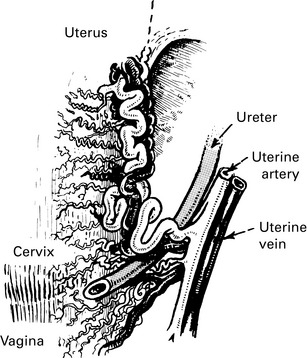
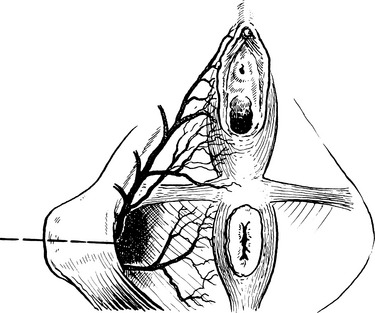
This picture shows the ureter passing under the uterine artery on its course to the bladder.
In this picture, the bladder has been removed to show just how close the ureter is to the cervix. It also demonstrates the problems that are likely to be encountered in controlling haemorrhage and avoiding damage to the ureter during surgery in this area (see pages 288–291).
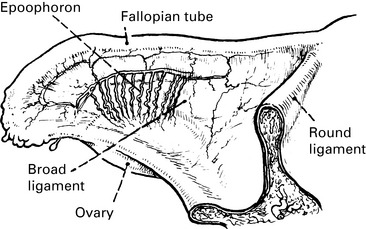
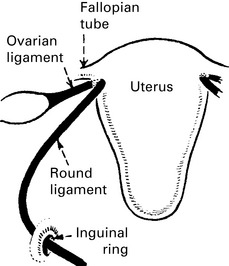
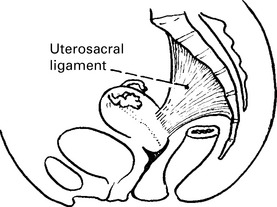
Ligaments of the uterus
The main supports of the uterus are the fibromuscular condensations of tissue in the pelvic fascia (page 21).
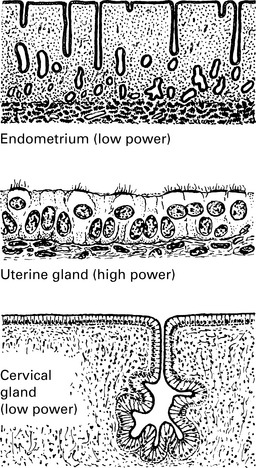
Histology
For cyclical changes in the endometrium see pages 49–51.
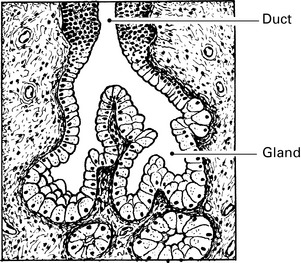
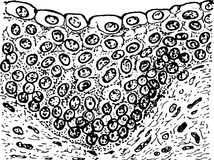
The cervix is lined by a single layer of high columnar ciliated epithelium, which covers the folds of the arbor vitae (pp. 29–30) and lines the cervical glands. The glands secrete an alkaline mucus, which is favourable to the activity of spermatozoa.
