Anatomy of the Cardiovascular System
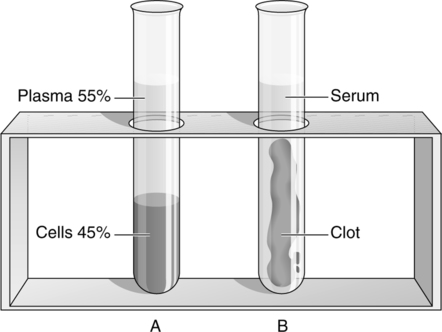
A A heterogeneous substance composed of a fluid (plasma) and a cellular component (Figure 9-1).
B Plasma: Whole blood minus the cellular component.
1. It is a pale yellow (strawlike) color.
2. The three major body fluids are plasma, the interstitial fluid, and the intracellular fluid.
3. Major constituents are water and chemical compounds (solutes).
C Cellular components: Red blood cells (RBCs), white blood cells (WBCs), and platelets are all generated in the red bone marrow from a common stem cell, the hemocytoblast (Figure 9-2).
1. RBCs, also called erythrocytes, are biconcave disks with a diameter of 7 to 8 μm and a thickness of approximately 2 μm.
a. Mature RBCs are anucleated (have no nucleus).
b. A semipermeable membrane surrounds RBCs.
(1) Placed in a hypotonic solution (<0.9% NaCl), they will swell and can rupture (hemolysis).
(2) Placed in a hypertonic solution (>0.9% NaCl), they will shrivel (crenation).
c. RBCs are relatively flexible and are able to accommodate changes in shape without rupturing. This becomes important when they pass through tight and/or irregular spots in the circulation (e.g., capillaries or sinusoids).
d. RBCs are produced in myeloid tissue (red bone marrow), a process termed erythropoiesis.
e. The normal number of RBCs is higher in males than in females.
f. Reticulocytes are newly released RBCs that retain a small portion of the hemoglobin-forming endoplasmic reticulum.
(1) In 2 to 3 days, formation of hemoglobin will be complete. At this point, the endoplasmic reticulum disappears, and the cell is a mature erythrocyte.
(2) The percentage of total RBCs that are reticulocytes indicates the rate of erythropoiesis.
(3) The normal range (percentage) of reticulocytes is 0.5% to 1.5% of the total number of RBCs.
g. Hemoglobin is the major solute contained within the RBC.
h. The hematocrit is the volume percentage of RBCs in whole blood (e.g., a hematocrit equal to 45 means that 45% of whole blood is RBCs by volume) (see Figure 9-1).
i. Normally the RBC count is approximately one third the hemoglobin levels, and the hemoglobin levels are equal to approximately one third of the hematocrit. Hence given a hematocrit of 45%, an approximation of hemoglobin of 15 gm% and an RBC count of 5 million/mm3 is made.
2. WBCs, also called leukocytes, are of the following five types: polymorphonuclear neutrophils, eosinophils, and basophils and mononuclear monocytes and lymphocytes.
a. Polymorphonuclear leukocytes
(1) Are formed in myeloid tissue.
(2) Have a multilobed nucleus.
(3) Are collectively called polys.
(4) Appear histologically to possess granulated cytoplasm and are collectively termed granulocytes.
(5) All can perform phagocytosis.
(6) Polymorphonuclear neutrophils
(1) Are formed in lymphoid tissue.
(a) Have a diameter of 10 to 15 μm.
(b) Have a crescent-shaped nucleus.
(c) Have cytoplasm containing fine granules.
c. Total WBC count has the normal range of 5,000 to 10,000 WBCs/mm3.
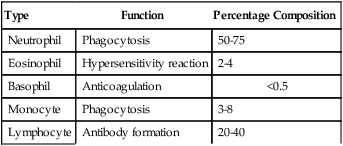
d. A differential count identifies the percentage of the total WBC count that each WBC type comprises (Table 9-1). (Note normal range [percent] in each of the WBC types previously described.)
