Chapter 43 Anatomy of the female genital tract
THE VULVA
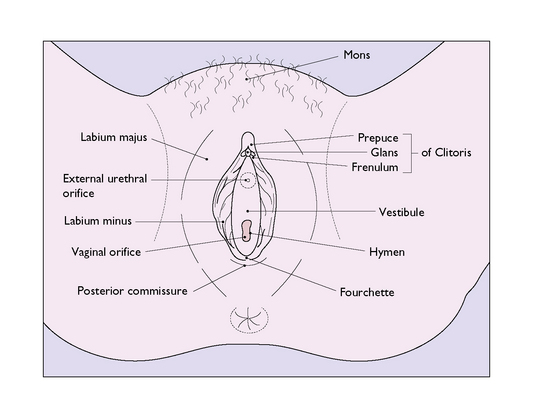
The labia majora are two large folds containing sebaceous and sweat glands embedded in adipose and connective tissue and covered by skin (Fig. 43.1). They form the lateral boundaries of the vulval cleft and are the homologues of the scrotum. Anteriorly, they unite in an adipose pad over the symphysis pubis to form the mons veneris. In the adult the mons is covered with hair, which terminates cephalically in a horizontal upper border. Hair also grows on the outer – but not the inner – surface of the labia majora. Posteriorly, the labia majora unite to form the posterior commissure. In childhood the labia majora contain little adipose tissue, and in older age the adipose tissue disappears. At the extremes of life, therefore, the labia majora are relatively small.
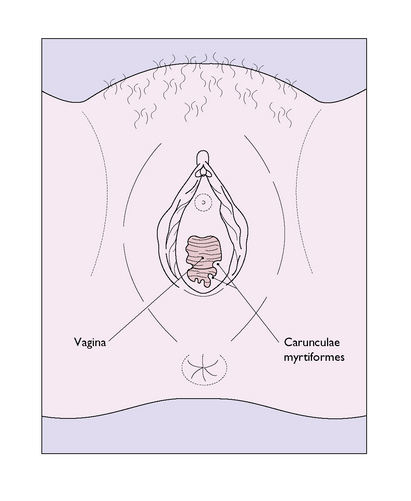
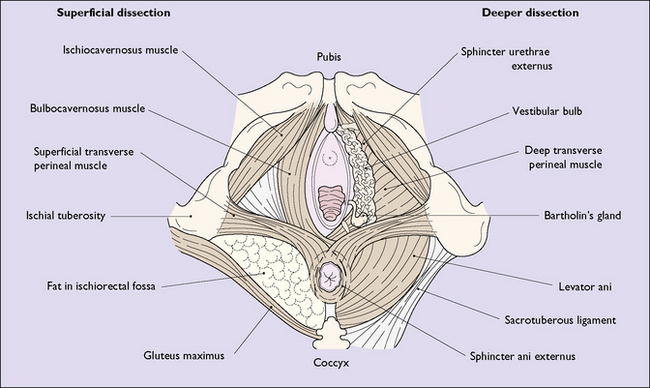
The hymen is a thin, incomplete membrane surrounding the vaginal orifice, and has one or more apertures in it that allow menstrual blood to escape. The apertures are of various shapes and sizes and the hymen varies considerably in elasticity, but is generally torn during a first coitus. An ‘intact’ hymen is considered a sign of virginity, but this is not reliable as in some cases coitus fails to cause a tear, and in others the hymen may be torn by digital interference. In attempting to make a decision regarding virginity, palpation to feel a circular ridge of hymenal tissue is more accurate than inspection. Although the hymen is relatively avascular, tearing at first coitus may be accompanied by a small amount of bleeding, which ceases rapidly. Childbirth causes a much greater tearing of the hymen, and after parturition only a few tags remain. These are known as carunculae myrtiformes (Fig. 43.2). Just lateral to the hymen, surrounding the vaginal orifice on each side and deep to the bulbocavernosus muscle (the sphincter vaginae), are two collections of erectile tissue – the vestibular bulbs. Embedded in the posterolateral parts of the bulbs on each side is Bartholin’s gland (Fig. 43.3), which is the homologue of Cowper’s gland in the male. The gland is pea-sized and not palpable unless infected. It is connected to the posterior part of the vestibule, between the hymen and the fourchette, by a duct some 2 cm in length. It is lined by columnar cells, which secrete a mucoid substance during sexual excitement.
Vascular and nerve supply
Arteries
The external genitalia are very vascular and are supplied by branches of the internal pudendal arteries, which originate from the internal iliac arteries, and by the external pudendal arteries, deriving from the femoral arteries (Fig. 8.23).