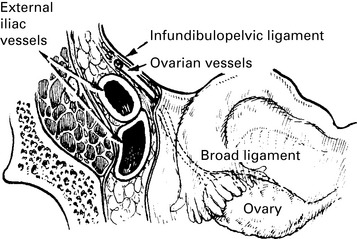
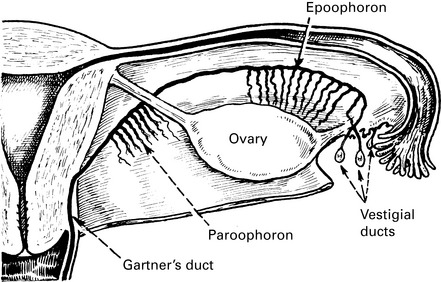
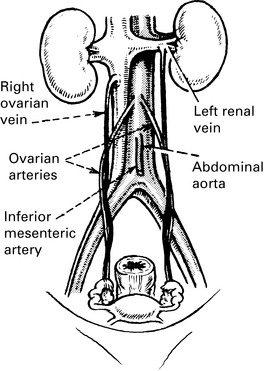
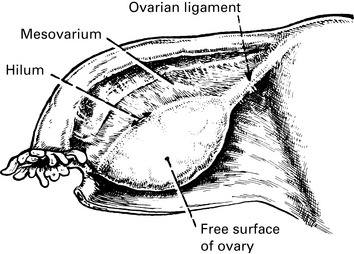
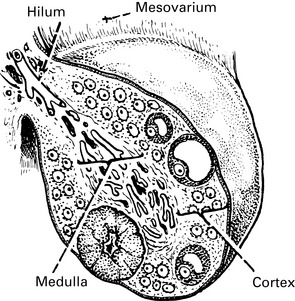
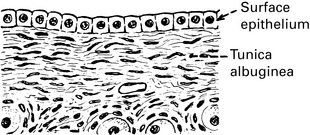
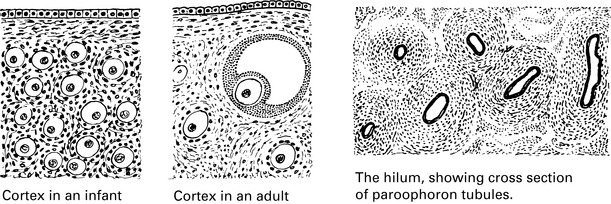
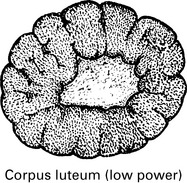
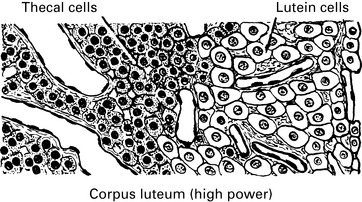
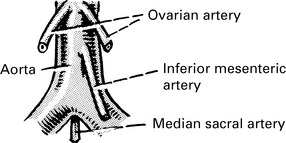
Ovary
Note: The left ovarian vein empties into the left renal vein.
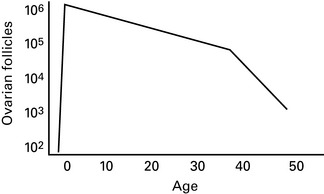
Changes in the genital tract with age
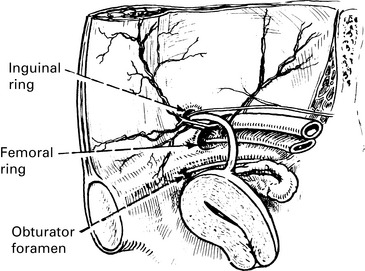
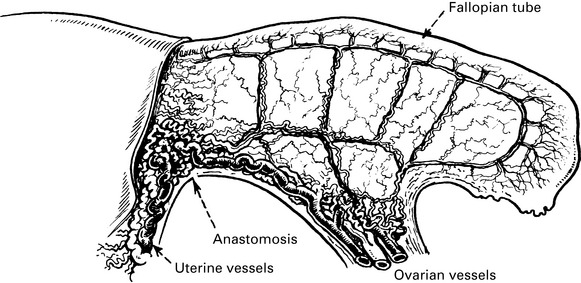
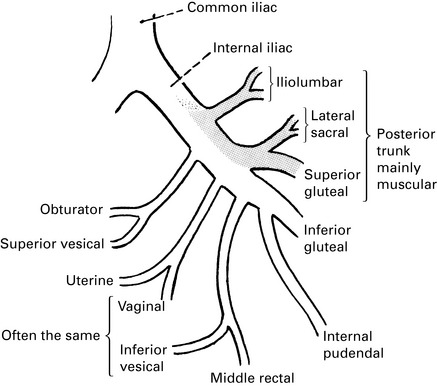
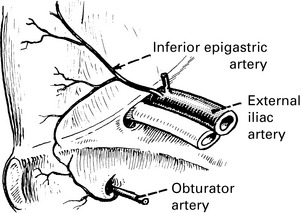
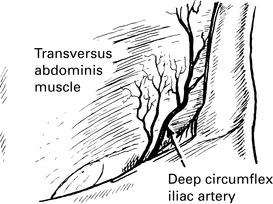
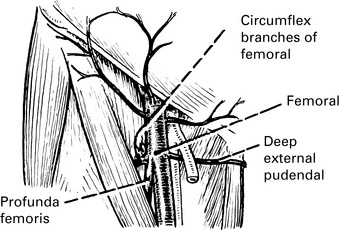
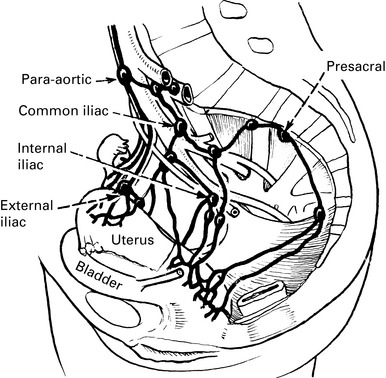
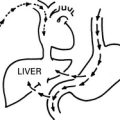
Blood supply of the pelvis
Supply to uterus, vagina and bladder
This picture shows an arrangement often met with.
