CHAPTER 13 An Overview of the Modern Era of Breast Reduction
Key Terms
Reduction Mammaplasty
Goals of reduction mammaplasty
To best serve our patients’ needs and desires the surgeon needs a solid knowledge of anatomy.
Breast anatomy
Circulation
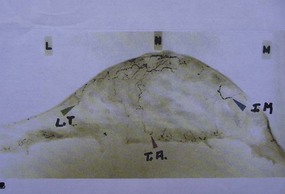
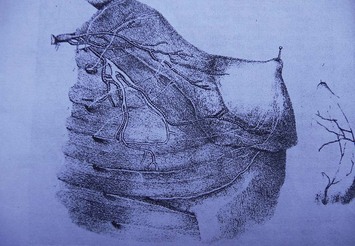
Maliniac1 in 1943 performed cadaver injections in 103 female breasts followed by roentgenographic studies. Mathes2 used latex and barium injections and dissections to further define the blood supply. His studies showed the main sources of blood supply to the breast (Fig. 13.1A, B) to be from:
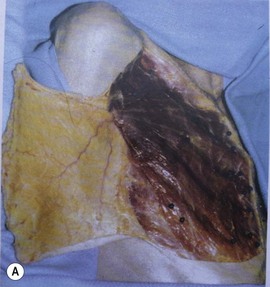
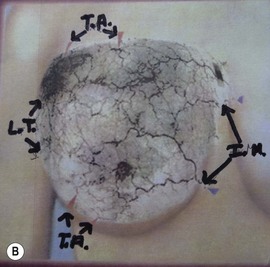
Fig. 13.1 An anatomic dissection performed by Dr. Stephen Mathes showing the vascular anatomy of the breast.
These studies, in addition, identify direct communications of the vascular network between the terminal branches of the lateral thoracic artery, the internal mammary artery, and the musculocutaneous branches of the thoracoacromial arteries and associated veins (Fig. 13.2).
Functional anatomy (lactation and innervation)
Before describing the various flaps we need to consider the pertinent anatomy of the breast parenchyma and the innervation of the nipple. The simplified version of breast parenchyma is that 10–100 alveoli comprise a breast lobule. Multiple lobules form a single lobe. Each lobe is drained by 15–20 lactiferous ducts. The end of a duct dilates becoming the lactiferous sinus which empties into the nipple. The nipple is composed of two layers of circular and longitudinal smooth muscle the contraction of which makes the nipple firm, erect and allows milk to be emptied from the lactiferous sinuses.4 The lobules are attached to the skin by dense fibrous bands termed Cooper’s ligaments. The breast is firmly fixed to the skin in the area of the areola.
Common sense tells us that there must be adequate parenchyma in the nipple bearing flap for sufficient milk production, and that the milk must have an intact pathway to the nipple which must be innervated so that it can become erect and empty on demand. It stands to reason that broader, thicker flaps will produce and transport more milk than narrower thin flaps. This is not to say that all or even most of the women undergoing reduction mammaplasty will want to be able to lactate postoperatively. It is however, the reason that surgeons whose primary technique greatly reduces or eliminates the possibility of breast feeding, should have the versatility required to employ a technique that retains normal breast function.6
Innervation
Nipple
Most authors agree that nipple sensibility is primarily derived from the lateral cutaneous branch of the fourth intercostal nerve3 (Fig. 13.3). Lesser contributions are made by the anterior cutaneous branches of the third, fourth, and fifth intercostal nerves and the third and fifth lateral cutaneous branches.
Skin
Innervation of the skin is not really a matter of practical concern in reduction mammaplasty because it comes superficially from all directions. The nerves are: (1) the supraclavicular branch of the cervical plexus from C3 and C4, (2) the lateral cutaneous branches of the anterior thoracic intercostal nerves, and (3) the anterior perforating cutaneous branches of the intercostal nerves.4,5,7
Fascia
The body’s superficial fascia system invests the breast parenchyma with a superficial and deep layer.7 The superficial layer has the same important role in reconstituting the breasts during reduction mammaplasty as does the superficial muscular aponeurotic system (SMAS) in the face and neck and Scarpa’s fascia in the abdomen during the rhytidectomy and abdominoplasty respectively. This superficial layer of fascia is immediately deep to the subcutaneous fat and needs to be incorporated in the medial and lateral limbs as it is the repair of this fascia that takes the tension off the skin closure, presumably resulting in a more favorable scar. Superficial fascia repair should be performed on all incisions except the periareolar which is repaired with deep dermal sutures.
