Airway Clearance Techniques
Evidence for the use of airway clearance techniques is often difficult to evaluate, in part due to agreement that top-level evidence on this topic is lacking.1a–b The components of a given treatment have not been standardized and the literature refers to ACTs using a variety of terms, including chest physiotherapy, chest physical therapy (CPT), bronchial drainage, postural drainage (PD) therapy, and bronchial hygiene. In addition, the availability of equipment and cultural differences in its application confound research results. Differences in the outcome measures for a given technique also occur—some studies use wet or dry (dehydrated) sputum volume or radioaerosol clearance, whereas other studies use pulmonary function tests, radiographic evidence, or arterial blood gases to asses the effectiveness of a specific technique. The majority of secretion clearance research has been focused on patients with cystic fibrosis, as the need for ongoing secretion removal is apparent in this population. However, results showing a treatment to be effective in one cross section of patients must not be generalized to apply to the treatment across all patients with pulmonary disease.
Historically, the gold standard of airway clearance has been a combination of postural drainage, percussion, and vibration with cough. This has been challenged1b–c as more techniques have been demonstrated to be effective. Postural drainage and percussion have been shown to be ineffective in some cases and, in fact, to be detrimental to pulmonary status in others. Caregivers have also been shown to suffer from the performance of percussion; repetitive-motion injuries of the wrists have been documented as a result of regular performance of percussion.2,3
Alternative techniques have arisen out of the need to find effective methods for those patients not responsive to traditional methods. A desire to increase adherence with airway clearance, especially in patients approaching adolescence and adulthood, has led to an investigation of more independent techniques.4 Many of these techniques have been practiced longer in other countries, but are now commonly used by practitioners in the United States.
It is important to remember, however, that secretion clearance is just one step toward realizing effective gas exchange in the complex oxygen transport pathway.5 Airway clearance, when indicated, should be integrated into a comprehensive plan of care, including positioning and mobilization, to optimize oxygen transport.
Conditions That May Indicate Airway Clearance
Oxygen transport is the primary purpose of the cardiopulmonary system (see Chapter 2). Ventilation of the alveoli is an important step in the oxygen transport chain; it allows optimal delivery of oxygen to the tissues. Several medical and surgical conditions may interfere with this process. Retained secretions or mucus plugs in the airways may interfere with the exchange of oxygen. The secretions must be mobilized from the peripheral, or smaller, airways to the larger, more central airways, where coughing or suction may remove them.
Cystic Fibrosis
In this multisystem genetic disease of exocrine gland dysfunction, copious (often purulent), thick secretions and mucus plugs block the peripheral and central airways. Even infants diagnosed with cystic fibrosis, whether symptomatic or not, show evidence of small airway obstruction in the form of bronchial mucus casts.6 Recurrent bacterial infections combined with this mucus hypersecretion in the lungs leads to destruction of the bronchial walls, or bronchiectasis. Airway clearance is recommended for all patients with CF and continues to be an important therapy in the treatment of cystic fibrosis.1b,6a This practice is supported by evidence of deteriorating lung function when regular treatments of postural drainage and percussion have been stopped.7,8
Bronchiectasis
This condition results in a breakdown of the elastic tissue in the bronchial walls, causing severe dilation. Inflamed mucosa and copious purulent secretions are present in this condition. Airway clearance has been shown to benefit patients with bronchiectasis in the mobilization of sputum.9,10
Atelectasis
This condition is caused by the collapse of alveolar segments, often by retained pulmonary secretions. It has been documented in patients who have undergone surgery under general anesthesia, especially in cases of thoracic or abdominal surgery. ACTs are indicated in cases of atelectasis due to mucus plugging.11,12
Respiratory Muscle Weakness
Many patients with neurological or metastatic diseases or general debilitation tend to hypoventilate or have increased work of breathing. They are unable to maintain adequate control of respiratory secretions and often have weak, ineffective coughing mechanisms.13 This is especially true in patients with diminished diaphragm innervation resulting from spinal cord injuries.14
Mechanical Ventilation
Patients requiring ventilatory support for any reason, including patients who are obtunded or comatose, are at risk for atelectasis and are unable to manage their secretions independently.15 Airway clearance is considered standard practice in the management of patients on mechanical ventilation.15a
Neonatal Respiratory Distress Syndrome
These infants are born lacking surfactant in the lungs, which results in atelectasis. ACTs may be useful in clearing secretions and preventing atelectasis, but there should be a clear indication for this procedure and it must be monitored carefully in this population.16,17
Asthma
This condition is characterized by the presence of hyperreactive airways and mucus plugging. ACTs may be beneficial to assist in the mobilization of mucus plugs but are not helpful in treating uncomplicated acute exacerbations.18
There are several conditions that do not appear to benefit from ACTs. Patients with pneumonia or chronic bronchitis without large amounts of secretion production do not appear to benefit from airway clearance. No differences in outcome were found when these populations were treated with postural drainage and percussion.19–22 Viral bronchiolitis is an asthma-like lung disease occurring in infants less than 2 years of age. These patients do not appear to benefit from ACTs.23 Also of little benefit, and possibly harmful, is the inclusion of airway clearance in the routine care of postoperative patients without extensive secretions.18 Even in patients with a history of lung disease, the use of ACTs has failed to affect the incidence of atelectasis as a postoperative complication.24
Airway Clearance Techniques
Exercise for Airway Clearance
In addition to improving many outcomes in patients with lung disease, exercise has been shown to assist in secretion clearance.25–28 Exercise increases mucociliary transport in patients with chronic bronchitis.28 Higher transpulmonary pressure with aerobic exercise may open closed bronchi, as well as increase collateral ventilation to allow mucus to be moved.26 It has also been shown that exercise-induced hyperventilation is more effective than eucapnic hyperventilation in mobilizing bronchial secretions.29 The contribution of increased expiratory airflow and exercise-induced coughing are other factors in improving secretion removal. Exercise for secretion clearance has focused on aerobic or endurance exercise; however, any form of exercise must be adapted to the individual patient’s status and abilities.
