Chapter 79 Analgesics and Antidepressants
4 What are the initial steps in treating salicylate poisoning?
 First, delay and prevent absorption of salicylate. Early initial management of an acute ingestion should include administration of activated charcoal, when possible. Multiple dose activated charcoal may also be considered.
First, delay and prevent absorption of salicylate. Early initial management of an acute ingestion should include administration of activated charcoal, when possible. Multiple dose activated charcoal may also be considered.
 Patients should also be resuscitated.
Patients should also be resuscitated.
 Patients with moderate or severe poisoning are typically volume depleted, and intravenous fluids should be administered via bolus.
Patients with moderate or severe poisoning are typically volume depleted, and intravenous fluids should be administered via bolus.
 It is important to remember that salicylate-poisoned patients have a very high minute ventilation, both from primary respiratory alkalosis and to compensate for metabolic acidosis. Physicians must be especially cautious in administering sedation or initiating mechanical ventilation so as not to worsen acidosis.
It is important to remember that salicylate-poisoned patients have a very high minute ventilation, both from primary respiratory alkalosis and to compensate for metabolic acidosis. Physicians must be especially cautious in administering sedation or initiating mechanical ventilation so as not to worsen acidosis.
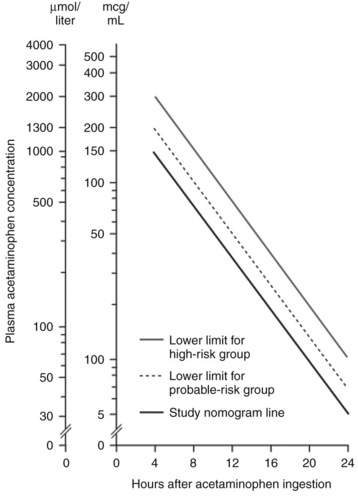
10 How is the Rumack-Matthew acetaminophen treatment nomogram used?
The Rumack-Matthew treatment nomogram is used to identify patients who have taken a single, acute acetaminophen overdose and who are at risk for hepatotoxicity and require treatment. To use the nomogram, the time of ingestion must be known and a serum acetaminophen level must be drawn at a known time at least 4 hours after ingestion. The time after ingestion is plotted on the x-axis and the acetaminophen level on the y-axis. If the intersection point of these two values falls above the treatment line, the patient is treated with N-acetylcysteine (NAC). In the United States, this treatment line is labeled “possible hepatic toxicity” and corresponds with a 4-hour postingestion acetaminophen level of 150 mcg/mL (Fig. 79-1).
13 What are the receptor effects and clinical effects of tricyclic antidepressant (TCA) poisoning?
TCAs have seven pharmacologic effects. Understanding these effects is helpful in remembering the associated clinical syndrome of TCA toxicity (Table 79-1).
Table 79-1 Pharmacologic Effects of Tricyclic Antidepressants
| Mechanism | Effect |
|---|---|
| Presynaptic biogenic amine reuptake inhibition (norepinephrine and serotonin) | Therapeutic antidepressant effect Early sympathomimesis Myoclonus Hyperreflexia |
| Fast sodium channel influx blockade | QRS duration prolonged PR interval prolonged Right axis deviation Bundle branch blockade Ventricular dysrhythmias Negative inotropy |
| Potassium channel efflux blockade | QTc prolongation |
| Muscarinic acetylcholine receptor blockade | Tachycardia Mydriasis Decreased sweating Hyperthermia Flushing Ileus Urinary retention |
| Histaminic receptor blockade | Sedation |
| Alpha receptor blockade | Sedation Orthostatic hypotension Miosis Reflex tachycardia |
| GABA-A receptor blockade | Seizures Status epilepticus |
GABA-A, γ-Aminobutyric acid-A.