Lymphatics
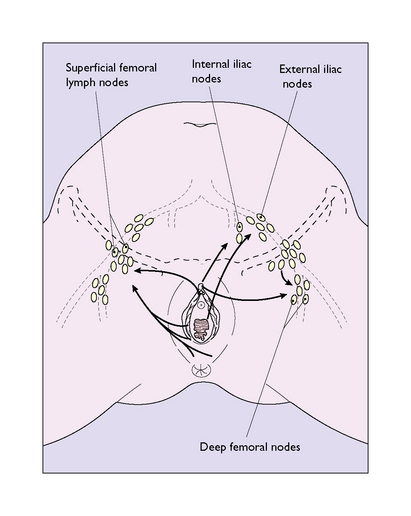
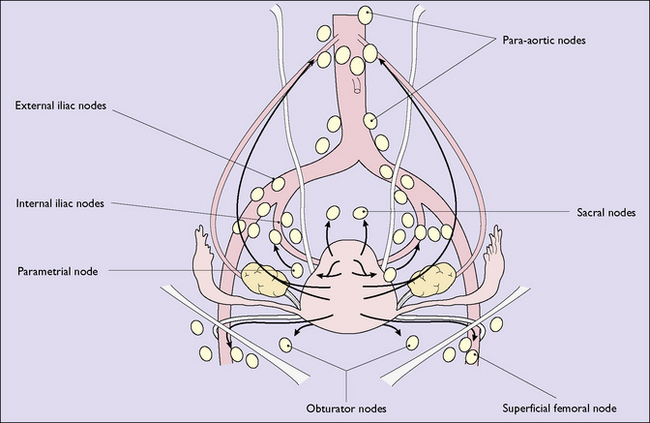
The lymphatics from the clitoral shaft (which interconnect with those of the glans) pass directly to internal iliac nodes in the pelvis (Fig. 43.4). The lymphatics anastomose with those of the opposite side, and consequently bilateral or contralateral involvement is not uncommon in malignant tumours of the vulva. The vulval lymphatics also anastomose with the lymphatics of the lower third of the vagina, which drain into the external iliac nodes.
PELVIC FLOOR
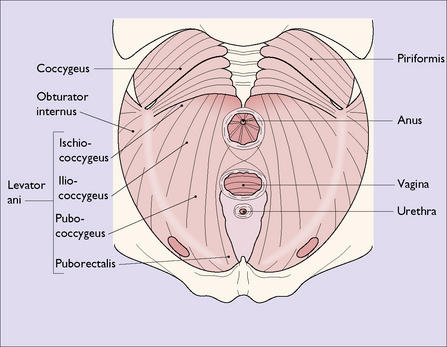
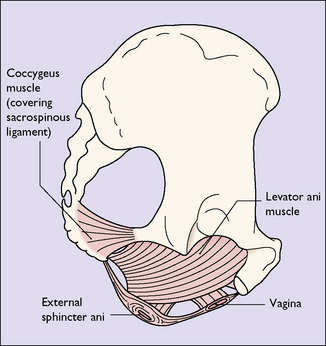
The pelvic floor consists of the levator ani group of muscles, which arise on each side of the pelvis, (i) from the posterior surface of the pubis, (ii) from a condensation of fascia (the white line) which covers the obturator internus muscle, and (iii) from the pelvic aspect of the ischial spine (Fig. 43.5). The muscle has several designated parts, the pubococcygeus muscle, the levator ani muscle and the coccygeus muscle (Fig. 43.6). The fibres of these muscles slope downwards and forwards and interdigitate with muscle fibres of the opposite levator ani group to form a muscular sling through which the urethra, the vagina and the rectum pass. The muscles enclosed in fascia form the pelvic diaphragm (Fig. 43.7).
Perineum
The perineum (perineal body) is the tissue that lies distal to the pelvic diaphragm. It is pyramid shaped and is bounded superiorly by the lower surface of the pelvic diaphragm; laterally by the bones and ligaments of the pelvic outlet; and below by the vulva and the anus. It can be subdivided into the urogenital triangle anteriorly and the anal triangle posteriorly by the transverse perineal muscles (Fig. 43.8). The perineum contains a number of superficial muscles, is very vascular and is filled with fatty tissue. Its importance in childbirth is that it is frequently damaged as the fetus is born.
