Airway Clearance Techniques
I Definition: Airway clearance techniques include the use of invasive and noninvasive therapy to help mobilize and remove secretions and improve gas exchange.
II Airway Clearance Physiology
A Normal airway clearance (see Chapter 4)
1. Normal clearance of the airway depends on a patent airway, a functional mucociliary transport system, and an effective cough.
2. The mucociliary transport system functions from the larynx down to the respiratory bronchioles.
3. Goblet cells and submucosal glands are responsible for the majority of secretions in the central airways.
4. Ciliated epithelial cells in a coordinated wavelike motion move mucus toward the trachea and larynx where it can be swallowed or expectorated.
5. The normal respiratory tract produces approximately 100 ml of mucus per day.
B Four phases of normal cough reflex (Figure 36-1)
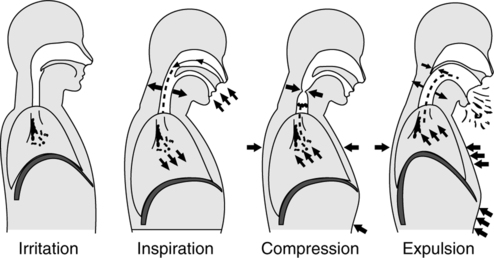
a. Inflammatory, mechanical, chemical, or thermal stimulus trigger airway sensory receptors, sending impulses to the brain’s medullary cough center.
a. In response to these afferent impulses the cough center reflexively stimulates the inspiratory muscles to initiate a deep inspiration.
1. Airway abnormalities that alter airway patency, mucociliary transport, or cough reflex may impede airway clearance and cause retention of secretions.
2. Mucous plugging can cause complete obstruction of the airway, resulting in atelectasis and impaired gas exchange because of shunting.
3. Partial obstruction from retained secretions restricts airflow, causing increased work of breathing, air trapping, overdistention, and ventilation/perfusion ( /
/ ) mismatch.
) mismatch.
4. Infectious processes caused by microorganisms in retained secretions cause an inflammatory response and the release of chemical mediators, resulting in increased mucus production.
5. Causes of impaired mucociliary transport in intubated patients
III Methods to Manage Thick Secretions
1. Bland aerosol therapy can be used for the management of thick, tenacious secretions in patients who have intact upper airways.
2. However, no studies have reported a benefit from external humidification in improving the character or mobilization of thick secretions.
3. Systemic hydration is the most effective method to improve the character of pulmonary secretions.
a. Approved for the management of cystic fibrosis
b. Delivered to the airway via small volume nebulizer
c. Efficacy not proven for acute exacerbations of cystic fibrosis or for the management of other chronic airway diseases
a. Delivered to the airway via small volume nebulizer or instillation into artificial airway
b. Has never been approved for inhalation
c. Few or no data to support its efficacy when nebulized
d. Can irritate the airway and induce bronchospasm
e. Effective when instilled into specific lung segments during bronchoscopy
A Suctioning through an artificial airway
b. Wheezing, rhonchi, or rales or decreased breath sounds
c. Unexplained increases in ventilator pressure during volume ventilation or decreases in tidal volume during pressure control ventilation
2. Sterile technique must be used when suctioning an artificial airway, except when an in-line suction catheter is used.
3. Preoxygenation can help minimize hypoxemia caused by suctioning.
4. The suction catheter should not remain in the airway for >15 seconds.
5. Sterile saline should not routinely be instilled into the airway. There is no evidence that this practice increases the amount of secretions removed from the airway, and it may worsen oxygenation. Sterile saline should only be used to help loosen exceptionally thick and tenacious secretions encountered during suctioning.
1. Patients with excessive secretions and a poor cough reflex may benefit from nasotracheal suctioning.
2. Placement of a nasopharyngeal airway may help to reduce trauma to the nasal passage from repeated suctioning.
a. Inability to clear secretions
b. Audible evidence of secretions in the large/central airways that persist despite patient’s best cough effort
1. Therapeutic bronchoscopy is used for the removal of foreign bodies from the airway, management of focal atelectasis, and airway occlusion caused by retained secretions.