14 What value is the electrocardiogram in patients with TCA poisoning?
15 How is cardiovascular toxicity of TCAs treated?
Cardiovascular toxicity of TCAs is treated first with sodium bicarbonate therapy, titrating initial bolus therapy to resolution of QRS prolongation and following this with continuous infusion of bicarbonate solution to alkalinize the serum and provide a loading dose of sodium ions. If the patient continues to have QRS prolongation or significant right axis deviation, despite alkalemia to pH of 7.55, hypertonic saline solution can also be administered. Lidocaine is the historical second-line agent in treating dysrhythmias, but the physician must be aware that lidocaine is also a sodium channel blocker and administration could potentiate seizures. Synchronous cardioversion should be used in patients with TCA overdose on the basis of current advanced cardiac life support guidelines when indicated. Torsades de pointes can be treated with magnesium sulfate infusion. Despite the QTc prolongation associated with TCA use, the tachycardia due to the antimuscarinic effects of TCAs often limits the likelihood of “R-on-T” phenomena. Finally, in recent years, lipid emulsion rescue has emerged as an antidotal treatment in life-threatening poisoning by lipophilic drugs. All TCAs are highly lipophilic, given their therapeutic targets in the CNS, and animal and human data suggest that TCAs and related compounds respond well to lipid rescue. Patients with known or suspected TCA cardiotoxicity and hemodynamic instability or malignant dysrhythmias are candidates for lipid emulsion therapy, discussed in more detail in Chapter 81 on cardiovascular drug toxicity.
Key Points Analgesics and Antidepressants
1. Patients with salicylate toxicity should start alkalinization therapy and have serum salicylate levels checked every 1 to 2 hours.
2. Hemodialysis should be initiated promptly in any patient with salicylate levels over 100 mg/dL or those with levels greater than 80 mg/dL with significant clinical deterioration or neurotoxicity.
3. Acetaminophen levels may be plotted on the Rumack-Matthew nomogram only if the patient has had a single, acute ingestion of acetaminophen at a known time at least 4 hours before presentation.
4. Any suspected or confirmed acetaminophen-toxic patient should immediately start receiving NAC, by either the oral or IV route.
5. Sodium bicarbonate is the treatment of choice to prevent seizures and arrhythmias in TCA overdose and should be administered as boluses until the QRS is <100 milliseconds.
1 Bailey B., Buckley N.A., Amre D.K. A meta-analysis of prognostic indicators to predict seizures, arrhythmias or death after tricyclic antidepressant overdose. J Toxicol Clin Toxicol. 2004;42:877–888.
2 Bradberry S.M., Thanacoody H.K., Watt B.E., et al. Management of the cardiovascular complications of tricyclic antidepressant poisoning: role of sodium bicarbonate. Toxicol Rev. 2005;24:195–204.
3 Body R., Bartram T., Azam F., et al. Guidelines in Emergency Medicine Network (GEMNet): guideline for the management of tricyclic antidepressant overdose. Emerg Med J. 2011;28:347–368.
4 Engels P.T., Davidow J.S. Intravenous fat emulsion to reverse haemodynamic instability from intentional amitriptyline overdose. Resuscitation. 2010;81:1037–1039.
5 Heard K.J. Acetylcysteine for acetaminophen poisoning. N Engl J Med. 2008;359:285–292.
6 Higgins R.M., Connolly J.O., Hendry B.M. Alkalinization and hemodialysis in severe salicylate poisoning: comparison of elimination techniques in the same patient. Clin Nephrol. 1998;50:178–183.
7 Johnson M.T., McCammon C.A., Mullins M.E., et al. Evaluation of a simplified N-acetylcysteine dosing regimen for the treatment of acetaminophen toxicity. Ann Pharmacother. 2011;45:713–720.
8 Khandelwal N., James L.P., Sanders C., et althe Acute Liver Failure Study Group. Unrecognized acetaminophen toxicity as a cause of indeterminate acute liver failure. Hepatology. 2011;53:567–576.
9 Kolecki P.F., Curry S.C. Poisoning by sodium channel blocking agents. Crit Care Clin. 1997;13:829–848.
10 O’Malley G.F. Emergency department management of the salicylate-poisoned patient. Emerg Med Clin North Am. 2007;25:333–346.
11 Pentel P.R., Benowitz N.L. Tricyclic antidepressant poisoning. Management of arrhythmias. Med Toxicol. 1986;1:101–121.
12 Pierog J.E., Kane K.E., Kane B.G., et al. Tricyclic antidepressant toxicity treated with massive sodium bicarbonate. Am J Emerg Med. 2009;27:1168. e3-e7
13 Wells K., Williamson M., Holstege C.P., et al. The association of cardiovascular toxins and electrocardiographic abnormality in poisoned patients. Am J Emerg Med. 2008;26:957–959.