THE VAGINA
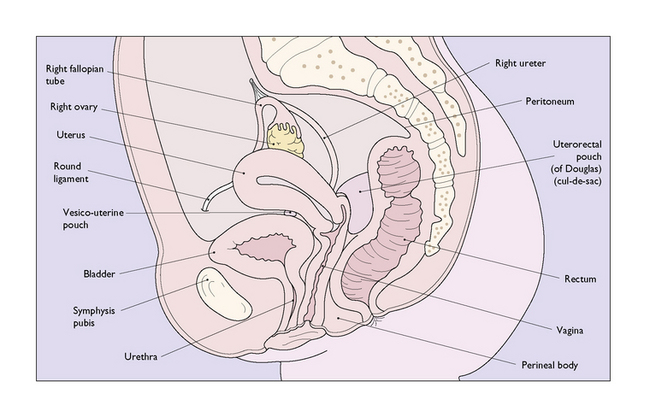
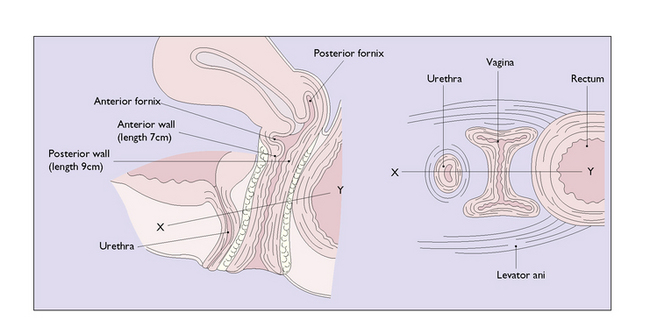
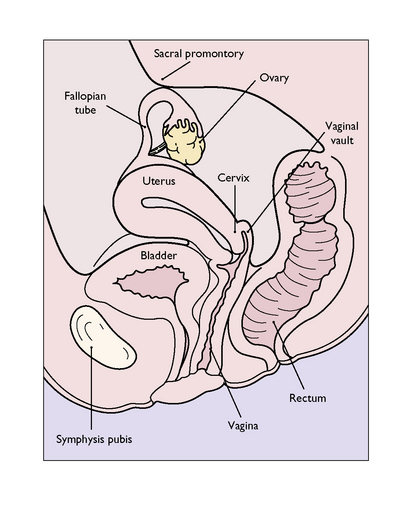
The vagina is a fibromuscular sheath extending upwards and backwards from the vestibule, at an angle of about 85° to the horizontal, and parallel with the plane of the pelvic brim when the woman is standing erect (Fig. 43.9). The walls of the vagina, as well as being muscular, contain a well-developed venous plexus. Normally the walls are in apposition, the vagina being a potential cavity and having an H-shape in cross-section in the middle third (Fig. 43.10). In the lower third the widest diameter of the vagina is the anteroposterior, but above this the widest diameter is the transverse. Knowledge of this is important when introducing a vaginal bivalve speculum. Because of the well-developed walls, the lining epithelium tends to be lifted into ridges, or rugae, which run in a circumferential manner from two longitudinal columns running sagittally the length of the anterior and posterior vaginal walls. The formation of rugae in this manner permits the great distension without damage of which the vagina is capable. The length of the anterior vaginal wall is about 7 cm, and its upper end is invaginated by the cervix. Because of this, the posterior vaginal wall, which ends blindly, is about 2 cm longer. The vaginal vault is divided into four areas, which are related to the projecting cervix. These are the shallow anterior fornix, the capacious posterior fornix and the shallow lateral fornices (Fig 43.10). Although the vagina varies considerably in length and width, its functional size is largely determined by the tone in its muscular wall and the contractions of the surrounding muscles. These are under voluntary control. Unless the vagina has been injured or shortened at operation, anatomical variations in size do not cause difficulty or pain (dyspareunia) during coitus; most cases of dyspareunia are psychosomatic in origin.
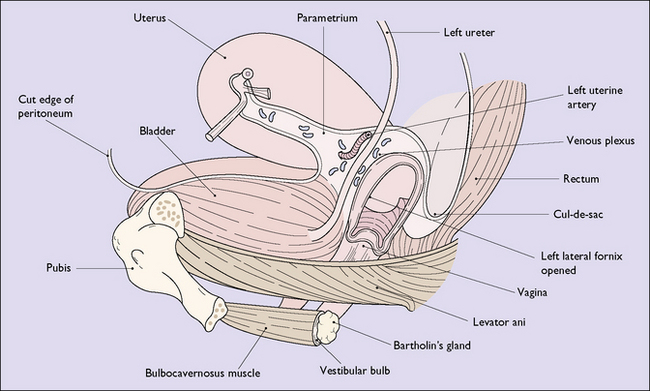
The vagina is surrounded by several important structures. The anterior wall is in contact with the urethra, to which it is closely bound, and above this with the base of the bladder. Posteriorly, the lower third is separated from the rectum by the complex of muscles and fascia that constitutes the perineal body but, above, is in direct contact with the rectum. The upper one-quarter, including the posterior fornix, is covered by the peritoneum of the uterorectal pouch (pouch of Douglas, or cul-de-sac). The upper third of the lateral walls are in intimate contact with the pelvic connective tissue, and the fornices abut the parametrium, which contains a rich venous plexus. Lying about 1 cm above each lateral fornix are the uterine artery and the ureter (Fig. 43.11). In the middle third the lateral wall blends with the levator ani muscles, which together with the muscular vagina form one of the supports of the uterus. In the lower third the walls are related to the bulbocavernosus muscle, the bulb of the vestibule and Bartholin’s glands.