2. There is limited evidence that routine bronchoscopy for removal of retained secretions provides any greater benefit than suctioning and chest physiotherapy techniques.
3. Bronchoscopy is beneficial for the removal of secretions from the airway for diagnostic testing purposes.
V Noninvasive Bronchial Hygiene
1. Postural drainage is a method of removing pooled secretions by positioning the patient to allow gravity to assist in movement of secretions. The patient should be positioned so that the affected lung segments are superior to the carina, with each position maintained for 3 to 15 minutes.
2. Indications (Modified from AARC Clinical Practice Guideline: Postural Drainage, 1991)
a. Inability or reluctance of patient to change body position
b. Poor oxygenation associated with position (e.g., unilateral lung disease)
c. Potential for or presence of atelectasis
d. Presence of artificial airway
e. Evidence or suggestion of difficulty with secretion clearance
f. Difficulty clearing secretions, with expectorated sputum production >25 to 30 ml/day (for an adult)
g. Evidence or suggestion of retained secretions in the presence of an artificial airway
h. Presence of atelectasis caused by or suspected of being caused by mucous plugging
i. Diagnosis of diseases such as cystic fibrosis, bronchiectasis, or cavitating lung disease
j. Presence of foreign body in airway
k. External manipulation of the thorax: Sputum volume or consistency suggesting a need for additional manipulation
3. Contraindications (Modified from AARC Clinical Practice Guideline: Postural Drainage, 1991)
a. The decision to use postural drainage therapy requires assessment of potential benefits versus potential risks. Therapy should be provided for no longer than necessary to obtain the desired therapeutic results. Listed contraindications are relative unless marked as absolute (A).
b. Positioning: All positions are contraindicated for
(1) Head and neck injury until stabilized (A)
(2) Active hemorrhage with hemodynamic instability (A)
(4) Recent spinal surgery or acute spinal injury
(8) Pulmonary edema associated with congestive heart failure
(9) Aged, confused, or anxious patients who do not tolerate position changes
(11) Rib fracture, with or without flail chest
c. Trendelenburg position is contraindicated for
(1) Recent gross hemoptysis related to recent lung carcinoma managed surgically or with radiation therapy
(5) Patients in whom increased ICP is to be avoided (e.g., neurosurgery, aneurysms, or eye surgery)
(6) Uncontrolled airway at risk for aspiration (e.g., tube feeding or recent meal)
d. External manipulation of the thorax (in addition to contraindications previously listed)
4. Hazards and complications (Modified from AARC Clinical Practice Guideline: Postural Drainage, 1991)
5. Standard postural drainage positions for each of the lung segments
a. Apical segments of right and left upper lobes: Patient in semi-Fowler’s position with head of the bed raised 45 degrees (Figure 36-2).
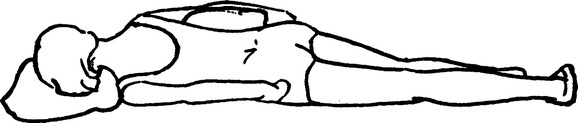
b. Anterior segments of both upper lobes: Patient supine with the bed flat (Figure 36-3).
c. Posterior segments of right upper lobe: Patient one-quarter turn from prone with the right side up, supported by pillows, and with head of the bed flat (Figure 36-4).
d. Apical-posterior segment of left upper lobe: Patient one-quarter turn from prone with the left side up, supported by pillows, and with head of the bed elevated 30 degrees (Figure 36-5).
e. Medial and lateral segments of right middle lobe: Patient one-quarter turn from supine with right side up and foot of the bed elevated 12 in. (Figure 36-6).
f. Superior and inferior segments of lingula: Patient one-quarter turn from supine with left side up and foot of the bed elevated 12 in. (Figure 36-7).
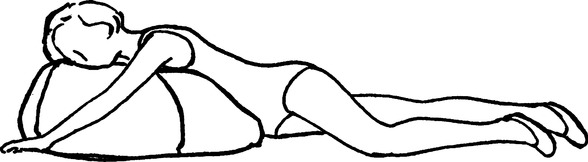
g. Superior segments of both lower lobes: Patient prone with head of the bed flat and pillow under the abdominal area (Figure 36-8).
