Anaesthesia for the Bariatric Patient
MEASURING OBESITY
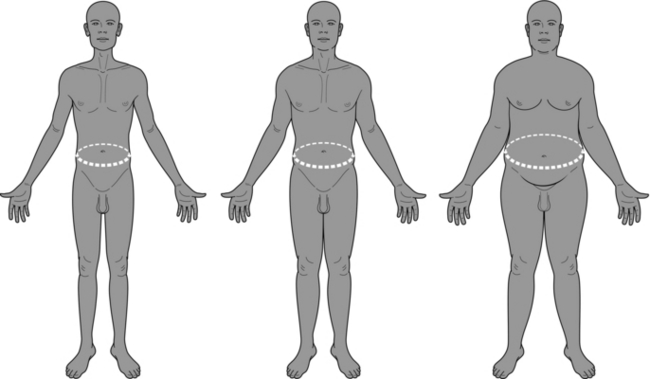
BMI has limitations and may not be representative in certain ethnic groups, or in those of athletic build. It cannot describe the distribution of weight, nor discriminate the nature of the excess tissue. However, calculation of BMI, from two ubiquitous measurements, requires the minimum equipment and expertise. Hence, it is likely to remain the measure of choice as a shorthand to express obesity (Table 25.1, Fig. 25.1).
TABLE 25.1
WHO Obesity Classes by BMI (Other Nomenclatures Included)
| Category | BMI (kg m–− 2) |
| Underweight | < 18.5 |
| Normal | 18.5–24.9 |
| Overweight (pre-obese) | 25–29.9 |
| Obese Class I | 30–34.9 |
| Obese Class II (severe to morbid) | 35–39.9 |
| Obese Class III (morbid to super) | 40 + |
| (Super obesity) | 45–50 + |
COMORBIDITY AND ANAESTHETIC MANAGEMENT
Airway
Anatomy: In the obese patient, the airway undergoes progressive adipose infiltration. This occurs at all levels from the oropharynx through to the glottis and vocal cords. Adipose infiltration causes progressive narrowing and reduction in airway diameter, which may reduce by 50% or more from the physiological male normal of about 20 mm in the hypopharynx.
Careful positioning is key to successful management of the bariatric airway. This can be achieved either using specifically designed equipment, or special modifications to normal equipment. In urgent situations a number of aids to achieving the position have been suggested including multiple towels, fluid bags or inflatables. The key is to ensure true neck flexion and AO extension. This is best achieved by ensuring that the patient posture, in particular neck/head position is viewed from the side (Fig. 25.2A and B).
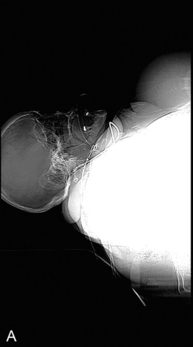
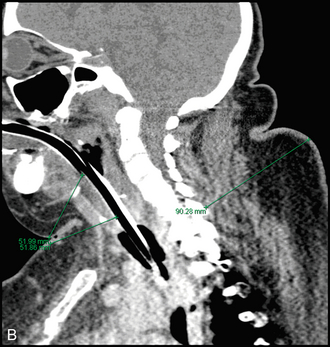
FIGURE 25.2 (A) Lateral CT Scout (supine, female, BMI 59 kg m− 2). Note neck position, ‘free-floating’ head and the potential for neck, chest and breast adipose tissue to hinder airway management. (B) Sagittal cross-section (BMI 55 kg m− 2). Note depth of both anterior and posterior airway structures and the extent of airway soft tissue around the 7.5 tracheal tube.
Airway Adjuncts: A range of products to assist in the management of difficult airways exists. Simple adjuncts such as oral and nasopharyngeal airways, and the use of CPAP can help to splint the airway open. Laryngeal mask airway products retain their role in airway salvage. Their routine use in the morbidly obese patient remains controversial, focusing on concerns around pulmonary aspiration and optimization of pulmonary function.
Anatomy
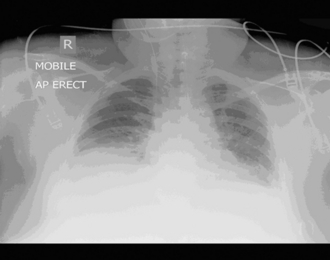
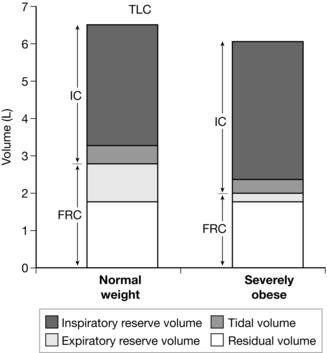
Lung size is predicted by height or ideal body mass, rather than gross weight. The lung fields of obese patients often look small when assessed by chest radiography (Fig. 25.3). This is an artefact of accommodating the patient on the chest X-ray. Total lung capacity is usually nearly normal and it is functional spirometry which reveals the associated pathology (Fig. 25.4).
