CHAPTER 7 Allografts for the Arthritic Knee
 Biologic joint restoration should be considered as an alternative to arthroplasty in young, active individuals.
Biologic joint restoration should be considered as an alternative to arthroplasty in young, active individuals.Introduction
Osteochondral allografts have become an integral part of articular cartilage restoration and repair. The use of osteochondral allografts for the treatment of focal, chondral, and osteochondral lesions in the knee is well supported by clinical experience and peer-reviewed literature.1–3 However, the use of allografts in the treatment of more advanced diseases, such as that seen in arthritis, is not as well established. Nonetheless, the need for a biologic treatment option for young individuals with degenerative conditions of the knee is clear. While this chapter describes the technical components of osteochondral allograft surgery, it is more important to understand the indications for using allografts as opposed to traditional implants.
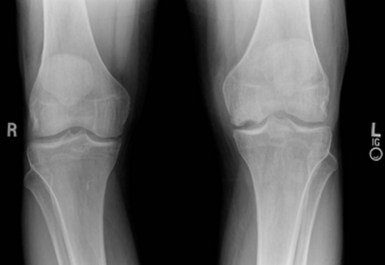
Fundamentally, biologic joint restoration may be appropriate in any patient considered too young or active for conventional arthroplasty. While these criteria are often vague, our practice is to evaluate any patient younger than 50 years for potential biologic reconstruction. In our experience with over 500 knee allografts, we have found that successful clinical outcome is predicated on defining specific patient indications, including a definitive preoperative diagnosis (e.g., post-meniscectomy arthritis or posttraumatic arthritis vs. idiopathic osteoarthritis), with attention to all other confounding patient variables such as limb alignment and ligament status. Common indications for osteochondral allografting are listed in Box 7–1. This list defines a broad spectrum of clinical conditions; however, it is important to note that, as the extent of disease progresses into the realm of arthritis, the use of allografts becomes more controversial and the technical aspects more difficult, often including adjunct procedures such as osteotomy and ligament reconstruction or meniscal transplant.
In treatment of the “arthritic” patient who is considered for biologic restoration, the following diagnostic categories are relevant: osteonecrosis of the femoral condyle, either spontaneous or steroid-associated4; posttraumatic arthritis secondary to tibial plateau fracture malunion,5,6 femoral condyle fracture, or patella fracture; and cases of unicompartmental arthrosis of either the tibiofemoral joint7 or the patellofemoral joint.8,9 These conditions may be idiopathic but, in young patients, are more likely secondary to some underlying condition such as a remote meniscectomy or long-standing chondral injury. The allografting procedure may involve a single surface, such as the femoral condyle or tibial plateau, or a multifocal reconstruction such as the femoral condyle and trochlea or both medial and lateral femoral condyles or a so-called bipolar allograft, which includes resurfacing the tibia and femoral condyle in a single compartment. There are technical aspects of each of these allografts, but they are generally classified into plug or shell grafts. A plug graft is, essentially, a round graft prepared by commercially available instruments that form grafts between 15 and 35 mm in diameter. Shell grafts are more complex geometric shapes that must be prepared by hand. These are utilized for resurfacing the femoral condyle (particularly large or difficult to reach areas, such as the posterior condyle), patella, and tibial plateau. Table 7–1 outlines common diagnoses and allograft patterns.
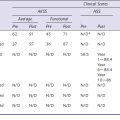
Table 7–1 Specific Allograft Reconstruction Options for Degenerative Knee Conditions
| Condition | Reconstruction Option |
|---|---|
| 1. Spontaneous osteonecrosis of the medial femoral condyle | Focal allograft, with or without high tibial osteotomy |
| 2. Steroid-associated osteonecrosis | Multiple plugs or shell graft |
| 3. Tibial plateau fracture malunion | Combined tibial plateau allograft and meniscal transplantation, with or without osteotomy |
| 4. Unicompartmental, tibiofemoral arthrosis (secondary to meniscectomy or repetitive chondral trauma) | – Realignment osteotomy, if indicated – Bipolar allograft (tibial plateau with meniscus and plug or shell femoral allograft) |
| 5. Patellofemoral arthrosis | Bipolar plug or shell allograft, with or without tibial tubercle osteotomy |
Setup and Equipment
The setup for osteochondral allografting of the knee is very similar to a unicompartmental arthroplasty.10,11 We prefer the use of regional blocks for postoperative pain management; however, the anesthesia is at the discretion of the surgeon and the anesthesiologist. A tourniquet is used in all cases, and the leg positioner is set so the knee can be placed in varying degrees of flexion (70–130°), which is critical for access to the pathologic lesion(s).
