ALTITUDE-RELATED PROBLEMS
Altitudes of 8,000 to 14,000 ft (2,438 to 4,267 m) are attained regularly by skiers, hikers, and climbers in the continental United States. Outside the United States, mountain climbers may reach altitudes of up to 29,029 ft (8,848 m) (Mount Everest). Appendix 2 (page 512) lists common conversion numbers from feet to meters and vice versa.
Most difficulties at high altitude are a direct result of the lowered concentration of oxygen in the atmosphere. Although the percentage of oxygen in the air is relatively constant at about 20%, the absolute amount of oxygen decreases with the declining barometric pressure. Thus, at 19,030 ft (5,800 m) there is half the barometric pressure, and therefore half the oxygen, that is available at sea level. A person transported suddenly to this altitude without time to acclimatize or without the provision of supplemental oxygen would probably lose consciousness; sudden transport to the summit of Mount Everest (where the amount of inspired oxygen is 28% that at sea level) would cause rapid collapse and death. Although high-altitude illness is common with rapid ascent above 8,200 ft (2,500 m), the most common range for severe altitude illness is 11,500 to 18,000 ft (approximately 3,500 to 5,500 m). Above 18,000 ft (5,500 m), altitude is considered extreme, and a human deteriorates rather than adapts. Commercial airplanes are pressurized to an atmospheric pressure equivalent to that at 8,200 ft (2,500 m) above sea level.
PREVENTION OF ALTITUDE-RELATED DISORDERS
For any climb above 9,843 ft (3,000 m), spend an initial 2 to 3 nights at 8,202 to 9,843 ft (2,500 to 3,000 m) before proceeding higher. The first day should be a rest day. Do not sleep at an altitude more than 984 ft (300 m) above the previous night’s sleeping altitude. If anyone shows signs of altitude-related illness, spend additional time at this altitude. Do not ascend to sleep at a higher altitude if you have any symptoms of high-altitude illness.
For any climb above 13,000 ft (3,962 m), all members of the party should add 2 to 4 days for acclimatization at 10,000 to 12,000 ft (3,048 to 3,658 m). Subsequent climbing should not exceed 1,500 ft (457 m) per day. A rest day every 2 to 3 days is advised, along with an extra night for acclimatization with any ascent of 2,000 ft (609 m) or more. The party should sleep at the lowest altitude that does not interfere with the purpose of the expedition, and should sleep no higher than 1,312 to 1,968 ft (400 to 600 m) above the sleeping altitude of the previous night. The aphorism is “Climb high—sleep low.” After a person has acclimatized by adhering to a schedule of slow ascent, it is important to remember that even a few days at low altitude may cause the adjustments to disappear, so that a person is once again susceptible to altitude illness, particularly high-altitude pulmonary edema (HAPE).
In addition, the drug acetazolamide (Diamox) has proven to be useful in stimulating breathing, diminishing the sleep disorder associated with acute mountain sickness (AMS; see page 341), facilitating the body’s normal adjustment to high altitude, and thus improving nocturnal oxygenation. It is administered in a dose of 125 to 250 mg twice a day beginning 24 hours before ascent, and continued for a period of 2 days; within this period, the initial physiological acclimatization process should become operative. It may also be given as a 500 mg sustained-action capsule every 24 hours, with perhaps fewer side effects. Acetazolamide should be used if an ascent will be unavoidably rapid.
It is not known if sleep apnea contributes to AMS or HAPE. However, a person with sleep apnea should be extremely cautious when traveling at high altitude. Findings suggestive of sleep apnea include the following: daytime—excessive sleepiness, feeling tired on awakening, fatigue, irritability, difficulty with simple tasks, and shortness of breath; nighttime—loud snoring, witnessed episodes of diminished or absent breathing, poor sleep, frequent awakening, frequent urination at night, and bedwetting.
Probably no extra risk: extremes of age, obesity, diabetes, stable condition (e.g., no ongoing angina) after coronary artery bypass surgery, mild chronic obstructive pulmonary disease (COPD), controlled asthma, normal (low-risk) pregnancy, controlled high blood pressure, controlled seizure disorder, psychiatric disorder, cancer, inflammatory diseases
Caution: moderate COPD, congestive heart failure, sleep apnea, worrisome irregular heart rhythms, recurrent episodes of angina, sickle cell trait, cerebrovascular diseases, abnormal lung circulation, uncontrolled seizure disorder, radial keratotomy
High risk: sickle cell anemia with history of crises, severe COPD, pulmonary hypertension, poorly controlled congestive heart failure
If a person suffers from any chronic condition, he should clear any travel of an extreme nature (high-altitude, cold, hot, exertion) with a physician and become educated on potential problems and solutions.
