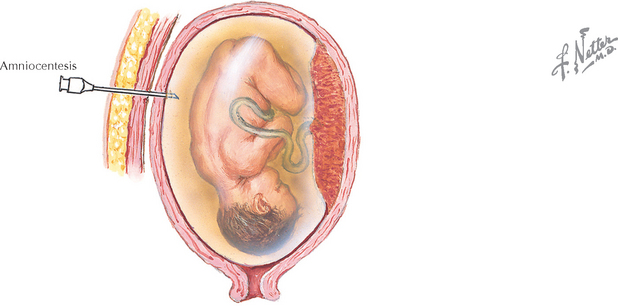
Chapter 227 Amniocentesis
REQUIRED EQUIPMENT
Gordon MC, Ventura-Braswell A, Higby K, Ward JA. Does local anesthesia decrease pain perception in women undergoing amniocentesis? Am J Obstet Gynecol. 2007;196:55.e1.
Sundberg K, Bang J, Smidt-Jensen S, et al. Randomized study of risk of fetal loss related to early amniocentesis versus chorionic villus sampling. Lancet. 1997;350:697.
Alfirevic Z, Sundberg K, Brigham S. Amniocentesis and chorionic villus sampling for prenatal diagnosis. Cochrane Database Syst Rev. 2004. CD003252.
Bombard AT, Powers JF, Carter S, et al. Procedure-related fetal losses in transplacental versus nontransplacental genetic amniocentesis. Am J Obstet Gynecol. 1995;172:868.
Bravo RR, Shulman LP, Phillips OP, et al. Transplacental needle passage in early amniocentesis and pregnancy loss. Obstet Gynecol. 1995;86:437.
Eddleman KA, Malone FD, Sullivan L, et al. Pregnancy loss rates after midtrimester amniocentesis. Obstet Gynecol. 2006;108:1067.
Eiben B, Osthelder B, Hammans W, Goebel R. Safety of early amniocentesis versus CVS. Lancet. 1994;344:1303.
Nicolaides K, Brizot M, de L, Patel F, Snijders R. Comparison of chorionic villus sampling and amniocentesis for fetal karyotyping at 10–13 weeks’ gestation. Lancet. 1994;344:435.
Petrikovsky BM, Kaplan GP. Fetal responses to inadvertent contact with the needle during amniocentesis. Fetal Diagnos Ther. 1995;10:83.
Somigliana E, Bucceri AM, Tibaldi C, et alItalian Collaborative Study on HIV Infection in Pregnancy. Early invasive diagnostic techniques in pregnant women who are infected with the HIV: a multicenter case series. Am J Obstet Gynecol. 2005;193:437.
American College of Obstetricians and Gynecologists. Assessment of fetal lung maturity. ACOG Educational Bulletin 230. Washington, DC: ACOG, 1996.
American College of Obstetricians and Gynecologists. Prenatal and preconceptional carrier screening for genetic diseases in individuals of Eastern European Jewish descent. ACOG Committee Opinion 298. Obstet Gynecol. 2004;104:425.
American College of Obstetricians and Gynecologists. Management of alloimmunization during pregnancy. ACOG Practice Bulletin 75. Obstet Gynecol. 2006;108:457.
American College of Obstetricians and Gynecologists. Screening for fetal chromosomal abnormalities. ACOG Practice Bulletin 77. Obstet Gynecol. 2007;109:217.
D’Alton ME, DeCherney AH. Prenatal diagnosis. N Engl J Med. 1993;328:114.
Elliott JP, Sawyer AT, Radin TG, Strong RE. Large-volume therapeutic amniocentesis in the treatment of hydramnios. Obstet Gynecol. 1994;84:1025.
Finegan JA. Amniotic fluid and midtrimester amniocentesis: a review. Br J Obstet Gynaecol. 1984;91:745.
Holzgreve W, Nippert I, Ganshirt-Ahlert D, et al. Immediate and long-term applications of technology. Clin Obstet Gynecol. 1993;36:476.
Jorgensen FS, Bang J, Lind AM, et al. Genetic amniocentesis at 7–14 weeks of gestation. Prenatal Diagn. 1992;12:277.
Moise KJJr. Management of rhesus alloimmunization in pregnancy. Obstet Gynecol. 2002;100:600.
Mujezinovic F, Alfirevic Z. Procedure-related complications of amniocentesis and chorionic villous sampling: a systematic review. Obstet Gynecol. 2007;110:687.
Nyberg DA, Hyett J, Johnson JA, Souter V. First-trimester screening. Radiol Clin North Am. 2006;44:837.
Rousseau O, Boulot P, Lefort G, et al. Amniocentesis before 15 weeks’ gestation: technical aspects and obstetric risks. Euro J Obstet Gynecol Reprod Biol. 1995;58:127.
Seeds JW. Diagnostic mid trimester amniocentesis: how safe? Am J Obstet Gynecol. 2004;191:607.
Stranc LC, Evans JA, Hamerton JL. Chorionic villus sampling and amniocentesis for prenatal diagnosis. Lancet. 1997;349:711.
Vandenbussche FP, Kanhai HH, Keirse MJ. Safety of early amniocentesis. Lancet. 1994;344:1032.