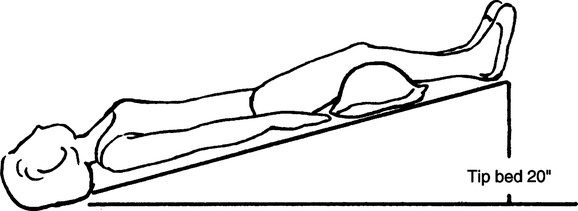
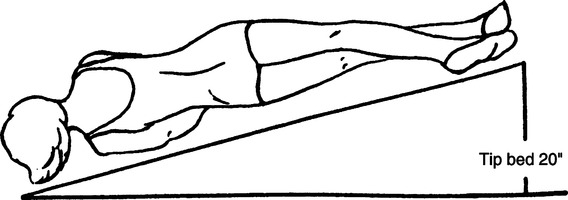
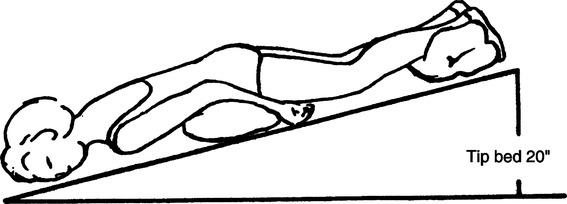
h. Anteromedial segment of left lower lobe and anterior segment of right lower lobe: Patient supine, with foot of the bed elevated 20 in. (Figure 36-9).
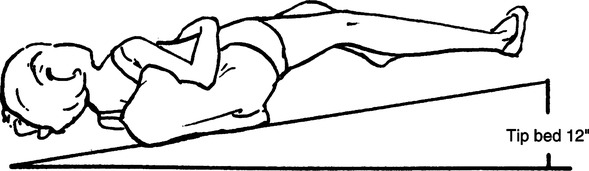
i. Lateral segment of right lower lobe: Patient directly on left side with right side up and foot of the bed elevated 20 in. (Figure 36-10).
j. Lateral segment of left lower lobe and medial (cardiac) segment of right lower lobe: Patient directly on right side, with left side up and foot of the bed elevated 20 in. (Figure 36-11).
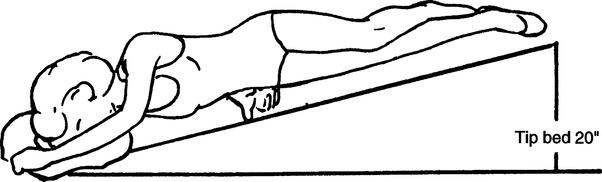
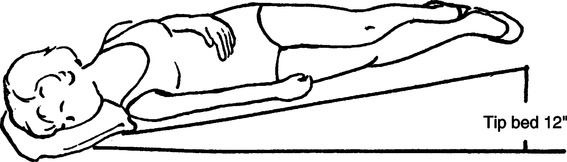
k. Posterior segment of both lower lobes: Patient prone with foot of the bed elevated 20 in. (Figure 36-12).
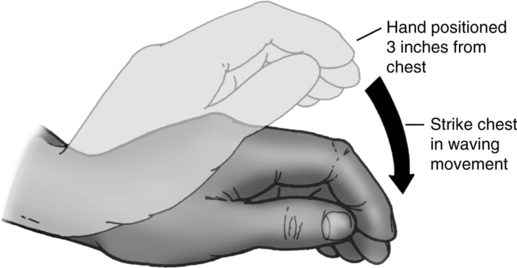
1. Percussion is a technique of rhythmically tapping the chest wall with cupped hands or mechanical device. No convincing evidence demonstrates the superiority of one method over the other. It is designed to loosen secretions in the area underlying the percussion by the air pressure that is generated by the cupped hand on the chest wall. Percussion is performed during inspiration and expiration (Figure 36-13).
2. There is no evidence that percussion alone increases the amount of secretions removed from the airway. Select patients may benefit if percussion is added to postural drainage therapy.