TABLE 9-1
Normal Function and Percentage Composition of Leukocytes
| Type | Function | Percentage Composition |
| Neutrophil | Phagocytosis | 50-75 |
| Eosinophil | Hypersensitivity reaction | 2-4 |
| Basophil | Anticoagulation | <0.5 |
| Monocyte | Phagocytosis | 3-8 |
| Lymphocyte | Antibody formation | 20-40 |
D Total blood volume of an individual
1. The total blood volume of an individual is equal to approximately 60 to 80 ml of blood/kg of body weight, which is equal to approximately 5 L in a normal man.
2. This relationship varies inversely with the amount of excess body fat; in other words, an obese individual has less blood volume per kilogram than a slender individual and vice versa.
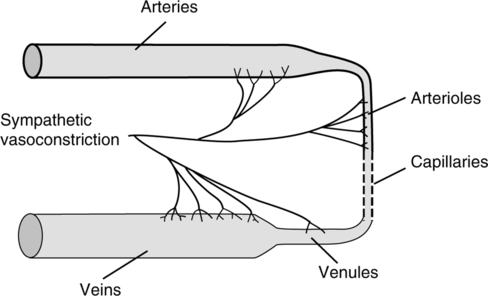
II The Blood Vessels (Figure 9-3)
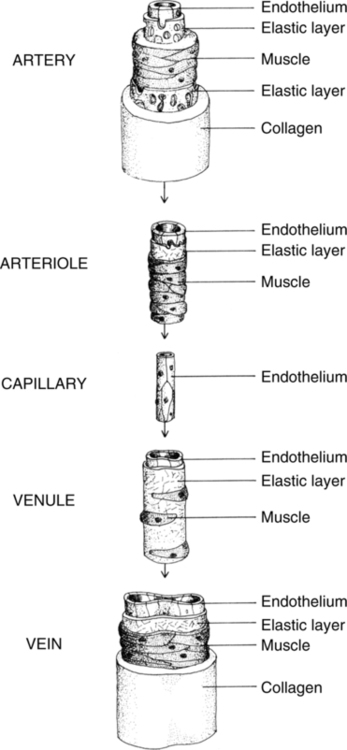
A The blood vessels consist of a closed system of connected arteries, arterioles, capillaries, venules, and veins.
B Arteries contain three characteristic layers: tunica adventitia, tunica media, and tunica intima.
1. Tunica adventitia (external layer)
a. It consists of connective tissue surrounding a network of collagenous and elastic fibers.
b. It supports and protects the blood vessels.
c. It contains vasa vasorum, fine vessels that serve the tunica adventitia with its blood supply.
2. Tunica media (middle layer)
a. It is the thickest layer of the artery.
b. It is composed of concentrically arranged smooth muscle and elastic fibers.
c. Nerve fibers contained in tunica adventitia terminate in the smooth muscle layer of the tunica media.
3. Tunica intima (internal layer)
a. It is the thinnest layer of the artery.
b. It consists of a flat layer of simple squamous cells called the endothelium:
(1) A fine layer of connective tissue supports the endothelium.
(2) A longitudinally placed network of elastic fibers surrounds the connective tissue.
c. Common to all blood vessels, the endothelium is even continuous with the endocardium of the heart, providing a smooth containment for blood travel.
C Large arteries: Termed elastic arteries because the tunica media has less smooth muscle and more elastic fibers.
D Medium-sized arteries: Sometimes called nutrient arteries because they control the flow of blood to various regional areas of the body. Their ability to regulate blood flow lies in a tunica media, which is composed almost entirely of smooth muscle.
1. The arterioles have a thin tunica intima and adventitia but have a thick, smooth muscle layer in the tunica media.
2. The arterioles range in diameter from 20 to 50 μm.
3. The tunica media is extensively innervated by postsynaptic sympathetic nerve fibers (Figure 9-4).
4. Because of the extensive innervation and abundance of smooth muscle, the arterioles control local blood flow to the capillary beds.