HIGH-ALTITUDE PULMONARY EDEMA
Symptoms begin 1 to 3 days after arrival at high altitude. They include shortness of breath, cough, weakness, easy fatigue (especially when walking uphill), and difficulty sleeping. Signs of acute mountain sickness (AMS; see page 341) are often present. As greater amounts of fluid accumulate in the lungs, the victim develops drowsiness, severe shortness of breath, and rapid heart rate; his initial dry and gentle (“soft”) cough produces white phlegm and then blood (pink, frothy sputum’a late sign); he exhibits confusion and cyanosis (bluish discoloration of the skin, particularly noticeable in the nail beds and lips). If you place an ear to the victim’s chest, you may hear crackling or gurgling noises. The symptoms worsen at night. Rapidly, the victim becomes extremely agitated, disoriented, and sweaty; he is in obvious extreme respiratory distress. Confusion, collapse, and coma follow. The victim may show a fever of up to 101.3°F (38.5°C).
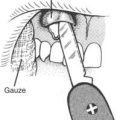
As soon as the earliest signs of HAPE are present, the victim should be evacuated (carried, if necessary) to a lower altitude at which there were previously no symptoms. Such warning signs include rapid heart rate (greater than 90 to 100 beats per minute at rest), weakness, shortness of breath, cough, difficulty walking, inability to keep up, and poor judgment. Maximum rest is advised. The definitive treatments are descent and the administration of oxygen; if it is available, oxygen at a flow rate of 4 to 6 liters per minute should be administered by facemask (see page 431). Improvement is rarely noted until oxygen is administered or descent of at least 1,000 to 2,000 ft (304 to 608 m) is accomplished. If the victim improves, diminish the flow rate of oxygen to 2 to 4 liters per minute to conserve supplies.
Have the victim inhale albuterol or salmeterol from a metered dose inhaler according to the directions. The administration of fluid pills (diuretics) is controversial and should be done only under strict medical supervision, as should the administration of morphine.
Some aid stations in high-altitude regions are equipped with an inflatable pressure bag (such as a “Gamow bag”) large enough to enclose a human. This is used to simulate conditions at lower altitude and may be used to treat moderate or severe high-altitude illness. The cylinder-shaped Gamow container is a small, portable hyperbaric chamber that can be pressurized with a foot pump to 2 lb (0.9 kg) per square inch, which simulates a descent of approximately 5,248 ft (1,600 m); the exact equivalent of descent depends on the altitude at which the bag is deployed. The victim should be placed in the bag for a minimum of 2 hours. In addition, oxygen from a tank can be administered to the victim by facemask (see page 431) within the bag.
HIGH-ALTITUDE CEREBRAL EDEMA
High-altitude cerebral edema (HACE) is the medical term for a disorder (theoretically linked to brain swelling) that involves an alteration of mental status seen at high altitude, related to diminished atmospheric oxygen. It may be present in someone who has worsened from acute mountain sickness (see below) or who is suffering from HAPE. Symptoms include headache (often throbbing), difficulty walking (loss of balance, inability to walk a straight line, staggering, or frank inability to walk), clumsiness, confusion, amnesia, difficulty in speaking, drowsiness, vomiting, and, in severe cases, blurred vision, blindness, unconsciousness, paralysis, and/or coma. Other symptoms may include mood changes, hallucinations, paralysis of an arm and/or leg, and seizures (rare). Victims are often gray or pale in appearance. Imbalance or the inability to walk heel to toe in a straight line is a very worrisome sign and should prompt immediate action to treat the victim. An exremely drowsy person may slip rapidly into a coma. “High-altitude headache” is often the first noxious symptom noted on exposure to high altitude, and may be the harbinger of acute mountain sickness (AMS—see below).
The treatment for HACE is immediate descent to an altitude below one at which the victim previously had no symptoms, and the administration of oxygen at a flow rate of 5 to 10 liters per minute by face mask or nasal cannula (tube) (see page 431). If the victim becomes severely ill, he should be brought (carried, if necessary, and preferably in the sitting position) to a lower altitude (below 5,000 ft, or 1,524 m). In addition, administration of the steroid drug dexamethasone (Decadron) 8 mg first dose, and then 4 mg every 6 hours until descent is accomplished, may be helpful. The pediatric dose of Decadron is 0.5 mg/kg (2.2 lb) of body weight for the first dose, followed by 0.15 mg/kg every 6 hours. Again, never leave a potentially seriously ill person to fend for himself. A victim of HACE or HAPE can deteriorate rapidly, and most will need to be transported down the mountain. As with HAPE, a Gamow bag can be used for treatment. Because the early symptoms of acute mountain sickness (see below) and HACE are similar, pay close attention to the condition of ill members of your climbing party.