The posterior layer of the superficial fascia is on the deep surface of the gland. Between it and the fascia of the pectoralis major muscle is the well defined retromammary space, which contains loose areolar tissue and allows the breast to glide freely over the chest wall.7
Skin marking patterns and scars
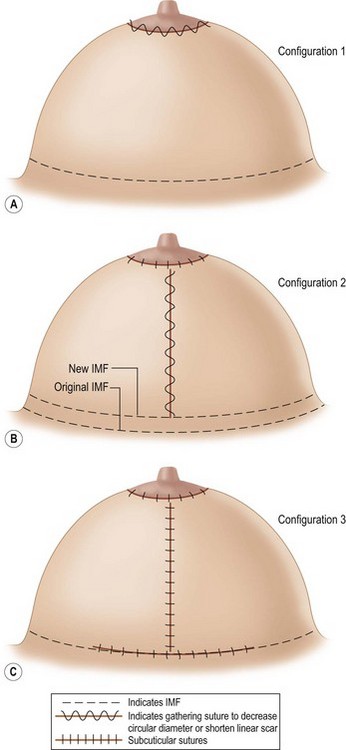
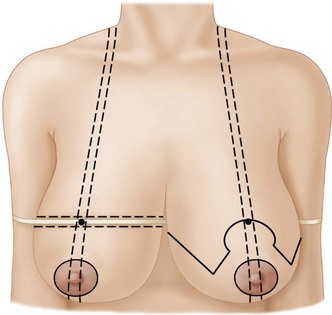
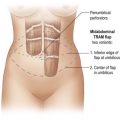
These basic configurations with multiple variations resulting in one or more of the following scars (Fig. 13.4A, B, C):
Analysis of Surgery Resulting in Configurations 1, 2, and 3
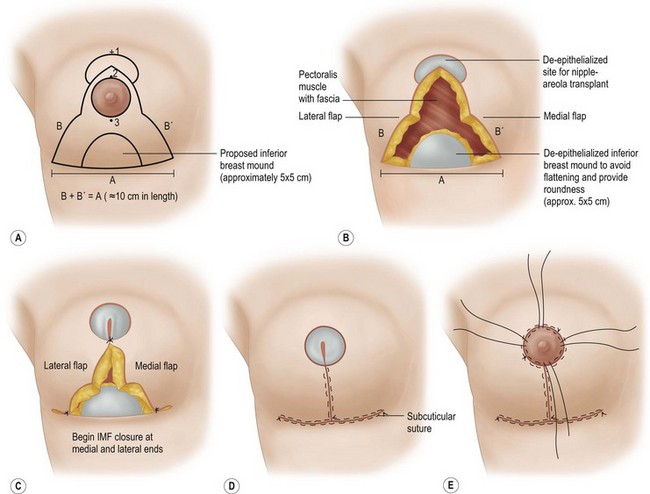
Configuration #18
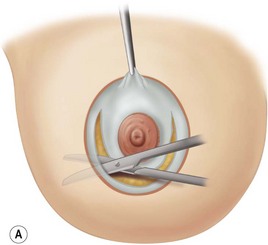
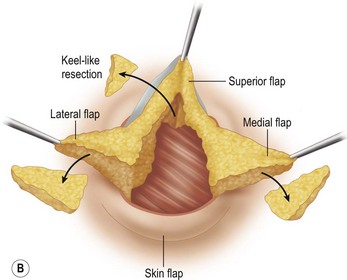
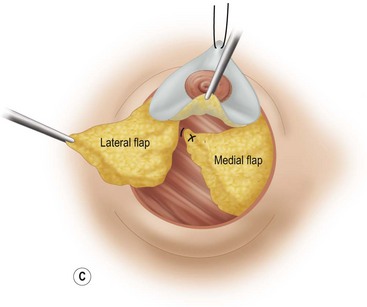
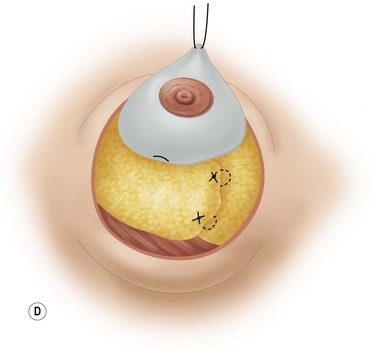
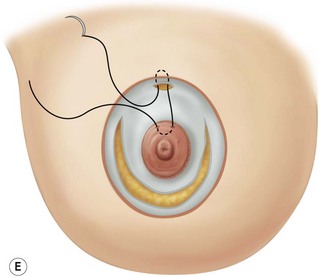
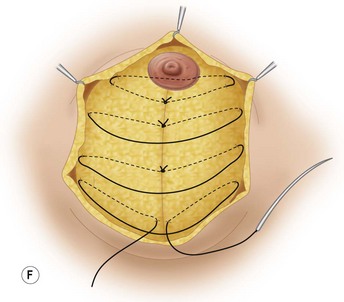
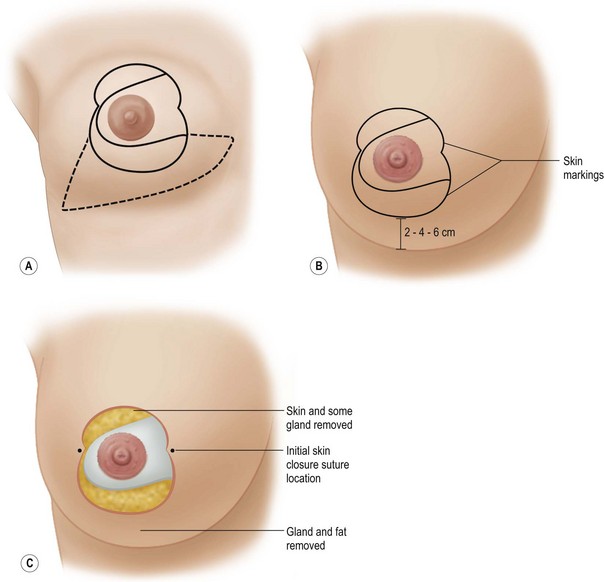
These diagrams demonstrate the oval skin and outer areola de-epithelialization pattern; the creation of a superior based flap with a crescent of parenchyma excised (Fig. 13.5A), the extent of which may be expanded to include tissue from the inferior, medial and lateral aspects of the breast (Fig. 13.5B). The medial and lateral glandular flaps are developed and crisscrossed under the superior based NAC flap (Fig. 13.5C, D). The superior (12 o’clock) aspect of the areola is then sutured in a subdermal window to the skin (gently folding the flap pedicle) and thus preventing enlargement of the scar (Fig. 13.5E) Lacing sutures traversing the entire thickness of the breast diameter support the conical shape of the breast and allows control of the NAC projection (Fig. 13.5F).
Disadvantages of the periareolar reduction mammaplasty are:
The proponents of this procedure have gained a degree of skill in this technique that the average plastic surgeon has found difficult to achieve. After an initial flurry of enthusiasm to utilize the periareolar procedure many have abandoned it. I am reluctant to criticize any technique that I have not tried to master. My initial bias against the technique was caused by the severe flattening created by the tension that the pursestring periareolar closure exerted on the breast mound. Benelli8 and Goes9 have overcome this by manipulating the breast mound with maneuvers such as crisscross flaps, lacing sutures, encompassing mesh, and extensive subcutaneous dissection to achieve aesthetically pleasing breasts. They appear to have succeeded by converting a compressible breast into a fixed, firm breast which resists the pressure of tight skin.