5. The arterioles are frequently called the resistance vessels. By vasomotion, they control the rate of arterial runoff (the rate at which blood leaves the arterial tree) and thereby arterial blood volume and, to a great extent, blood pressure.
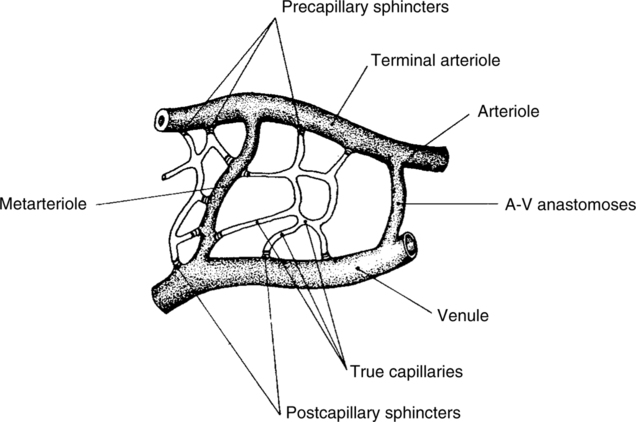
6. The arterioles terminate in either metarterioles or capillaries.
1. Capillaries consist only of tunica intima.
2. They vary in diameter from 5 to 10 μm.
3. Where capillaries originate from arterioles or metarterioles, there frequently is a small band of smooth muscle called the precapillary sphincter.
a. This sphincter controls blood flow through the distal capillary.
b. It is responsive (vasoactive) to local Pco2, Po2, pH, and temperature.
4. Capillaries frequently are called exchange vessels because they are the site of gas, fluid, nutrient, and waste exchange (Figure 9-5).
a. An intracellular cleft lies between the individual squames comprising the endothelium.
(1) They are approximately 50 to 60 Å wide.
(2) They act as pores through which substances can move into and out of the capillaries.
b. The basement membrane usually is continuous in the capillaries and may limit movement of substances into and out of the capillaries.
G Veins consist of a tunica adventitia, media, and intima, but each layer is thinner than its counterpart in the arteries.
a. Is one to five times as thick as the tunica media.
b. Is made up of connective, elastic, and smooth muscle tissue.
a. Is made up of concentrically arranged smooth muscle, collagenous, and elastic tissue.
b. Is innervated by postsynaptic fibers of the sympathetic nervous system (see Figure 9-4).
H All vessels of the venous system generally have smaller amounts of elastic and smooth muscle tissue than their arterial counterparts.
I Venules (small veins) have the three characteristic layers, but they are thin and almost indistinguishable.
J Veins are called capacitance vessels, or reservoir vessels, because 70% to 75% of the blood volume exists in the venous system.
K Veins contained in the periphery of the body contain one-way valves (Figure 9-6).
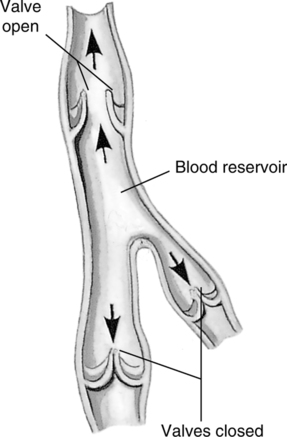
1. Valves are formed by duplication of endothelial lining of veins.
2. Valves are semilunar and prevent retrograde flow of blood.
3. Valves are found in veins >2 mm in diameter and exist in areas subjected to muscular pressure (e.g., arms and legs).
4. Valves are absent in veins <1 mm in diameter and in areas such as the abdominal and thoracic cavities.
A These vessels are a type of circulatory system that collects fluid, protein, lipids, and other material in the interstitial space and returns them to the venous vasculature.
B Lymphatic vessels originate as blindly ending vessels called lymphatic capillaries.
1. They have no basement membrane and consist only of loosely fitting endothelial cells.
2. They are invested in every tissue of the body except for cartilage, bone, and epithelium and are importantly absent in the central nervous system.