3. If percussion is performed care must be taken to carefully monitor the patient’s cardiopulmonary status throughout the procedure.
4. Indications (same as those for postural drainage)
5. Percussion may be contraindicated in patients with the following conditions.
a. Cancer with known metastatic changes
h. Wounds, skin grafts, and burns
6. Hazards and complications (same as those for postural drainage)
1. Vibration involves the application of a fine tremorous action (manually performed by pressing in the direction that the ribs and soft tissue of the chest move during expiration) over the draining area. Vibrations are intended to move secretions into the larger airways. No conclusive evidence supports the efficacy of vibration, the superiority of either manual or mechanical methods, or an optimum frequency.
2. Indications, possible contraindications, hazards, and complications are the same as postural drainage and percussion.
1. Directed cough (DC) to clear or mobilize secretions is a component of bronchial hygiene therapy when spontaneous cough is inadequate.
2. DC is a deliberate maneuver that is taught, supervised, and monitored. It attempts to mimic an effective spontaneous cough, to assist in voluntary control of the cough reflex, and to compensate for physical limitations that impair this reflex.
3. Forced expiratory technique (FET), or huff coughing, and manually assisted cough are examples of DC.
4. Indications (Modified from AARC Clinical Practice Guideline: Directed Cough, 1993)
a. The need to aid in the removal of retained secretions from central airways
b. The presence of atelectasis
c. Prophylaxis against postoperative pulmonary complications
d. Routine part of bronchial hygiene in patients with cystic fibrosis, bronchiectasis, chronic bronchitis, necrotizing pulmonary infection, or spinal cord injury
e. Integral part of other bronchial hygiene therapies, such as postural drainage therapy (PDT), positive expiratory pressure therapy (PEP), and incentive spirometry (IS)
5. Contraindications (Modified from AARC Clinical Practice Guideline: Directed Cough, 1993)
a. DC is rarely contraindicated. The contraindications listed must be weighed against potential benefit in deciding to eliminate cough from the care of the patient. Listed contraindications are relative.
(1) Inability to control possible transmission of infection from patients suspected or known to have pathogens transmittable by droplet nuclei (e.g., M. tuberculosis)
(2) Presence of an elevated ICP or known intracranial aneurysm
(3) Presence of reduced coronary artery perfusion, such as in acute myocardial infarction
b. Manually assisted DC with pressure to the epigastrium may be contraindicated in the presence of
(1) Increased potential for regurgitation/aspiration (e.g., unconscious patient with unprotected airway)
(2) Acute abdominal pathology, abdominal aortic aneurysm, hiatal hernia, or pregnancy
c. Manually assisted DC with pressure to the thoracic cage may be contraindicated in the presence of
6. Hazards/complications (Modified from AARC Clinical Practice Guideline: Directed Cough, 1993)
a. Reduced coronary artery perfusion
b. Reduced cerebral perfusion leading to syncope or alterations in consciousness, such as lightheadedness or confusion and vertebral artery dissection
h. Muscular damage or discomfort
i. Spontaneous pneumothorax, pneumomediastinum, and subcutaneous emphysema
l. Rib or costochondral juncture fracture
m. Incisional pain, evisceration
n. Anorexia, vomiting, and retching
7. DC is of limited value in the obtunded, paralyzed, or uncooperative patient.
8. The following clinical entities may compromise the effectiveness of a DC maneuver.
a. The presence of severe obstructive airway disease
c. Pain exacerbated by coughing
9. In patients with a bypassed upper airway or other conditions that preclude the ability to effectively close the glottis, the effectiveness of the cough may be limited.
10. Thick, tenacious sputum may limit the effectiveness of the techniques and may require other supplemental strategies to optimize clearance of secretions.
a. Instruct patient to take three to five slow deep breaths, inhaling through the nose, exhaling through pursed lips, and using diaphragmatic breathing.
b. Ask the patient to take a deep breath and hold for 1 to 3 seconds.
c. Exhale rapidly from mid lung volumes to low lung volumes to clear secretions from periphery.
d. Take in normal breath, and contract the abdominal and chest wall muscles with the mouth (and glottis) open while whispering the word “huff.” Repeat several times.
e. As secretions enter the larger airways, exhale rapidly from high to mid lung volumes to clear secretions from the more proximal airways. Repeat maneuver two or three times.
f. Take several relaxed diaphragmatic breaths before the next cough.
g. Manually assisted cough can be used by applying mechanical pressure to the epigastric region or thoracic cage with a forced exhalation.