Pathophysiology
 Functional residual capacity decreases (Fig. 25.5) and closing volume increases. Resulting atelectatic shunt reduces PaO2. At higher levels of morbid obesity, tidal ventilation may impinge on closing volume even in the standing position.
Functional residual capacity decreases (Fig. 25.5) and closing volume increases. Resulting atelectatic shunt reduces PaO2. At higher levels of morbid obesity, tidal ventilation may impinge on closing volume even in the standing position.
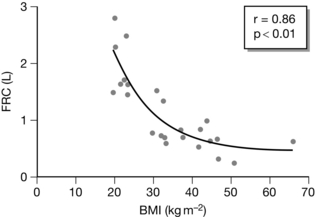
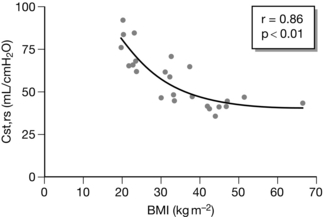
FIGURE 25.5 Changes in functional residual capacity (FRC) with increasing body mass index (BMI). (Adapted from Pelosi et al (1998).)
 FEV1 decreases, although the FEV1/FVC ratio is often preserved, particularly with central obesity patterns.
FEV1 decreases, although the FEV1/FVC ratio is often preserved, particularly with central obesity patterns.
 Work of breathing increases by 70% from low levels of obesity to an energy cost 300% higher in complicated, high BMI states. The energy cost of maintaining adequate minute ventilation is mitigated by a reduction in tidal volume, resulting in rapid, shallow breathing at rest.
Work of breathing increases by 70% from low levels of obesity to an energy cost 300% higher in complicated, high BMI states. The energy cost of maintaining adequate minute ventilation is mitigated by a reduction in tidal volume, resulting in rapid, shallow breathing at rest.
The elastic load increases (reduced static compliance; Fig. 25.6). This is a reflection of both the reduced elastance of chest wall and parenchymal tissue and tidal ventilation occurring at lower lung volumes. Dynamic compliance (i.e. resistance to gas movement) also falls. In the lower airway, there is narrowing of the small conducting airways. This may be due to multiple factors:
CARDIOVASCULAR PATHOPHYSIOLOGY
Cardiac Pathophysiology
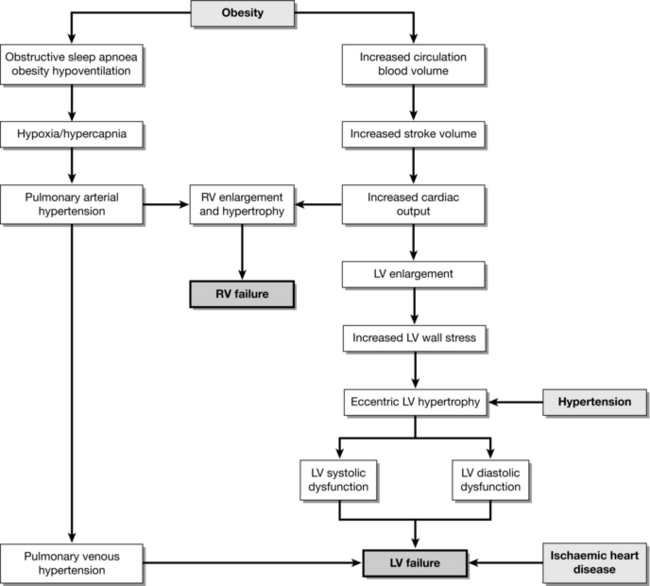
The heart of the obese patient may exhibit a number of pathological changes (Fig. 25.7). These may be related to either the primary obesity or associated comorbidity, e.g. hypertension, diabetes, hyperlipidaemia or sleep apnoea.
Electrophysiology
 Atrial fibrillation is the commonest arrhythmia associated with obesity and the prevalence increases exponentially with BMI.
Atrial fibrillation is the commonest arrhythmia associated with obesity and the prevalence increases exponentially with BMI.
 Voltage magnitudes vary and QRS complex size is not reliable for diagnosis.
Voltage magnitudes vary and QRS complex size is not reliable for diagnosis.
 Conduction axis is frequently left-shifted, but this may be caused by physical displacement of the heart from the normal position and rotation.
Conduction axis is frequently left-shifted, but this may be caused by physical displacement of the heart from the normal position and rotation.