ACUTE MOUNTAIN SICKNESS
The most common and disabling symptom of AMS is headache that typically occurs on the second or third day at high altitude and may be complicated by difficulty in walking (particularly if HAPE is present) and impaired memory. The headache is mild to severe, throbbing, in both temples or the back of the head, worse during the night and on awakening, and worsened by straining or bending over. Mild symptoms of HACE accompany AMS; they include decreased appetite, mood swings, and lack of interest in activity. Some victims complain of a deep inner chill. AMS is sometimes mistaken for a viral illness, such as the flu, or exhaustion or dehydration. Lassitude may be so severe that the victim is too apathetic to contribute to his or her own basic needs. The symptoms of AMS may be confused with dehydration, exhaustion, bacterial or viral infection, hypothermia, carbon monoxide poisoning, migraine headache, low blood sugar, transient ischemic attack or stroke, illicit drug ingestion, or psychiatric disease.
Prochlorperazine (Compazine) 10 mg by mouth or 25 mg by suppository can be given for nausea and vomiting, with the added benefit that it may stimulate the beneficial ventilatory (breathing) response that is triggered by a low oxygen content in the blood (associated with altitude and called the “hypoxic ventilatory response”). The dose in children older than 2 years of age is 0.4 mg/kg (2.2 lb) of body weight per day, by mouth or by oral suppository, in three or four divided doses. Promethazine (Phenergan) is fine as an alternative for adults, in a dose of 25 to 50 mg by mouth or suppository. Aspirin, acetaminophen, or ibuprofen may be given for headache. Avoid the use of alcohol or other respiratory depressants.
If an oxygen cylinder is available (see page 431), low-flow (0.5 to 1.5 liters per minute) oxygen by nasal cannula (tube) or facemask is particularly effective if used for sleep. This alone may be adequate to halt the progression of mild AMS and allow a victim to acclimatize without descent to a lower altitude. However, if this approach is taken, the victim should not be left alone until all symptoms of AMS have resolved. The victim who spends a few hours in a hyperbaric chamber, which simulates descent, will notice diminution of symptoms and benefit from hastened acclimatization. The “Gamow bag,” and other similar lightweight fabric pressure bags, are inflated by manual air pumps. Inflation at 2 pounds per square inch is roughly equivalent to a descent of 5,249 ft (1,600 m). A few hours of pressurization may have noticeable beneficial effect for many hours. To completely eliminate AMS, it is sometimes necessary to remain within the bag for 12 hours or more.
OTHER DISORDERS OF HIGH ALTITUDE
High-Altitude Flatus Expulsion (HAFE)
High-altitude flatus expulsion (HAFE) is the spontaneous and unwelcome passage of increased quantities of rectal gas noted at high altitude. It may become an embarrassment but is of no true medical concern. Avoid foods such as chili and beans that are known to induce flatulence at low altitudes, and show consideration for other members of the party in sleeping arrangements. If stricken, a traveler may benefit from chewable tablets of simethicone (Mylicon 80 mg) or simethicone 80 mg with activated charcoal 250 mg (Flatulex tablets) once or twice a day. Charcoal Plus is another simethicone-activated charcoal preparation.
Altitude Throat
Altitude throat (pharyngitis) is a sore throat caused by nasal congestion and mouth breathing during exertion at high altitudes. Because the air is dry and cold, the protective mucous coating of the throat is dried out and the throat becomes extremely irritated, with redness and pain. In general, this can be distinguished from a bacterial or viral infection (see page 195) by the absence of fever, swollen lymph glands in the neck, or systemic symptoms (fatigue, muscle aches, sweats, and the like). Prevention is difficult and treatment is only mildly satisfying. The victim should keep his throat moist by sipping liquids and sucking on throat lozenges or hard candies (Life Savers, for instance). As soon as convenient, nighttime breathing of warm humidified air should be instituted. Avoid anesthetic gargles, since they will mask the signs of a true infection. If the inside of the nose becomes dried out, this may be treated with topical ointment (e.g., bacitracin, mupirocin, or petroleum jelly).
High-Altitude Bronchitis
Most bronchitis has an infectious cause (see page 205). High-altitude bronchitis is more likely to be caused by relative hyperventilation of cold, dry air. This causes the secretions in the respiratory passages to thicken. The resulting airway irritation causes a persistent cough, which can cause coughing fits sufficiently severe to lead to rib fractures. Treatment consists of humidification of inspired air, which can be accomplished transiently by cautiously breathing steam, and over the longer term by breathing through a porous scarf or balaclava that allows retention of moisture and heat.