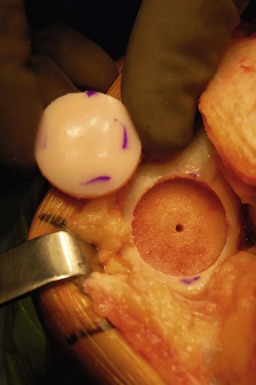
The key equipment issue regarding osteochondral allografting is the availability of the allograft tissue. Osteochondral allografts are size matched to the patient and obtained from an accredited tissue bank that is experienced in the recovery, testing, and processing of fresh osteochondral allografts. We prefer fresh, as opposed to frozen allografts, in order to maximize chondrocyte viability and, therefore, to maintain viable cartilage in the allograft in vivo.12,13 Prior to incision, the surgeon should inspect the allograft to ensure that it is the appropriate size and anatomic part for the proposed procedure. Commercially available instruments can be utilized for performing large, dowel-type allografts, typically on the femoral condyle (Fig. 7–1). However, in larger, degenerative conditions, the allograft must often be shaped in the freehand fashion, utilizing power equipment such as saws and burrs. Therefore, the surgeon should have the typical instrumentation utilized for a knee arthroplasty. Fluoroscopy is useful, particularly for tibial plateau allografts or for large femoral condyle allografts. Fixation of a dowel graft is achieved with press-fit, with or without the use of bioabsorbable pins or screws. Small screws, such as cannulated 3.0- or 3.5-mm screws, should be available to provide fixation for larger shell grafts.
Technical Description
Tibial Plateau Allografts (Figs. 7–7 through 7–13)
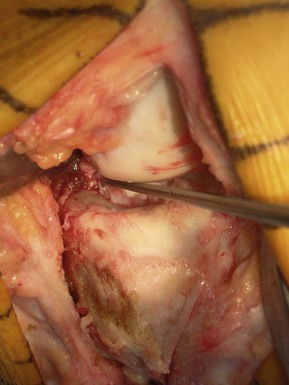
Tibial plateau allografts are particularly useful for reconstruction of posttraumatic problems, such as tibial plateau fractures.6 In this setting, the procedure is very similar to resurfacing of the tibial plateau in unicompartmental arthroplasty. After exposing the knee, it must be determined if the meniscus should be replaced. Most often, we replace the meniscus with the tibial plateau graft because meniscus pathology is almost universal in cases of posttraumatic or degenerative arthritis. After excising the meniscus remnant and determining the amount of bone loss from the involved plateau, the reciprocating saw is used to make a vertical cut and then, using either a unicompartmental knee jig or a freehand technique, a limited resection of the tibial plateau is made. This is important to consider, because frequently bone loss has led to a loss of plateau height that will be restored with the allograft. Over-resection of the tibial plateau should be avoided.
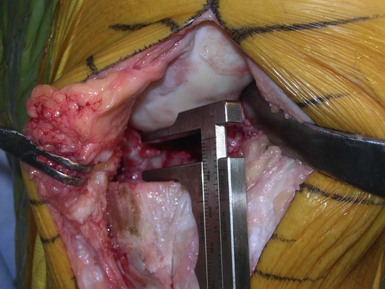
Figure 7–9 After resection of the plateau, the gap is measured to determine preliminary allograft thickness.
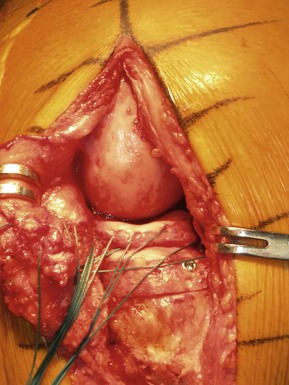
Bipolar Grafts (Figs. 7–14 through 7–19)
Single-compartment, reciprocal bipolar grafts for the treatment of unicompartmental arthritis or when both femoral and tibial surfaces are diseased are technically very challenging and should be used with great care.7,14 The technical aspects of each allograft have been outlined above. The sequence of events would be as follows: resection of the tibial surface, allowing for more access to the femoral side; preliminary preparation of the tibial graft, followed by allografting of the femoral condyle; and finally, insertion of the tibial allograft.