C Lymphatic capillaries drain into larger lymphatic vessels, which take on three characteristic layers similar to those of the veins.
1. Larger lymphatic channels contain smooth muscle, elastic, fibrous, and connective tissue.
2. These vessels resemble the veins except that the three layers composing the lymphatic vessels are thinner and less developed.
3. One-way semilunar valves are found approximately every millimeter and are more frequent in the lymphatic vessels than in the veins.
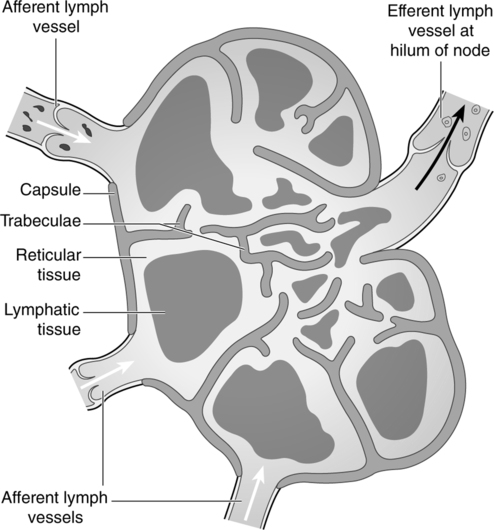
D The larger lymphatic vessels drain into lymph nodes (Figure 9-7).
1. Lymph nodes are found in the neck, axilla, groin, thorax, breast, arms, and mouth.
2. Lymph nodes are bean or oval shaped.
3. Lymph moves into the lymph nodes via afferent lymphatic channels.
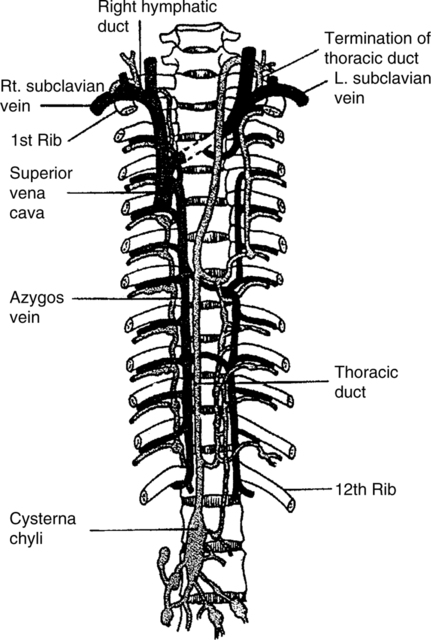
E The large efferent lymphatic vessels join one of two major lymphatic ducts, either the right lymphatic duct or the thoracic duct (Figure 9-8):
a. Drains right upper quadrant of the trunk.
b. Drains right side of the head and neck.
F Total lymphatic flow varies from 2 to 4 L/day, an amount roughly equal to the total plasma volume. This suggests that 50% to 100% of the plasma fluid volume leaves the vascular proper daily and is ultimately returned to the venous circulation.
G Having no true pump to create lymphatic flow, the lymphatic system depends on the contraction of skeletal muscle, intrathoracic pressure changes, and the pulsation of neighboring arteries to assist the movement of lymph.
A The heart is a muscular pump that maintains circulation of the blood through the vessels to all parts of the body.
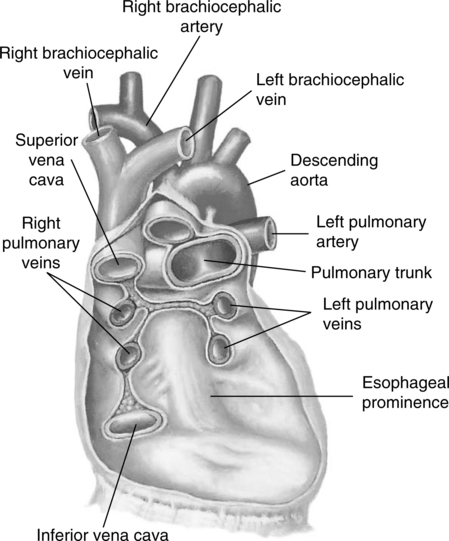
B The heart is located between the lungs in the mediastinum (Figure 9-9).