Histology
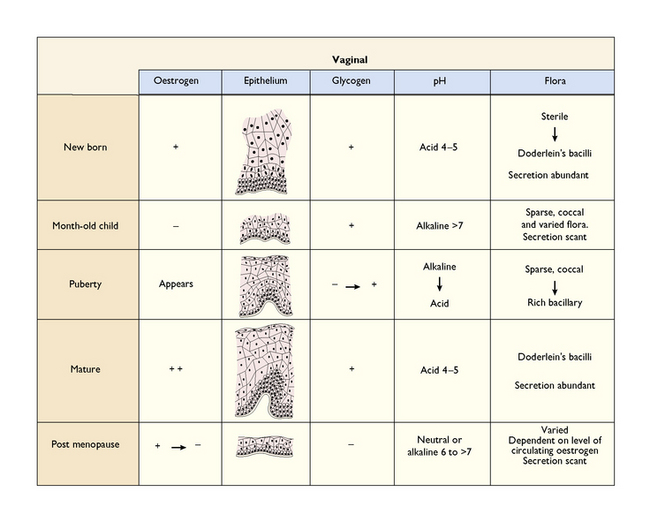
The vagina is lined with stratified, squamous, non-keratinized epithelium, some 10–30 cells deep, which rests upon a basement membrane and is continuous at the upper end with an identical epithelium covering the vaginal portion of the cervix. Should the epithelium be exposed to the dry external atmosphere, keratinization occurs. The cells are all derived by differentiation from the basal cells that lie upon the basement membrane. Three main cell types are described: parabasal, intermediate and superficial. The superficial cells and some intermediate cells contain glycogen. The entire epithelium shows cyclic changes during the menstrual cycle and in pregnancy, and cellular development and differentiation are controlled by the ratio of circulating oestrogens, progesterone and androgens (Fig. 43.12). The cells do not secrete mucus, but secretions seep between the cells to moisten the vagina, and the superficial cells are constantly exfoliated. The exfoliated cells release the contained glycogen, which is acted upon by Döderlein’s bacilli, a normal inhabitant of the vagina, to produce lactic acid. This causes the normal acidity of the vagina and explains the relative resistance of the vagina to infection. The vaginal epithelial cells can also absorb drugs, particularly oestrogens.
Vascular connections
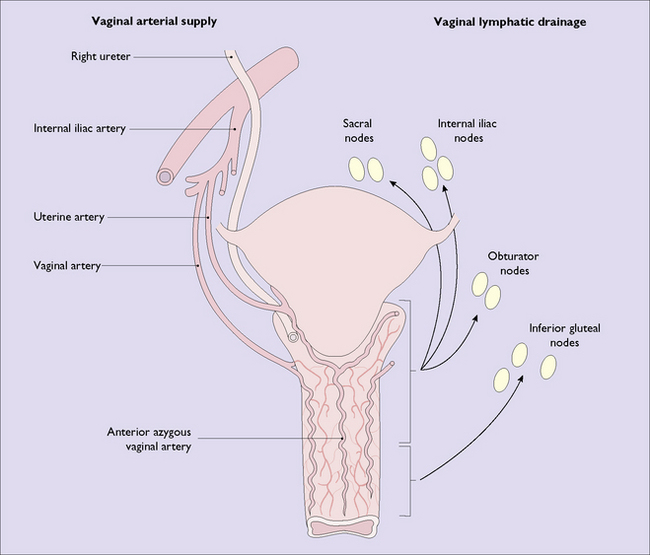
The arterial blood supply is from the vaginal and uterine arteries, which are branches of the internal iliac artery and which form a plexus around the vagina. A median artery arises from this plexus on the anterior and on the posterior walls. These are called azygous vaginal arteries (Fig. 43.13). The venous drainage, which goes to the internal iliac veins, is from a rich venous plexus situated on the muscular wall of the vagina, which is especially well developed at the lower end of the vagina and which communicates with the vesical, pudendal and haemorrhoidal venous plexuses.