Configuration #2
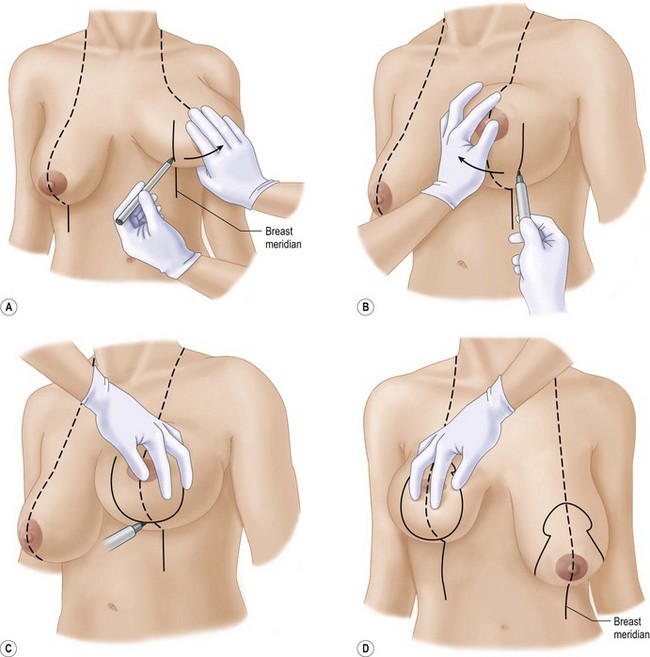
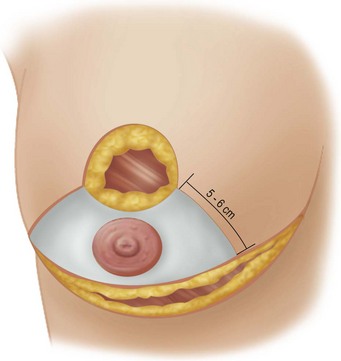
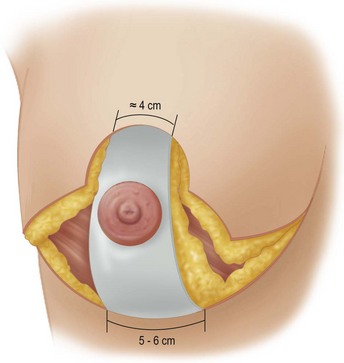
Advocates of vertical mammaplasty use primarily the mosque shape or the open circle for the neonipple–areola site (Fig. 13.6D) The nipple site is centered to correspond to the meridian of the breast with the superior border of the areola located at the level of the IMF. The markings from the lower edge of the nipple–areola site make use of the meridian line as it projects on the upper abdominal wall and the breast is maneuvered medially and laterally to determine the edges of the medial and lateral limbs (Fig. 13.6A, B); and also to determine how much tissue (skin and parenchyma) will be excised between the limbs. The incision pattern is rounded off 2–5 cm above the IMF (Fig. 13.6C) to protect against the lower end of the final scar projecting below the IMF and also to raise the level of the IMF.
Vertical mammaplasty surgeons with one notable exception10 use either superior11, medial,12 or lateral13 flaps. It is suggested that the length of a superior based flap should not exceed 10 cm as folding it can lead to vascular impairment. Indeed, if a superior based flap is going to be greater than 10 cm in length, Lassus will use a lateral based flap.13
Advantages of the vertical mammaplasty are:
Disadvantages of configuration #2
Configuration #3
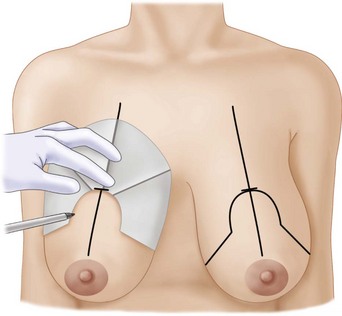
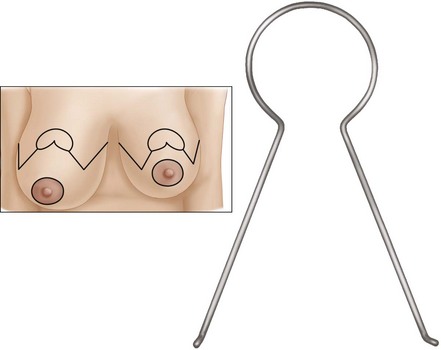
Patterns to fit different sized breasts were described by Wise in 195614 (Fig. 13.7). His concept has been simplified by the adjustable McKissock keyhole breast marker (Fig. 13.8). The marker can be opened more widely for broader bigger breasts and can be adjusted to compensate for asymmetry (Fig. 13.9). The retained tissue is equal on both sides. The top of the new NAC site should be at the level of the IMF and should bisect the breast rather than be on a direct line with the existing NAC if it is displaced, as it is in the right breast of this patient (Fig. 13.9). The most common error is for the nipple to be placed too high on the chest wall. This error can occur in all three configurations. It can be due to: (1) retraction of skin that was stretched preoperatively secondary to the heavy weight of the breast; (2) the medial and lateral vertical parenchymal limb closure pushing the nipple upward; (3) postoperative settling of parenchyma; (4) restretching of the vertically gathered skin in vertical mammaplasty; and/or (5) simply marking it too high on the chest wall. One way to ensure that the top of the areola is at the IMF is shown in Fig. 13.10.