C The apex is the inferior portion of the heart and is directed inferiorly, anteriorly, and to the left, with the majority of it located left of the midline.
D The base is the superior aspect of the heart.
E The heart is approximately the size of the clenched fist.
F A loose nondistensible sac called the pericardium encases the heart (Figure 9-10).
G Layers of pericardium (Figure 9-11)
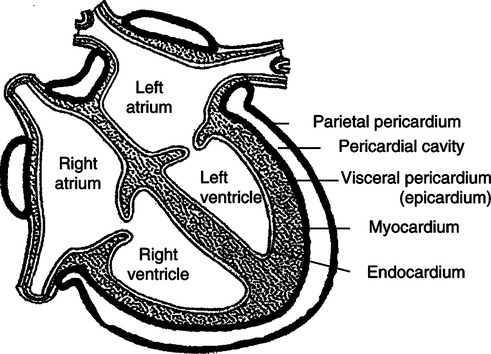
a. Is the outermost layer of pericardium.
b. Attaches to the great vessels (major vessels entering and exiting from the heart) of the heart and loosely encases the heart proper.
c. Is made of white fibrous tissue that protects and anchors the heart to some extent.
d. Is externally attached to the sternum, vertebral column, central tendon, and left hemidiaphragm.
2. Parietal serous pericardium
a. Lines the fibrous pericardium, to which it is closely adherent.
b. A moist serous membrane that forms a smooth surface to reduce frictional resistances.
c. Produces a small volume of serous fluid called pericardial fluid.
3. Visceral serous pericardium
a. The visceral serous pericardium is directly adherent to the heart.
b. It is also known as the epicardium of the heart.
c. It is a serous membrane that produces serous pericardial fluid.
d. The small space between visceral and parietal serous pericardial layers is called the pericardial space.
4. The fact that the visceral and parietal serous pericardial layers are smooth membranes with a small volume of lubricating pericardial fluid between them allows the heart to move freely in the pericardial sac opposed by reduced frictional forces.
5. Abnormal fluid and/or blood accumulation in the pericardial space may impede normal filling of the heart and hence compromise cardiac output, a condition called cardiac tamponade.
H The heart wall has three distinctive layers (see Figure 9-11):
1. Epicardium, or visceral serous pericardium
a. Is the most superficial layer.
b. Is a transparent serous sheet lying on a delicate network of connective tissue.
c. Contains fat, coronary blood vessels, and coronary nerves, which are observable on the cardiac surface.
I The heart has four chambers (Figure 9-12).
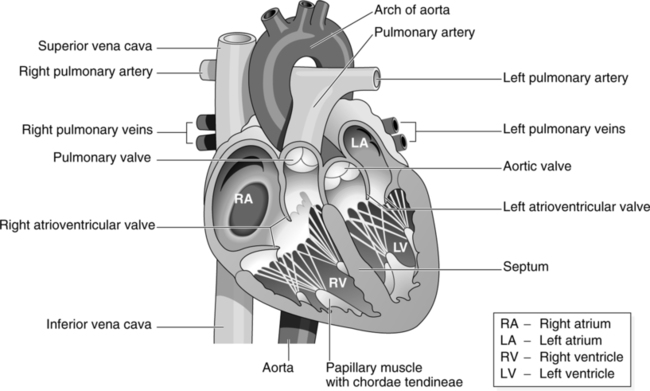
1. It has two superior chambers, or atria.
2. It has two inferior chambers, or ventricles.
3. Externally the two atria are separated from the two ventricles by a groove that circumscribes the heart, the coronary sulcus.
4. The roots of the aorta and the pulmonary artery externally separate the two atria from each other.
5. Externally the two ventricles are separated from each other by a groove, the interventricular sulcus.
6. A wall, the interatrial septum, internally separates the two atria from each other.
a. The fossa ovalis, a depression in the atrial septal wall, is the remnant of the fetal foramen ovale.