1. The active cycle of breathing (ACB) is a modification of the FET maneuver. It has three stages: breathing control, thoracic expansion control, and FET.
2. Indications, contraindications, hazards, and complications are similar to those of DC.
a. Position patient properly, either relaxed sitting or reclined position.
b. Breathing control: Several minutes of relaxed diaphragmatic breathing
c. Thoracic expansion: Three or four active deep inspirations with passive relaxed exhalation
d. Relaxed diaphragmatic breathing
e. FETs: As the patient feels secretions enter the larger central airway, two or three huffs followed by relaxed breathing control are performed.
1. Autogenic drainage is another modification of DC. Three phases of staged breathing at different lung volumes are performed until secretions are felt in the central airway. Several huff coughs at this point help to remove the secretions.
2. Indications, contraindications, hazards, and complications are similar to those of DC.
3. This technique requires a great deal of patient cooperation. It is recommended for patients aged ≥8 years.
1. Exercise has been shown to increase sputum production compared with rest. Exercise should be encouraged, as tolerated, to augment bronchial hygiene.
1. Cough assistance is indicated for the patient who cannot develop a forceful cough.
2. Cough assistance can be performed by
a. Applying pressure to the upper abdominal area during the compression and expiratory phase of the cough.
b. For patients with an artificial airway this is done by hyperinflating the lung with a manual ventilator, holding gas volume in the lung at end of inspiration, and then rapidly releasing pressure, allowing exhalation, while an associate applies vigorous chest wall compression in an inward and downward fashion. Care should be taken to follow the normal anatomic movement of the chest.
I Breathing instruction and retaining
1. These techniques are designed to assist patients with muscular weakness, postoperative pain, or chronic pulmonary disease to assume an efficient ventilatory pattern and effective cough.
a. To increase and improve ventilation
b. To strengthen respiratory musculature
c. To prevent development of atelectasis
a. Diaphragmatic breathing exercises
(1) The therapist and patient locate the xiphoid process. The patient is instructed to “sniff” to determine the location of the diaphragm.
(2) The patient is relaxed, supported with a pillow, and directed to inspire by contracting the diaphragm slowly and completely to allow a normal inspiratory pattern.
(3) The patient is encouraged to exhale slowly, passively, and completely. The therapist may assist exhalation by exerting a slight inward and upward pressure below the xiphoid process.
b. Lateral costal expansion exercises
(1) The therapist places his or her hands over the patient’s lower rib cage with the thumbs just above the xiphoid process.
(2) The patient is encouraged to relax and inspire against a slight pressure exerted by the therapist’s hands. The patient is instructed to try to expand the area located under the therapist’s hands.
(3) Exhalation should be passive but complete. The therapist can assist exhalation by applying an inward and downward pressure during exhalation.
c. Localized expansion exercises designed to direct the gas flow to a specific area of the lung
(1) The therapist places his or her hands over the problem area and instructs the patient to inspire against a slight pressure exerted by the therapist.
(2) Exhalation should be passive, complete, and assisted by the therapist. The therapist exerts an inward and downward force during exhalation, following the natural movement of the rib cage.
VI Mechanical Aids to Bronchial Hygiene and Lung Expansion
A Intermittent positive pressure breathing (IPPB)
1. IPPB is a technique used to provide short-term or intermittent mechanical ventilation for the purpose of augmenting lung expansion, delivering aerosol medication, clearing retained secretions, or assisting ventilation.
2. IPPB is usually administered using a pneumatically driven, pressure-triggered, and pressure-cycled ventilator (Figure 36-14).
3. IPPB may be delivered to artificial airways and nonintubated patients.
4. IPPB should not be the first choice to deliver aerosol or as a method of lung expansion in spontaneously breathing patients who are capable of using other less expensive but clinically comparative methods.