THE UTERUS
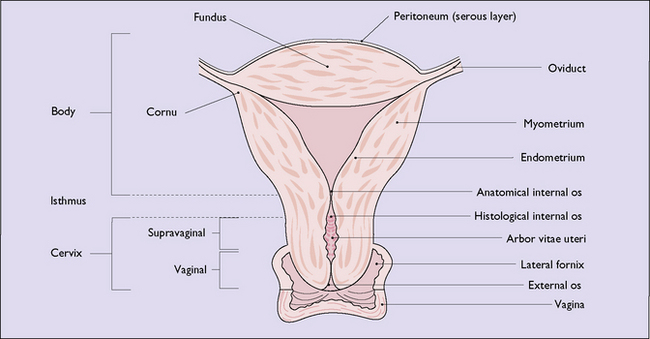
The uterus is a thick-walled, hollow muscular organ shaped like a pear, its apex forming the cervix, which projects into the vaginal vault (Fig. 43.14). It is located in the middle of the true pelvis, lying between the bladder and the rectum. It is flattened from before backwards, and its muscular anterior and posterior walls bulge into the cavity, the walls thus being in apposition. Viewed from the front, the cavity is triangular in shape. It communicates with the peritoneal cavity via the fallopian tubes (or oviducts) above, and with the exterior via the vaginal tube below. The uterus varies in size, being largest during the reproductive years and in women who have had children. The ‘average’ uterus of a nulliparous woman measures about 9 cm in length, 6 cm in width at its widest part and 4 cm from before backwards, and weighs 40–60 g. The wall is 1–2 cm thick, and hence the length of the cavity measures about 7 cm. All these dimensions are increased by about 1.5 cm in women who have borne children.
Structure
The uterus is made up of a body, or corpus, an isthmus and a cervix (Fig. 43.15). The body is further divided into the area that lies above the insertion of the oviducts, and which is called the fundus. The area where the oviducts join the uterus on each side is termed the cornu. The body (including the fundus) comprises the greater portion of the organ, and is formed of thick bundles of muscle. The isthmus is a constricted annular area about 0.5 cm wide, which lies between the corpus and the cervix. The proportion of muscle begins to diminish in the isthmus, and connective tissue appears in increasing amounts. The constriction at the upper end of the isthmus is called the anatomical internal os, and the line at the lower end, where the endometrium changes into columnar cervical epithelium, is termed the histological internal os.On the surface of the uterus the anatomical internal os is marked by the reflection of the peritoneum, which covers the uterus, onto the superior surface of the bladder.
The cervix is fusiform or cylindrical in shape and measures about 3 cm from above downwards, half projecting into the vagina. The proportion of muscle tissue decreases rapidly in the cervix, and in its midportion only 10% of its bulk is made of muscle, the rest being connective tissue. The supravaginal portion of the cervix is surrounded by pelvic fascia, termed the parametrium, except posteriorly, where it is covered with the peritoneum of the uterorectal pouch. The vaginal portion of the cervix is cone shaped and projects into the vagina (see Fig. 43.15). It is covered with stratified squamous epithelium, which joins the columnar epithelium of the cervical canal at or near the external os. The cervical canal is spindle shaped and connects the cavity of the uterus to the vaginal cavity (see Fig. 43.15). The mucous membrane lining the canal is thrown up into anterior and posterior folds, from which circular folds radiate to give the appearance of a tree-trunk and branches. The folds are given the name arbor vitae uteri. The epithelium dips into the underlying stroma in a complicated system of clefts and crypts. The endocervical epithelium consists of columnar cells which secrete mucus, but the quality and quantity of this are under the control of the sex hormones.
Relations
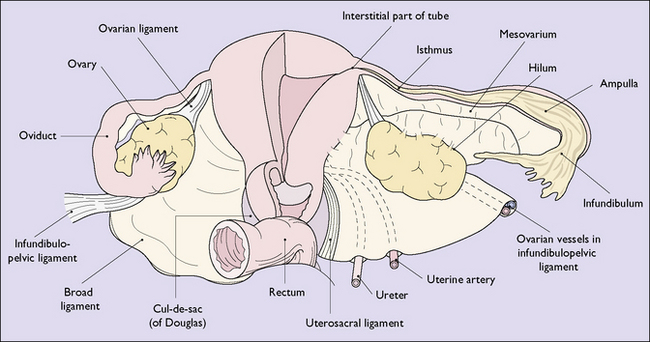
The uterus normally lies bent forward at an angle of 90° to the direction of the vagina, but is freely mobile, rotating about a fulcrum at the level of the supravaginal cervix. Anteriorly, the uterus is separated from the bladder by the vesicouterine pouch, and posteriorly is in contact with coils of bowel and the omentum. The anterior and posterior surfaces are covered with peritoneum, but its narrow lateral surfaces are in direct contact with the broad ligament and, below, with the connective tissue, venous plexuses, arteries, nerves and the ureter, which make up the substance of the parametrium. The peritoneum, which covers the anterior and posterior walls, joins at the lateral margins of the uterus to form the two leaves of the broad ligaments; and these two sheets of peritoneum remain in close proximity, except where they diverge to accommodate the round ligament (more accurately, the round muscle) and the infundibulopelvic ligament. The broad ligament extends from the lateral uterine border to the pelvic wall. Its upper border is formed by the peritoneum covering the oviduct, and below it merges anteriorly with the peritoneum of the pelvic floor, and posteriorly with the peritoneum covering the rectouterine shelf and the uterosacral ligaments (Fig. 43.16).