7. Internally the two ventricles are separated from each other by a fibrous and muscular interventricular septum. It is continuous with the interatrial septum through its fibrous portion (see Figures 9-11 and 9-12).
8. Internally the atria are separated from the ventricles by a structure known as the fibroskeleton of the heart (Figure 9-13).
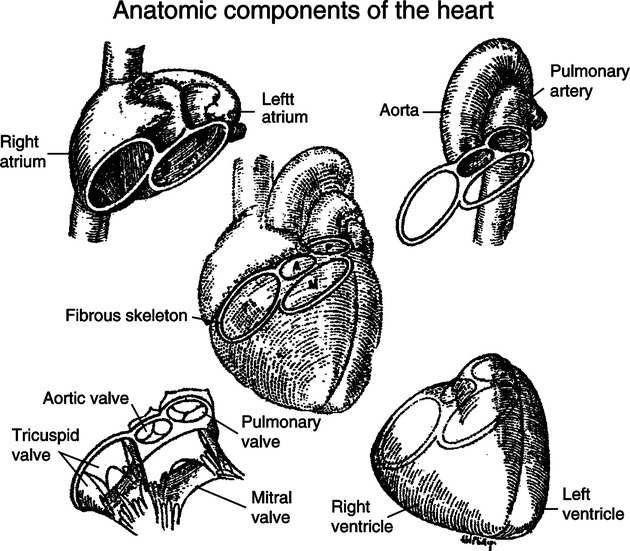
a. The fibroskeleton consists of fibrous rings (which surround the two atrioventricular [AV] cardiac valves, the pulmonic semilunar and aortic semilunar valves), fibrous interventricular septum, right and left trigone, and tendon of conus.
(1) The right fibrous trigone consists of fibrous tissue that connects the two AV rings, fibrous interventricular septum, and ring of the aortic semilunar valve.
(2) The left fibrous trigone consists of fibrous tissue that connects the fibrous ring of the left AV valve with the aortic semilunar valve.
(3) The tendon of conus is fibrous tissue that connects the fibrous ring of the pulmonic semilunar valve with the ring surrounding the aortic semilunar valve.
9. The right atrium is positioned atop the right ventricle (Figure 9-14).
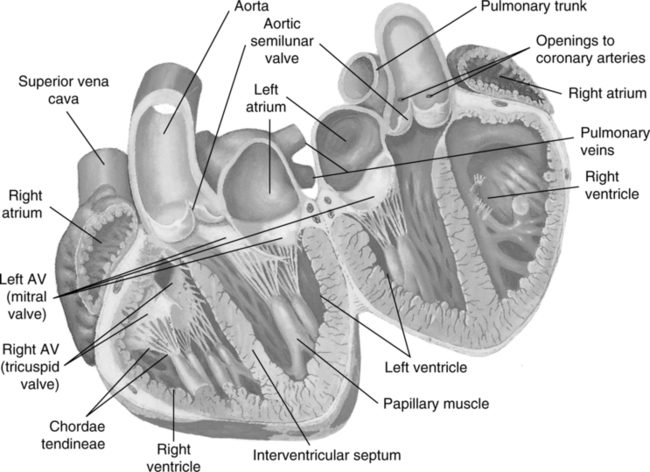
a. It is anterior to the left atrium because the heart is rotated to the left.
(1) Thus the bulk of the anterior surface of the heart is composed of the right side of the heart (i.e., right atrium and ventricle).
(2) Most of the posterior surface of the heart is composed of the left side of the heart (i.e., left atrium and ventricle).
b. The right atrium is larger than the left atrium and has a thinner wall.
(1) The right atrial wall is approximately 2 mm thick.
(2) The atrial musculature is divided into deep atrial muscle, which encircles each atrium individually, and superficial atrial muscle, which encircles both atria.
(3) The deep and superficial muscle fibers run perpendicularly to one another and originate and insert on the fibroskeleton of the heart.