5. Indications (Modified from AARC Clinical Practice Guideline: Intermittent Positive Pressure Breathing, 2003)
a. The need to improve lung expansion
(1) The presence of clinically significant pulmonary atelectasis when other forms of therapy have been unsuccessful (e.g., IS, chest physiotherapy, deep breathing exercises, or positive airway pressure) or the patient cannot cooperate
(2) Inability to clear secretions adequately because of pathology that severely limits the ability to ventilate or cough effectively and failure to respond to other modes of treatment
b. The need for short-term ventilatory support for patients who are hypoventilating as an alternative to tracheal intubation and continuous mechanical ventilation. Devices specifically designed to deliver noninvasive positive pressure ventilation (NPPV) should be considered first (see Chapter 43).
c. The need to deliver aerosol medication. (This is a highly controversial indication. The data indicate that IPPB adds no additional benefit to the spontaneous inhalation of aerosolized medication.)
(1) Some clinicians oppose the use of IPPB for the management of severe bronchospasm (e.g., acute asthma or status asthmaticus and exacerbated chronic obstructive pulmonary disease [COPD]); however, a careful, closely supervised trial of IPPB as a medication-delivery device when treatment using other techniques (e.g., metered dose inhaler or nebulizer) has been unsuccessful may be warranted.
(2) IPPB may be used to deliver aerosol medications to patients with fatigue as a result of ventilatory muscle weakness (e.g., failure to wean from mechanical ventilation, neuromuscular disease, kyphoscoliosis, or spinal injury) or chronic conditions in which intermittent ventilatory support is indicated (e.g., ventilatory support for home care patients and the more recent use of nasal positive pressure ventilation for respiratory insufficiency).
(3) For patients with severe hyperinflation IPPB may decrease dyspnea and discomfort during nebulized therapy.
6. Contraindications (Modified from AARC Clinical Practice Guideline: Intermittent Positive Pressure Breathing, 2003)
a. There are several clinical situations in which IPPB should not be used. With the exception of untreated tension pneumothorax, most of these contraindications are relative.
7. Hazards/complications (Modified from AARC Clinical Practice Guideline: Intermittent Positive Pressure Breathing, 2003)
a. Increased airway resistance and work of breathing
f. Hyperoxia when oxygen is the gas source
h. Impaction of secretions (associated with inadequately humidified gas mixture)
l. Hypoventilation or hyperventilation
m. Increased mismatch of ventilation and perfusion
n. Air trapping, auto-positive end-expiratory pressure, or overdistended alveoli
1. IS is designed to mimic natural sighing or yawning by encouraging the patient to take long, slow, deep breaths.
2. The apparatus acts purely as a visual motivator encouraging patient effort and compliance.
3. The IS maneuver consists of a sustained, maximal inspiration (SMI), followed by a 5- to 10-second breath-hold. Patients should be encouraged to take 5-10 breaths every hour.
4. The goals of IS are to increase transpulmonary pressure and inspiratory volumes, improving inspiratory muscle performance, and reestablishing or simulating the normal pattern of pulmonary hyperinflation.
5. Indications (Modified from AARC Clinical Practice Guideline: Incentive Spirometry, 1991)
a. Presence of conditions predisposing to the development of pulmonary atelectasis
b. Presence of pulmonary atelectasis
c. Presence of a restrictive lung defect associated with quadriplegia and/or dysfunctional diaphragm
6. Contraindications (Modified from AARC Clinical Practice Guideline: Incentive Spirometry, 1991)
a. Patient cannot be instructed or supervised to ensure appropriate use of the device.
b. Patient cooperation is absent, or patient is unable to understand or demonstrate proper use of the device.
c. Patients unable to deep breathe effectively (e.g., with vital capacity less than approximately 10 ml/kg or inspiratory capacity less than approximately one third of predicted)
d. Presence of an open tracheal stoma is not a contraindication but requires adaptation of the spirometer.