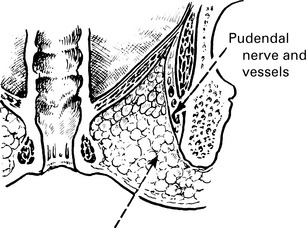
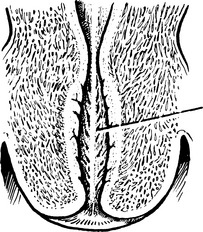
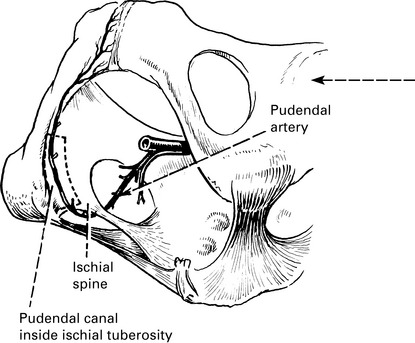
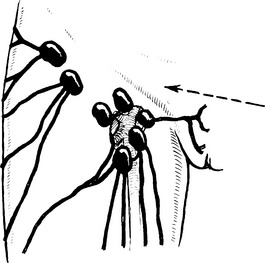
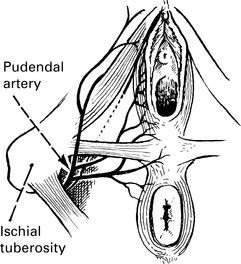
In the ischiorectal fossa, the pudendal artery divides into inferior rectal and perineal branches.
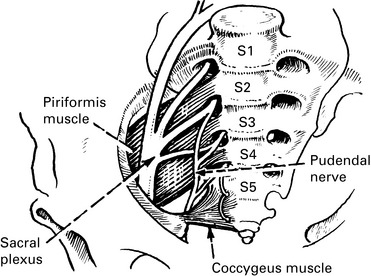
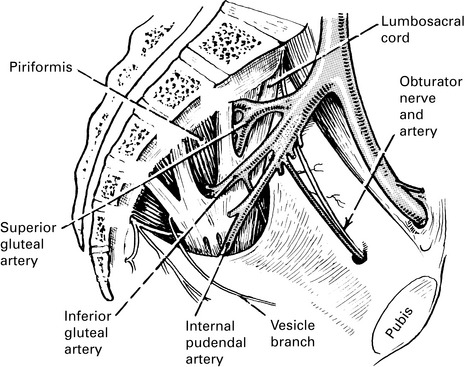
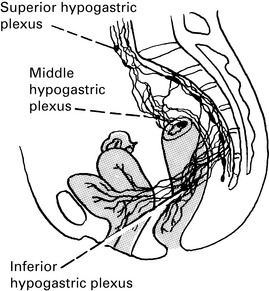
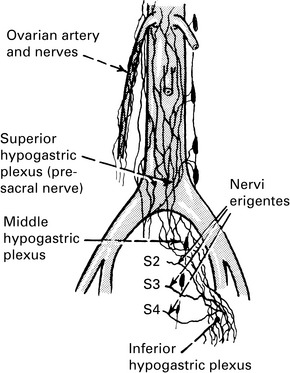
Nerves of the pelvis
The sacral plexus lies on the piriformis muscle beneath the vessels.
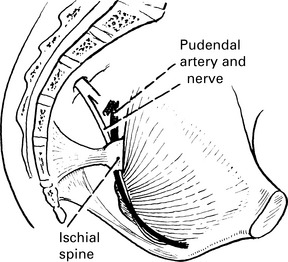
The pudendal artery and nerve pass behind the ischial spine to gain the ischiorectal fossa.
The pudendal nerve crosses the ischiorectal fossa to supply the vulva and perineum.