(4) Therefore contraction of the two major groups of atrial muscle fibers tends to decrease the size of the respective atria in all dimensions.
c. The cavity of the right atrium consists of two parts:
(1) The major cavity of the right atrium, or sinus venarum.
(2) The smaller cavity, which appears externally as a pouch, called the right auricle. (Note: Auricle is a term formerly used to denote the entire atrium.)
d. The right atrium accepts venous blood from the following veins:
(1) The superior vena cava, which opens into the superior and posterior portions of the major cavity of the right atrium.
(2) The inferior vena cava, which opens into the most inferior portion of the right atrium near the interatrial septal wall.
(3) The coronary sinus (of the coronary circulation), which opens into the right atrium between the tricuspid valve and the opening of the inferior vena cava.
10. The left atrium is positioned atop the left ventricle (see Figure 9-14).
a. The left atrium is smaller than the right atrium and has a thicker wall.
(1) The left atrial wall is approximately 3 mm thick.
(2) The left atrial muscle fibers are divided into deep and superficial muscle groups and have an arrangement similar to that of the right atrium.
b. The cavity of the left atrium consists of two parts:
(1) The major cavity of the left atrium.
(2) The left auricle, which appears externally as a pouchlike structure.
c. The left atrium accepts arterial blood from the four pulmonary veins, which open into its superior and posterior aspects.
11. Right ventricle (see Figure 9-14).
a. It constitutes most of the anterior surface of heart.
b. The right ventricular wall is one third the thickness of the left ventricular wall.
c. The ventricular musculature is classically separated into superficial and deep muscle groups.
(1) Superficial and deep muscle groups appear to originate on the fibroskeleton of the heart.
(2) Superficial fibers follow a clockwise spiral course to the apex of the heart. At the apex, these fibers turn inward and follow a spiraled course counterclockwise and upward toward the base of the heart to insert on the fibroskeleton.
(3) Deep fibers follow a similar course to the superficial ventricular fibers, with three exceptions:
(a) The spiraled course of the deep fibers is in a direction opposite to that of the superficial fibers.
(b) Deep fibers may not follow a course all the way to the apex of the heart before starting to ascend.
(c) Deep fibers may insert into the cardiac fibroskeleton, papillary muscles, or trabeculae carneae.
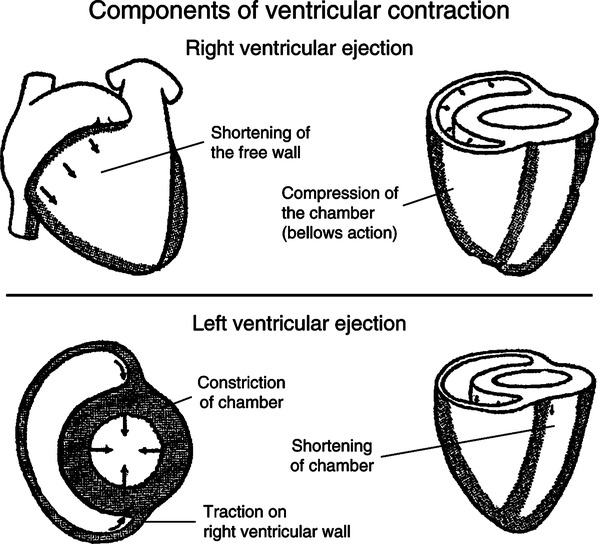
(4) Contraction of ventricular muscle fibers tends to decrease the internal anteroposterior and transverse diameters significantly but leaves the vertical diameter virtually unchanged (Figure 9-15).
d. The right ventricle receives venous blood from the right atrium through an opening called the right AV orifice.
(1) A fibrous ring that is a part of the cardiac fibroskeleton surrounds this orifice.
(2) The right AV orifice is approximately 4 cm in diameter.
(3) The right AV orifice contains the tricuspid valve.
(a) The tricuspid valve contains three cusps, each fused at its origin in the circumference of the AV ring.