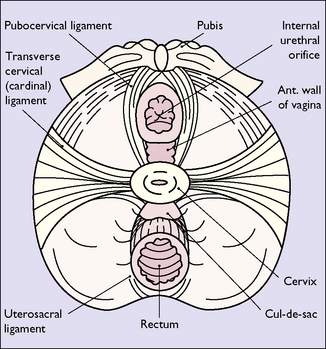
Uterine supports
These are discussed more fully in Chapter 38 and only a summary is presented here. The uterus is supported from below by the muscular vagina and the fibres of the levator ani muscles, which interdigitate with the middle third of the muscular vaginal sheath. An additional support of great significance is the collection of connective tissue, muscular-walled blood vessels and areolar tissue that forms a fan-shaped sheet on each side of the supravaginal cervix, and stretches from the fascia lining the pelvic wall to join the fibromuscular cervix. This fan-shaped sheet is condensed posteriorly to form the uterosacral ligaments, and medially to form the cardinal ligament, or the transverse cervical ligament (Fig. 43.17). Anteriorly, the fascia sweeps forward down the anterior wall of the vagina beneath the bladder base. This condensation is called the pubocervical fascia. Laterally, the broad ligament has a steadying effect on the uterus, and the round ligaments play a minor part in keeping the uterus in an anteverted position.
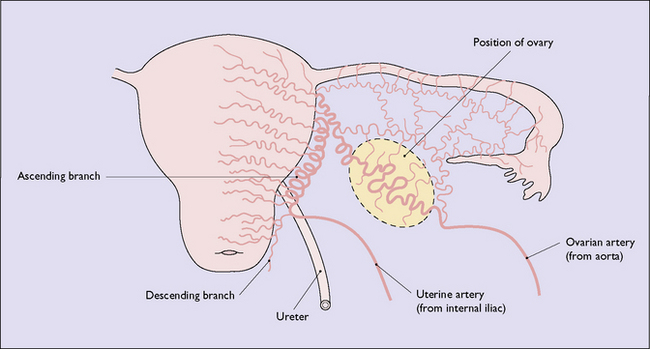
Vascular connections
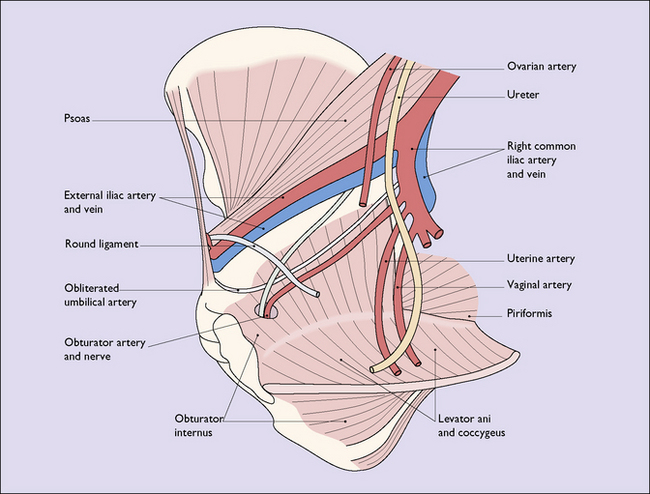
The uterus is supplied by the uterine arteries, which arise from the internal iliac artery. Each vessel runs forwards and inwards in the base of the broad ligament, and crosses the ureter above it and at right-angles to it (‘water under the bridge’), 1 cm lateral to the supravaginal cervix. Each gives off a descending branch which anastomoses with the ascending branches of the vaginal artery, and which supplies the lower cervix; and a circular branch to supply the upper cervix. The main trunk changes direction and passes upwards, coiled and tortuous, between the layers of the broad ligament adjacent to the lateral uterine wall, and supplies branches to the myometrium at intervals. It ends by anastomosing with the ovarian artery (Fig. 43.18). Each branch supplying the uterus divides in the outer muscular layer, to send anterior and posterior branches to the myometrium, and to anastomose with those from the opposite side. These arteries give off branches at right-angles, which penetrate and supply the myometrium and, entering the endometrium, form the basal arteries.