7. Hazards and complications (Modified from AARC Clinical Practice Guideline: Incentive Spirometry, 1991)
a. Ineffective unless closely supervised or performed as ordered
b. Inappropriate as sole therapy for major lung collapse or consolidation
e. Discomfort secondary to inadequate pain control
f. Hypoxia secondary to interruption of prescribed oxygen therapy if face mask or shield is used
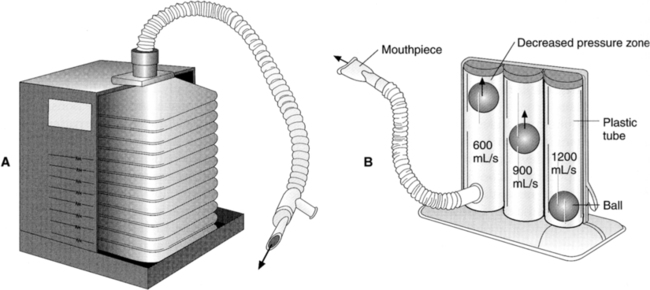
a. Flow oriented (Figure 36-15, B)
(1) The patient’s inspiratory flow rate causes a float or ball to rise in a canister. The float or ball remains suspended for a sustained period.
(2) The patient should maintain an inspiratory flow that slowly elevates the float.
(3) A rapid inspiration will cause the float to rise quickly but will not maintain it in a suspended position.
(4) Slow inspirations do not generate sufficient flow to raise the float.
A Positive airway pressure therapy (PAP) is used to mobilize secretions and manage atelectasis. The three adjuncts to PAP are continuous positive airway pressure (CPAP), positive expiratory pressure (PEP), and expiratory positive airway pressure (EPAP).
B Studies have shown that PAP therapy is most effective when combined with cough or other airway clearance techniques.
C CPAP therapy requires the patient to breathe from a pressurized circuit against a threshold resistor that maintains consistent preset airway pressures from 5 to 20 cm H2O (Figure 36-16).
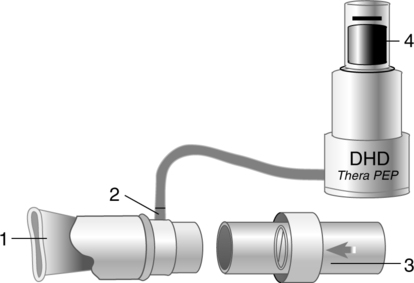
D PEP therapy requires the patient to exhale against a fixed-orifice resistor, generating pressures during expiration that usually range from 10 to 20 cm H2O (Figure 36-17).
E EPAP therapy requires the patient to exhale against a threshold resistor, generating preset pressures of 10 to 20 cm H2O.
F Indications (Modified from AARC Clinical Practice Guideline: Use of Positive Airway Pressure Adjuncts to Bronchial Hygiene Therapy, 1993)
1. To reduce air trapping in patients with asthma and COPD
2. To aid in mobilization of retained secretions in those with cystic fibrosis and chronic bronchitis
3. To prevent or reverse atelectasis
4. To optimize delivery of bronchodilators in patients receiving bronchial hygiene therapy
G Contraindications (Modified from AARC Clinical Practice Guideline: Use of Positive Airway Pressure Adjuncts to Bronchial Hygiene Therapy, 1993)
1. Patients unable to tolerate the increased work of breathing (e.g., those with acute asthma or COPD)
4. Recent facial, oral, or skull surgeries or trauma
10. Known or suspected tympanic membrane rupture or other middle ear pathology
H Hazards and complications (Modified from AARC Clinical Practice Guideline: Use of Positive Airway Pressure Adjuncts to Bronchial Hygiene Therapy, 1993)
VIII Mechanical Insufflation/Exsufflation (MIE)
A MIE is indicated for patients with decreased cough ability (e.g., those with neuromuscular disorders). Its purpose is to simulate a spontaneous cough (Figure 36-18).

B A positive pressure breath is delivered at 30 to 50 cm H2O for 1 to 3 seconds via an oronasal mask or artificial tracheal airway. A negative pressure of −30 to −50 cm H2O follows this for 2 or 3 seconds to stimulate a cough.