(b) The cusps are formed by a duplication of the endocardial layer of the heart and are supported with fibrous tissue.
(c) The three cusps collectively have a funnel shape that projects into the cavity of the right ventricle.
(d) The free borders (inferior border) of each cusp have an attached fibrous cordlike structure, the chordae tendineae.
(e) The chordae tendineae are in turn attached to the intraventricular papillary muscles.
(f) The chordae tendineae commonly cross, passing from one of the cusps to a group of papillary muscles on the opposite side of the ventricle.
e. The cavity of the right ventricle is lined with muscular ridges (trabeculae carneae) and papillary muscle covered by endocardium.
(1) The cavity of the right ventricle has a bellows or U shape (see Figure 9-15).
(2) The muscular arrangement and shape of the right ventricle are well suited to its function of pumping blood under low pressure.
f. Blood exits from the cavity of the right ventricle by passing into the pulmonary artery via an opening called the orifice of the pulmonary trunk.
12. Left ventricle (see Figure 9-14)
a. It constitutes most of the posterior surface of the heart.
b. The left ventricular wall is three times the thickness of the right ventricular wall.
c. Left ventricular muscle fibers are part of the continuum of muscle circumscribing both ventricles and cannot be anatomically separated from right ventricular fibers. (Note: The arrangement of the ventricular muscle fibers is described in the foregoing section on the right ventricle.)
d. The left ventricle receives arterial blood from the left atrium through the left AV orifice.
(1) A fibrous ring, which is one of the components of the cardiac fibroskeleton, surrounds this orifice.
(2) Contained in the left AV orifice is the bicuspid or mitral valve.
e. The cavity of the left ventricle is lined with muscular ridges (trabeculae carneae), which appear in a more numerous and dense arrangement than in the right ventricle. The endocardial layer covers the papillary muscles with the corresponding thick chordae tendineae, along with the trabeculae carneae.
(1) The cavity of the left ventricle is conical.
(2) The arrangement of the more developed left ventricular musculature coupled with its conical shape lends well to its function of pumping blood under high pressure (see Figure 9-15).
f. Blood exits from the cavity of the left ventricle into the root of the aorta by passing through the aortic opening.
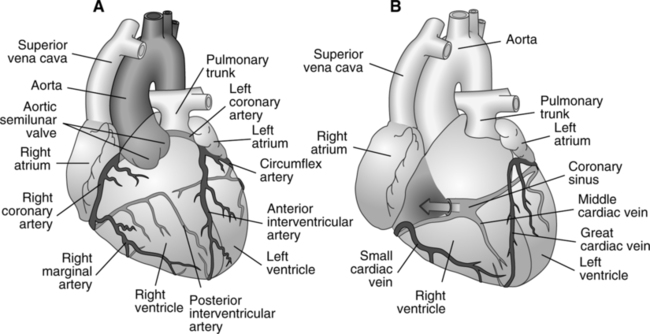
J The coronary circulation (Figure 9-16)
1. Blood supply to the heart is delivered via the right and left coronary arteries, which have their origins in the root of the aorta just distal to the aortic semilunar valve.
a. The right coronary artery bifurcates into the posterior (interventricular) descending and marginal arteries serving the majority of the right side of the heart with its blood supply.
b. The left coronary artery bifurcates into the anterior (interventricular) descending and circumflex arteries serving the majority of the left side of the heart with its blood supply.
c. The aforementioned four arteries divide numerous times over the epicardial layer of the heart and ultimately penetrate the myocardium, giving way to a typical vascular bed and providing the myocardial perfusion.
d. The coronary circulation terminates in the large coronary veins and the anterior cardiac vein that drain into the coronary sinus and right auricle, respectively. The thebesian veins of the coronary circulation empty a minor amount of venous blood directly into the right and left ventricles.
e. It is worth noting that the normal coronary circulation, despite having a significant cardiac distribution, does not possess many anastomoses, hence making the tissue it serves (the myocardium) prone to ischemia and infarction should the local arterial vessels be compromised.