Lymphatic drainage
The lymphatic drainage of the uterus consists of three communicating networks: the deepest lies in the endometrium, the second lies in the substance of the myometrium, and the superficial network is subperitoneal. The networks form collecting trunks, which pass from the corpus between the layers of the broad ligament along with the ovarian lymphatics. These trunks then pass through the infundibulopelvic fold, and ascend, on the posterior abdominal wall, to join the nodes of the para-aortic group. A few channels pass along the round ligament to the superficial femoral nodes. The lowest two trunks communicate with the collecting trunks from the cervix, which pass through the base of the broad ligament to an inconstant node lateral to the parametrial node, to the nodes along the internal iliac arteries (the internal iliac or hypogastric nodes), and to the obturator nodes anteriorly. A few channels pass backwards along the uterosacral ligaments to the sacral nodes (Fig. 43.19).
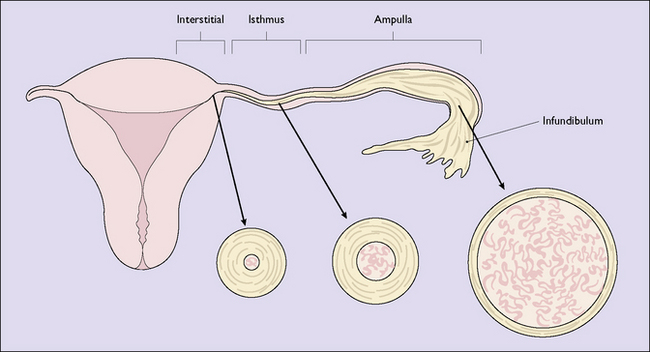
THE OVIDUCTS OR FALLOPIAN TUBES
The oviducts, or Fallopian tubes, are two small muscular tubes, one on each side, which extend for about 10 cm from the uterine cornua towards the pelvic wall, forming the upper border of the broad ligaments. The outer half of each oviduct lies in contact with the ovary, curving over its superior surface to end in the abdominal ostium. Because the tube is hollow, a direct connection exists between the peritoneal cavity and the uterus. The mucous membrane lining of the tube is thrown up into folds which almost obliterate the lumen, and which are prolonged through the abdominal ostium to form the fimbriae of the tube. The oviduct can be divided into four parts. The infundibulum is the outermost portion of the tube. It includes the trumpet-shaped abdominal ostium, and lies in close proximity to the ovary. The ampulla is the longest segment of the oviduct, is normally rather tortuous, and has a relatively thin dilatable wall. The isthmus is a straight, narrow, relatively thick-walled segment, and the interstitial portion is the short, narrow portion within the uterine wall. The size of the lumen decreases from the infundibular to the interstitial portion, where it is only about 1 mm in diameter, whereas the complexity of the folds in the mucous membrane increases from the interstitial to the infundibular portions (Fig. 43.20).
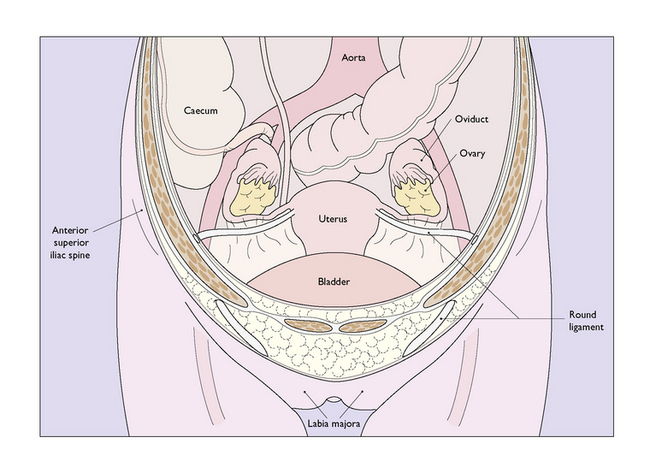
THE OVARY
The two ovaries are the homologues of the testes and are ovoid in shape. Each ovary normally lies in a shallow peritoneal fossa adjacent to the lateral pelvic wall, with its long axis in a vertical plane, but its position is influenced by movements of the uterus and broad ligament (Fig. 43.21). The ovaries have an irregular surface, are pinkish-grey in colour, and vary in size in different women and at different times of the cycle. In the infant, the ovary is a delicate, elongated structure with a smooth, glistening surface. The ovary of a neonate contains little stroma and consists mainly of primordial follicles. As infancy and childhood progress, increasing numbers of follicles degenerate and there is a progressive increase in stromal content, up to puberty. During puberty the ovary enlarges, and in the reproductive period it averages 3.5 cm in length, 2 cm in breadth and 1 cm in thickness, and weighs about 7 g. After the menopause the ovary undergoes rapid regressive changes, becoming wrinkled, white in colour and less than half the size it was in the reproductive era. Each ovary is attached to the posterior leaf of the broad ligament by a fold of peritoneum called the mesovarium, through which pass the ovarian vessels and nerves (see Fig. 43.16). The peritoneum stops where the mesovarium joins the ovary, and this part of the ovary is called the hilum. The remainder of the ovarian cortex is covered by a single layer of low columnar epithelium under which is a layer of connective tissue called the tunica albuginea. This layer increases in density with increasing age.