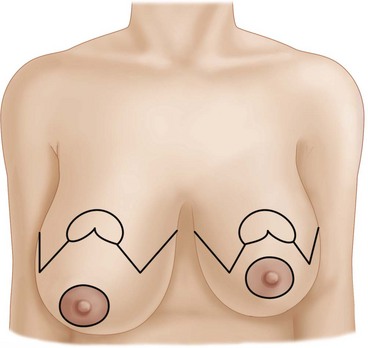
Fig. 13.9 The application of the marker adjusted to asymmetric breasts is demonstrated.
Note the symmetrical preservation of skin and parenchyma above the markings.
Determination of the length of the scar in the IMF. It is necessary to excise skin between the diverging medial and lateral limbs as well as below the limbs to the IMF (see Fig. 13.20A) The broader the breast the longer will be the scar in the IMF. It should be short enough to avoid it being seen medially in the cleavage area or laterally in the anterior axillary line. It is always shorter than the full length of the IMF.
Advantages of Configuration #3:
Disadvantages of Configuration #3:
Hybrids of Configurations #2 and #3 (Table 13.1)
Marchac24 (Figs 13.16, 13.17, 13.18) in a widely referenced publication has modified the traditional Configuration #2 or vertical mammaplasty markings to include a short (up to 7–8 cm) horizontal scar above the inframammary fold. In all other aspects he is a strict adherent to the superior based vertical mammaplasty technique.
Table 13.1 Comparison of Configuration 3 (Wise pattern) to Configuration 2 (vertical): different described techniques
| Configuration 3 | Configuration 2 | |
|---|---|---|
| A. Horizontal bipedicle | Strombeck15 | |
| B. Vertical bipedicle | McKissock16 | |
| C. Superior pedicle | Weiner19 | Lassus13 Lejour11 |
| Marchac19 Nahai30 | ||
| D. Inferior pedicle | Courtiss22 | Hammond10 |
| E. Lateral pedicle | Skoog31 | Lassus13 |
| F. Medial pedicle | Hall-Findlay12 | |
| G. Nipple transplantation | Gradinger17 and Cassis20 | |
| H. Superior medial | Hauben21 |
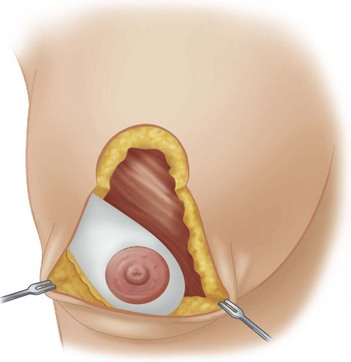
Fig. 13.16 Lateral based flap utilizing the vertical mammaplasty marking technique or Configuration #2 as advocated by Lassus.13
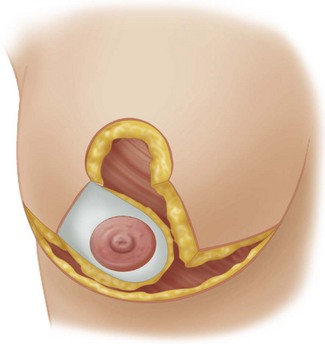
Fig. 13.17 Lateral based dermoglandular flap in combination with the Wise pattern reduction markings as advocated by Skoog.31
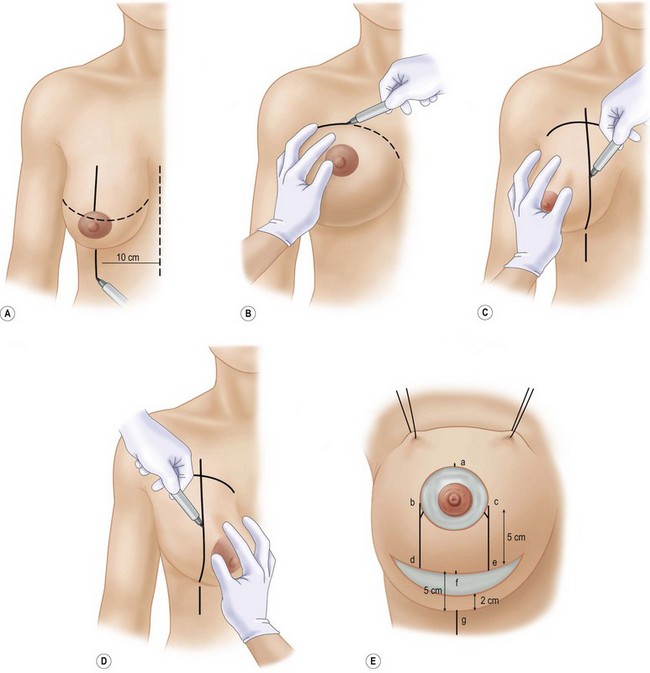
Fig. 13.18 The markings are made on the operating table, the patient being in the semisitting position.