LIVER
Intra-abdominal pressure is raised in obesity and increases with BMI. Resting pressure is usually around twice normal, at 10 mmHg (Fig. 25.8). During laparoscopic procedures, the pneumoperitoneal pressure may need to be high to allow adequate vision. Care should be taken because pressures of 15 mmHg or higher have been shown to significantly reduce femoral vein, gut, visceral and portal blood flows. Measures such as positioning and adequate relaxation should be addressed first.
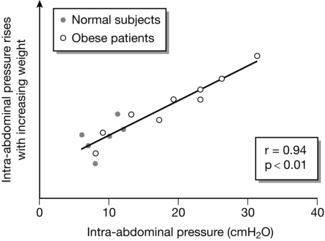
FIGURE 25.8 Relationship between body weight and intra-abdominal pressure. (Adapted from Pelosi et al (1999).)
PHARMACOLOGY
Patients who are obese may display altered pharmacokinetics and pharmacodynamics (Table 25.2). These factors have clinical relevance. The application of basic concepts such as drug solubility, compartment volumes, transportation and metabolism may be helpful. However, the interactions are complex and reference to published data should be made. For these reasons, controversy remains and particular care should be taken with the use of target controlled infusion algorithms developed for patients of normal weight.
TABLE 25.2
Factors Which Affect the Pharmacokinetic and Pharmacodynamic Properties of Drugs in Obesity
| Kinetic Property | Effect of Increasing Obesity |
| Blood volume and cardiac output | Increase |
| Adipose and lean body mass | Increase |
| Hepatic blood flow and glucuronidation rate | Increase |
| GFR and renal excretion | Increase |
| Cytochrome P450 isoenzymes | Variable |
| Renal tubular reabsorption | Decrease |
Muscle Relaxants
Suxamethonium: Suxamethonium has traditionally been the drug of choice for facilitating tracheal intubation in the obese. This has largely been driven by concerns about the need for rapid sequence induction, the potential for difficult intubation and the difficulty of managing the airway with a face mask and airway adjuncts. Morbidly obese patients have been shown to have increased pseudocholinesterase activity and a larger immediate distribution volume. Dosing based on 1 mg kg− 1 total body weight has been demonstrated to give better intubating conditions than dosing by ideal body weight or lean body weight, but at the expense of approximately 90 additional seconds before return of spontaneous breathing.
Non-Depolarizing Agents: The quaternary ammonium group makes non-depolarizing relaxants highly ionized and generally poorly lipophilic. This limits their distribution to extracellular fluid. Dosing based on total body weight uniformly leads to a prolonged duration of action. Consensus suggests that dosing on the basis of ideal body weight is predictable and acceptable, although some authorities suggest that correction for body surface area may be more precise.
Reversal Agents: Limited data exists for the most appropriate dose of neostigmine in the morbidly obese. Dosing studies suggest that if a suboptimal ceiling effect is observed with neostigmine, full twitch height recovery from this point in the morbidly obese patient is prolonged.
Sugammadex: The cyclodextrin sugammadex rapidly and selectively binds rocuronium (and vecuronium to a lesser extent) to form inactive complexes. Consequently, there is an agent-specific alternative to neostigmine and, because of the speed of the reversal, the possibility for a two-agent alternative to suxamethonium for rapid sequence induction. Dosing of sugammadex by total body weight is currently advised in all patients. However, some emerging data suggests that a dose based on a modification of lean body mass may be effective.
POSTOPERATIVE CARE OF THE OBESITY SURGERY PATIENT
Presentations associated with the surgical procedure include the following.
Weight Loss and Malnutrition
 A careful history should be taken, including obtaining information about the operating centre, follow-up arrangements and weight history.
A careful history should be taken, including obtaining information about the operating centre, follow-up arrangements and weight history.
 It is prudent to consult an expert centre for advice. Consider band deflation and be aware of post-surgery anatomical alterations.
It is prudent to consult an expert centre for advice. Consider band deflation and be aware of post-surgery anatomical alterations.
 Care should be taken in the use of modified- release medications. Mechanisms differ and may be severely affected in patients who have undergone bariatric surgery.
Care should be taken in the use of modified- release medications. Mechanisms differ and may be severely affected in patients who have undergone bariatric surgery.
Alvarez A., Brodsky J.B., Lemmens H.J.M., Morton J.M., eds. Morbid obesity. Cambridge: Cambridge University Press, 2010.
Ortiz V.E., Wiener-Kronish J., eds. Perioperative anaesthetic care of the obese patient. Informa Healthcare, 2010.
Pelosi, P., Croci, M, Ravagnan, I, et al. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth. Analg. 1998;87:654–660.