Special Considerations
The surgical techniques involved in osteochondral allografting are fairly straightforward, but the nuances of the biologic restoration can be daunting for inexperienced surgeons. It is important to have one or two scrubbed assistants to maintain the leg in an appropriate position for reconstruction and access to the lesions. It is important to confirm that the appropriate allograft material is on hand. The least amount of allograft material necessary for reconstruction should be used, and it should be noted that unipolar grafts (i.e., single-surface grafts) are far easier and have better outcomes than bipolar grafts.10 For this reason, in cases such as osteonecrosis of the femoral condyle, even if there is some articular cartilage disease of the tibial plateau, we would choose not to resurface the plateau. Conversely, in cases of tibial plateau disease with only modest femoral condyle articular cartilage disease, we would choose to reconstruct only the tibial plateau, rather than perform a bipolar graft. However, in those cases where exposed bone is present on both joint surfaces, it is appropriate to perform a bipolar allograft. In situations where malalignment or ligament deficiency is present, it is important to consider correction of these pathologies.
Tips and Pearls
1 Emmerson BC, Gortz S, Jamali AA, et al. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35:907-914.
2 Gortz S, Bugbee WD. Allografts in articular cartilage repair. J Bone Joint Surg [Am]. 2006;88:1374-1384.
3 Sgaglione NA, Chen E, Bert JM, et al. Current strategies for nonsurgical, arthroscopic, and minimally invasive surgical treatment of knee cartilage pathology. Instruct Course Lect. 2010;59:157-180.
4 Gortz S, De Young AJ, Bugbee WD. Fresh osteochondral allografting for steroid-associated osteonecrosis of the femoral condyles. Clin Orthop Relat Res. 2010;468:1269-1278.
5 Gross AE, Kim W, Las Heras F, et al. Fresh osteochondral allografts for posttraumatic knee defects: long-term followup. Clin Orthop Relat Res. 2008;466:1863-1870.
6 Shasha N, Krywulak S, Backstein D, et al. Long-term follow-up of fresh tibial osteochondral allografts for failed tibial plateau fractures. J Bone Joint Surg [Am]. 2003;85(Suppl 2):33-39.
7 Görtz S, De Young A, Bugbee WD. Fresh osteochondral allograft transplantation for biopolar cartilage lesions of the knee. Paper No 513, presented at the annual meeting of the American Academy of Orthopaedic Surgeons, Las Vegas, NV, February 25–28, 2009.
8 Jamali AA, Emmerson BC, Chung C, et al. Fresh osteochondral allografts: results in the patellofemoral joint. Clin Orthop Relat Res. 2005;437:176-185.
9 Torga Spak R, Teitge RA. Fresh osteochondral allografts for patellofemoral arthritis: long-term followup. Clin Orthop Relat Res. 2006;444:193-200.
10 Görtz S, Bugbee WD. Osteochondral grafts: diagnosis, operative techniques, clinical outcomes. In: Noyes FR, Barber-Westin SD, editors. Knee Disorders: Surgery, Rehabilitation, Clinical Outcomes. Philadelphia: Elsevier; 2010:948-960.
11 Dietrick TB, Bugbee WD, Fresh osteochondral allografting. 4th ed. Scott WN, editor, Insall & Scott Surgery of the Knee. Vol 2, 2006. Elsevier, Philadelphia, 405-419.
12 Czitrom AA, Keating S, Gross AE. The viability of articular cartilage in fresh osteochondral allografts after clinical transplantation. J Bone Joint Surg Am. 1990;72(4):574-581.
13 Williams SK, Amiel D, Ball ST, et al. Analysis of cartilage tissue on a cellular level in fresh osteochondral allograft retrievals. Am J Sports Med. 2007;35:2022-2032.
14 Park DY, Chung DB, Bugbee WD. Fresh osteochondral allografts for younger, active individuals with osteoarthrosis of the knee. Presented at the International Cartilage Repair Society (ICRS) Meeting, San Diego, CA, January 9–11, 2006.