Chapter 32 Analgesia and relief of pain
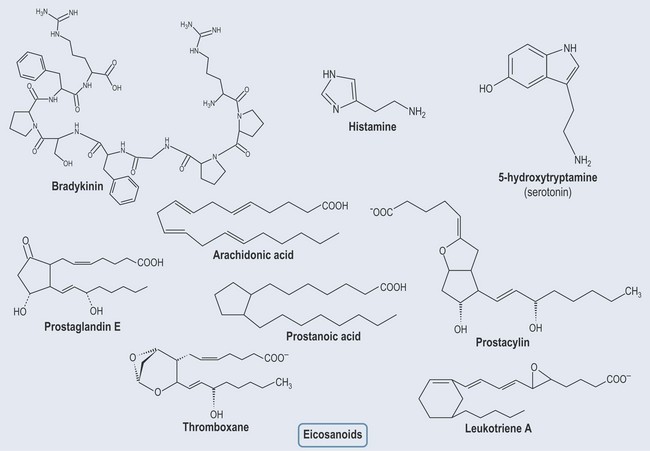
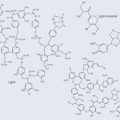
Bradykinin (Figure 32.3) is released when tissue is damaged and so is found in inflammatory processes, e.g. joint inflammation. It stimulates and sensitizes nerve endings, which leads to the stimulus that registers pain with the body. Anti-inflammatories and aspirin inhibit prostaglandin synthesis and therefore the release of mediators that create pain (see Chapter 30 ‘Inflammation and the immune system’, p. 228).
Analgesics
Sites of Action
Terminology
Specific Analgesics
Paracetamol
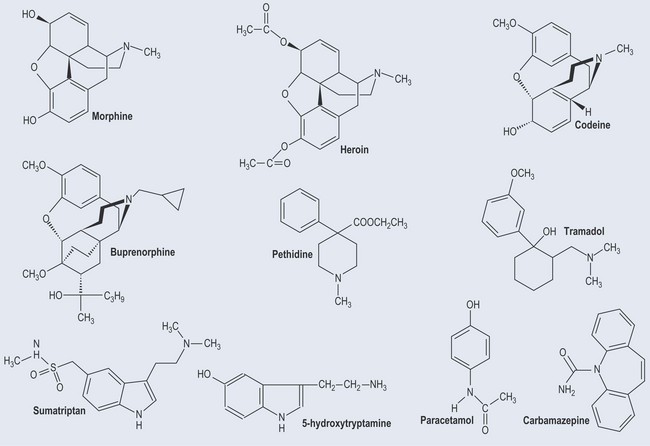
Paracetamol (Figure 32.4) acts largely as a painkiller and has very little effect on inflammation.
Opioid Analgesics
The opiate-based drugs alter the perception and response to pain.
• Morphine
Types of Morphine Administration
Oral
Not the most effective way to give lasting relief because morphine is subject to a high first-pass metabolism (see Chapter 17 ‘Metabolism’, p. 129). Manufacturers have, however, produced a slow-release oral preparation.
Intravenous
This is the usual route of administration. In terminal cases, use is made of a pump system that patients can operate independently when pain relief is required. Otherwise morphine can be given intramuscularly or subcutaneously. Very little of the administered drug crosses the well-protected blood–brain barrier. What medication does get there peaks between 30 and 45 minutes after administration.
Drug Interactions
Opiate Partial Agonists and Opiate Antagonists
• Buprenorphine
• Tramadol
Migraine Medication
• Treatment
Triptans
Local Anaesthetics
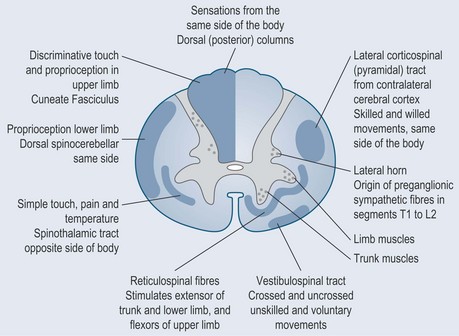
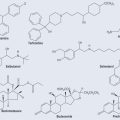
Lidocaine and novocaine are sodium-channel blockers (see Figure 19.6, p. 141 and Figure 31.2, p. 237). When sodium is not allowed to move through the channels, depolarization in the neurons is no longer possible. This means that the neuron will be unable to transmit an action potential; it is this that creates the anaesthesia.