C This process is repeated with breaks for spontaneous or assisted breathing until secretions are cleared from the airway.
D The expiratory flow remains high immediately after exsufflation, indicating that MIE does not promote airway collapse.
E Although studies have found this to be a useful adjunct for patients with neuromuscular disease, there is no evidence of its effectiveness in critically ill patients.
IX High Frequency Oscillation of the Airway
A High frequency oscillation of the airway (HFOA) is the rapid vibratory movement of small volumes of air produced by either a mechanical device or the patient’s own expiration with an oscillatory device.
B HFOA has been shown to increase mucous clearance by altering mucous rheology and enhancing mucous-airflow interaction and reflex mechanisms.
C HFOA methods include the flutter valve and intrapulmonary percussive ventilation (IPV).
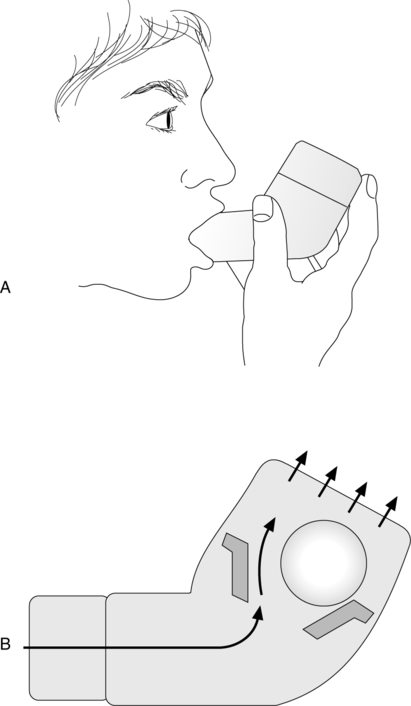
a. The flutter valve is a mucous clearance device that combines the technique of PEP with high frequency oscillations at the airway opening.
b. It is pipe shaped with a steel ball in the bowl covered by a cap. When the patient exhales actively into the device, the ball creates a positive pressure between 10 and 25 cm H2O and generates oscillations of approximately 15 Hz (Figure 36-19).
c. It may decrease mucous viscoelasticity within the airways, thus modifying mucus and allowing it to be cleared.
d. To use the flutter valve, instruct the patient to sit comfortably and take in a breath slightly larger than normal. Place the flutter in the mouth, seal lips, and the patient exhales actively but not forcefully. Do this for 10 to 20 breaths.
e. There are few data on its efficacy, but it has been shown to be of benefit for patients with cystic fibrosis.
a. IPV is a form of chest physiotherapy (CPT) that uses a pneumatic device to deliver pressurized gas minibursts at rates of 100 to 225 cycles/min to the respiratory tract via a mouthpiece. Normal treatment time is 20 minutes.
b. IPV can be used to manage atelectasis, enhance the mobilization and clearance of retained secretions, and deliver nebulized medications to the distal airways.
c. Limited data reported show that IPV may be comparable with the results of standard CPT.
X High Frequency Chest Wall Oscillation
A High frequency chest wall oscillation (HFCWO) is a noninvasive form of oscillation that uses an air-pulse generator and a nonstretch inflatable vest that covers the patient’s torso.
B HFCWO methods include the ThAIRapy Vest and the Hayek oscillator.
a. The ThAIRapy Vest is an airway clearance device that consists of an inflatable vest connected to an air-pulse generator. The generator rapidly inflates and deflates the vest, which helps move mucus toward the large airways, where it can be cleared by coughing.
b. The frequency of oscillations and flow bias are variable and it is important to determine optimal settings for maximal effectiveness.
c. The data show the ThAIRapy Vest is effective for secretion clearance in patients with cystic fibrosis.
a. The Hayek oscillator is an electrically powered, noninvasive ventilator that uses a chest cuirass to apply negative and positive pressure to the chest wall, which delivers oscillations to the lungs.
b. Frequency, inspiration/expiration ratio, inspiratory pressure, and expiratory pressure are variable settings and it is important to determine optimal settings for maximal effectiveness.
c. Limited data on the efficacy of the Hayek oscillator are available.