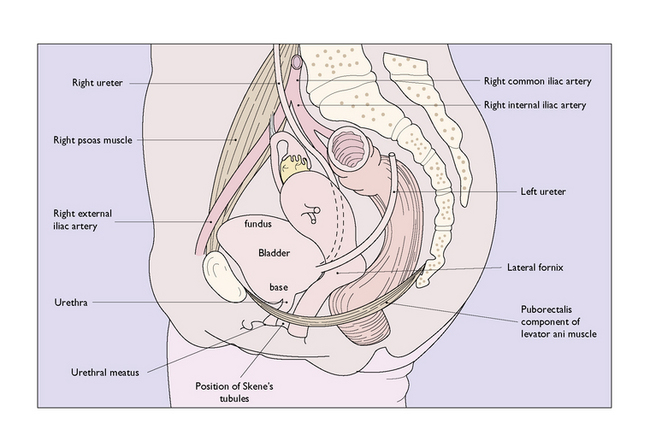
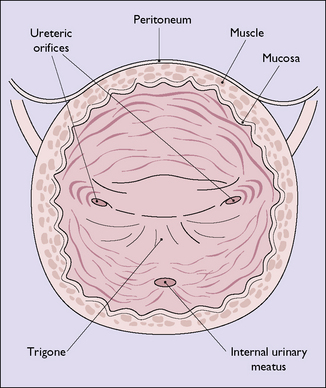
ANATOMY OF THE URINARY TRACT
The bladder is a muscular organ with a considerable capacity for distension. The base is relatively flat, lies parallel with the axis of the vagina, and contains the internal urinary meatus and the orifices of the ureters (Fig. 43.22). The triangular area between these three openings constitutes the trigone. The dome, or fundus, of the bladder varies in shape and position depending upon the degree of distension. It is lined by transitional epithelium, and external to this is the muscular layer. The involuntary muscle that forms the bladder can be divided into two parts, that forming the fundus, which is poorly supplied by autonomic nerves, and that forming the base (the detrusor muscle), which is richly supplied by autonomic nerves. The female urethra is a muscular tube composed of two muscle layers. It is about 4 cm long. The inner layer of muscle is longitudinal and is a direct continuation of the inner longitudinal layer of the detrusor muscle. It is embedded in dense collagen. The outer layer, which is a continuation of the outer layer of the detrusor muscle, is composed of semicircular fibres which never form a complete ring around the urethra. They loop around the urethra, at various degrees of obliquity, turning back to reach the bladder. Collectively they form a thick muscle layer, which encircles the urethra to form a sphincter.
The ureters pass from the renal pelves, behind the peritoneum, lying on the psoas muscle, to enter the true pelvis anterior to the sacroiliac joint. They are separated from the joint by the ligaments of the joint, the psoas muscle and the common iliac vessels, and enter the pelvis in front of the common iliac artery at its bifurcation into the external and internal branches. Inside the true pelvis, each ureter turns downward and runs on the medial side of the internal iliac artery. In the parametrium, as it courses forward to the bladder, it is crossed by the uterine artery, and lies 1 cm lateral to the supravaginal cervix and 1 cm above the lateral fornix. It passes obliquely through the bladder wall on the posterior aspect of its base, and the ureteric orifices mark the posterior points of the trigone of the bladder (Fig. 43.23). The ureter is lined with transitional epithelium, and the main coats of its wall consist of involuntary muscle, which constantly moves as peristaltic waves pass along it. The obliquity with which the ureter enters the bladder acts as a valve preventing reflux of urine when the bladder is full.