Redrawn from Marchac D, DeObest G. Reduction mammaplasty and correction of ptosis with a short inframammary scar. Plast Reconstr Surg 1982;59:45.
Hall-Findlay12 uses the advantages of the diverging limbs provided by the Wise pattern (Fig. 13.19), but rather than extending the incision medially and laterally at the base of the limbs she rounds it off at the bottom to end above the IMF and uses a gathering suture for closure which results in somewhat of a pucker at the level of the new IMF and relies on nature to flatten this with time. Both of these authors present their work with great clarity and I feel have incorporated the advantages of Configuration #2 and Configuration #3.
Other marking configurations
Variations of ‘lateral’ approach,25,26 the B technique,27 and the L-shaped suture line28 have been published by highly respected surgeons. A review of these articles show excellent results. It is beyond the scope of this chapter.
Nipple-bearing flaps
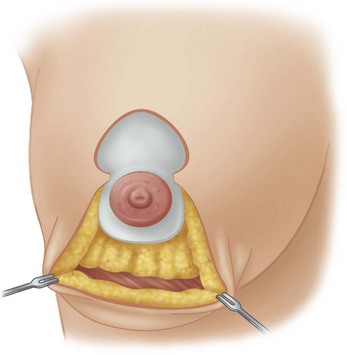
Fig. 13.13 Superior based pedicle flap as utilized in vertical mammaplasty or Configuration #2. After Lejour.11
Free Nipple Graft
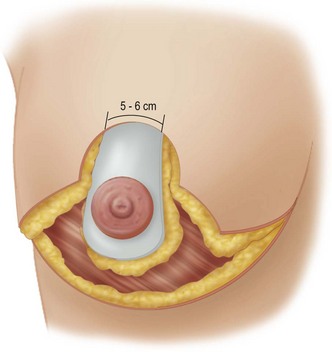
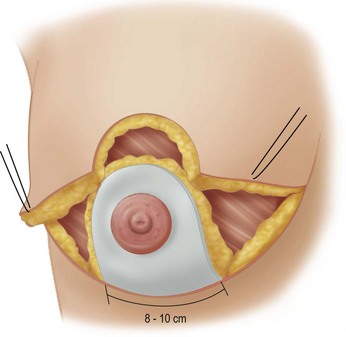
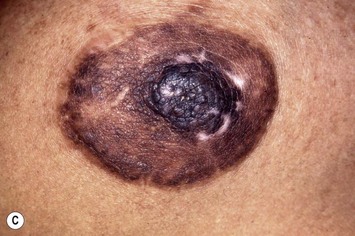
Advantages of the free nipple graft17,18,20 (Fig. 13.20)
Disadvantages of the free nipple graft technique
Conclusion
In this chapter I have attempted to present those techniques which appear most widely in the literature and seem to be most popular among plastic surgeons. As Goldwyn29 stated in his classic textbook on reduction mammaplasty ‘if, indeed reduction mammaplasty was simple and an excellent result were automatic, the need for this book detailing various concepts and techniques would not have been necessary… while not flitting from one technique to another like a butterfly the surgeon would be wise to have in his or her repertoire two or three procedures along with their variations in their execution.’ Quoting Goldwyn further ‘a surgeon may believe that one method fits every patient, the reality is that the surgeon may be trying to fit every patient to a single procedure.’
1 Maliniac JW. Arterial blood supply to the breast. Arch Surg. 1943;47:329.
2 Mathes ST, Schooler W. Inferior pedicle reduction techniques. In: Mathes ST, editor. Plastic surgery, Vol 6. Saunders-Elsevier; 2006:601. chapter 137
3 Cooper A. The anatomy of the breast. Longman, London, 1840, in The breast, principles and art edited by Spear, SL. Pertinent anatomy of the breast reduction mammaplasty, Golden edition. Philadelphia: Little Brown; 1990. p. 17
4 Haagensen CD. Anatomy of the mammary gland. In Diseases of the breast, 2nd ed, Philadelphia: Saunders; 1971:4-20.
5 Moore KL. The developing human. In Clinically oriented embryology, 2nd ed, Philadelphia: Saunders; 1977:379-380.
6 Gradinger G. Is there virtue in versatility in reduction mammaplasty? Aesth Surg J. 1997;17(5):308-315.
7 Rehman I. Embryology and anatomy of the breast. In: Spear SL, editor. The breast. St. Louis: Mosby; 1978:3-21.
8 Benelli LC. Periareolar Benelli mastopexy and reduction. In: Spear SL, editor. The breast, principles and art. Philadelphia: Lippincott-Raven; 1998:685.
9 Goes JCS. Periareolar mastopexy and reduction with mesh support. In: Spear SL, editor. The breast, principles and art. Philadelphia: Lippincott-Raven; 1998:697.
10 Hammond OC. Short scar periareolar inferior pedicle reduction (SPAIR) mammaplasty. Plast Reconstr Surg. 1999;103:890-901.
11 Lejour M. Vertical mammaplasty for breast reduction and mastopexy. In: Spear SL, editor. The breast, principles and art. Philadelphia: Lippincott-Raven; 1998:735.
12 Hall-Findlay EJ. Vertical breast reduction with medially based pedicle. Aesth Surg J. 185, 2002;March/April.
13 Lassus C. Vertical scar breast reduction and mastopexy without undermining. In: Spear SL, editor. The breast, principles and art. Philadelphia: Lippincott-Raven; 1998:717.
14 Wise RJ. A preliminary report on a method of planning the mammaplasty. Plast Reconstr Surg. 1956;17:367.
15 Strombeck JO. Mammaplasty, report of a new technique based on the two pedicle procedure. Br J Plast Surg. 1960;13:79.
16 McKissock PK. Reduction mammaplasty with a vertical dermal flap. Plast Reconstr Surg. 1972;49:245.
17 Gradinger GP. Reduction mammaplasty utilizing nipple-areola transplantation. Clin Plast Surg. 1988;15:641.
18 Gradinger GP. Breast reduction with the free nipple graft technique. In: Spear SL, editor. Surgery of the breast principles and art. Philadelphia: Lippincott-Raven; 1988:807-821.
19 Weiner DL. Reduction mammaplasty using superior pedicle technique. Aesth Plast Surg. 1982;6:7.
20 Casas LA, Byan MY, Pepoli PA, et al. Maximizing breast projection after free-nipple-graft reduction mammaplasty. Plastic Reconstr Surg. 2001;107:955.
21 Haupen DJ. Discussion on superior medial pedicle technique of reduction mammaplasty. Plast Reconstr Surg. 1989;83:479.
22 Courtiss EA, Goldwyn RM. Reduction mammaplasty by the inferior pedicle technique. Plast Reconstr Surg. 1982;69:45.
23 Hall-Findlay EJ. Pedicles in vertical breast reduction and mastopexy. Clin Plast Surg. 2002;29:379-391.
24 Marchac D, DeObest G. Reduction mammaplasty and correction of ptosis with a short inframammary scar. Plast Reconstr Surg. 1982;59:45.
25 Duformentel C, Mouchy R. Plastic mammoire par la methods oblique. Ann Chir Plast Esthet. 1961;6:45.
26 Schatten WE. Breast reduction: Lateral technique using inferiorly based flap in aesthetic breast surgery. Georgiade NG, editor. Aesthetic breast surgery. Baltimore/London: William & Wilkins. 1983: 196-204.
27 Regnault P. Reduction mammaplasty by the B technique. Plast Reconstr Surg. 1974;53:19.
28 Meyer R, Kisselring U. Reduction mammaplasty with an L-shaped suture line. Plast Reconstr Surg. 1975;53:139.
29 Goldwyn R. Reduction Mammaplasty. Philadelphia: Little, Brown & Co. 1990: 88.
30 Nahai F. Vertical reduction and operative techniques. Cuthbertson JHJr, Jones G, editors. Plastic and reconstructive surgery, Vol 6. May 1999:97-105. No 2
31 Skoog T. A technique of breast reduction. Acta Chir Scand. 1963;126:453-465.
32 Blondeel PN, Hamdi M, Vande Sijpe KA. The latero-central glandular pedicle technique for breast reduction. Br J Plast Surg. 2003;56:348-359.