Based on a lack of decrease in lung function following the cessation of PD and percussion but the continuation of an exercise program, or based on the improvement in pulmonary function, exercise has been recommended as a replacement for a conventional chest physiotherapy routine in some patients or at some stages of lung disease.26,27,30,31 In hospitalized patients with cystic fibrosis, no significant change in pulmonary function was reported when exercise was substituted for two of three daily treatments of PD, percussion, and vibration, and the weight of the sputum produced was equivalent.30 In terms of mucus cleared, no significant differences were found among exercise on a cycle ergometer, postural drainage, and PEP mask breathing.32 Increases in sputum expectoration on exercise days as opposed to nonexercise days have also been reported.27,33
However, other studies conclude that exercise alone is not sufficient and recommend its use as a complement to other forms of airway clearance. Airway clearance using PD and FET was shown to be more effective than exercise with a cycle ergometer in inducing sputum expectoration.34 Results from Bilton and colleagues35 demonstrated that any modality that included the active cycle of breathing technique (ACBT) in PD positions alone or in combination with exercise is better than exercise alone at clearing sputum.
It is difficult to compare these studies, however, because the mode and length of exercise differ, as do the outcome measures of effectiveness of airway clearance. Exercise as an airway clearance technique is not suitable for the very young (younger than 4 to 5 years of age), for patients with neuromuscular limitations, or for patients with limited exercise tolerance. Moreover, the potential need for supplemental oxygen during exercise should be monitored. Nonetheless, evidence suggests that an exercise program, in addition to clearing secretions, may decrease morbidity and mortality by improving exercise capacity.36,37
Treatment with Exercise
 A walking program requires only a suitable pair of shoes and a safe location. Higher-impact exercise, because of increased stress on the knees, requires shoes specifically for that purpose. Clothing should be appropriate for the weather if exercising outdoors.
A walking program requires only a suitable pair of shoes and a safe location. Higher-impact exercise, because of increased stress on the knees, requires shoes specifically for that purpose. Clothing should be appropriate for the weather if exercising outdoors.
 Exercise equipment suitable for a patient who is beginning an exercise program includes the treadmill, bicycle ergometer, elliptical trainer, mini-trampoline, or arm ergometer. For more accomplished exercisers or patients with a higher exercise tolerance, equipment may include a stair climber, cross-country ski machine, or rowing machine. Numerous other exercise equipment options are available; the patient’s interests should be the primary factor for choosing.
Exercise equipment suitable for a patient who is beginning an exercise program includes the treadmill, bicycle ergometer, elliptical trainer, mini-trampoline, or arm ergometer. For more accomplished exercisers or patients with a higher exercise tolerance, equipment may include a stair climber, cross-country ski machine, or rowing machine. Numerous other exercise equipment options are available; the patient’s interests should be the primary factor for choosing.
 Tools to monitor a patient’s response to exercise include a sphygmomanometer, stethoscope, heart rate monitor, pulse oximeter, and a scale to measure patient’s level of perceived exertion (Figure 21-1). In a home setting, patients should be knowledgeable in self-monitoring exercise intensity. For those patients who require closer monitoring, a pulse oximeter may be rented from an oxygen supply company. Monitoring of vital signs before and during exercise, and during recovery, will allow titration of the workload for optimal performance.
Tools to monitor a patient’s response to exercise include a sphygmomanometer, stethoscope, heart rate monitor, pulse oximeter, and a scale to measure patient’s level of perceived exertion (Figure 21-1). In a home setting, patients should be knowledgeable in self-monitoring exercise intensity. For those patients who require closer monitoring, a pulse oximeter may be rented from an oxygen supply company. Monitoring of vital signs before and during exercise, and during recovery, will allow titration of the workload for optimal performance.
 Supplemental oxygen and oxygen delivery supplies will be necessary for those patients who exhibit oxygen desaturation during exercise.
Supplemental oxygen and oxygen delivery supplies will be necessary for those patients who exhibit oxygen desaturation during exercise.
 Patients with hyperreactive airways should be premedicated with a prescribed bronchodilator before an exercise session.
Patients with hyperreactive airways should be premedicated with a prescribed bronchodilator before an exercise session.
 The principles of an exercise prescription addressing mode, intensity, duration, and frequency, as well as principles of “warm up” and “cool down,” should be followed when using exercise as a form of airway clearance. Individualizing an exercise program for each patient is of the utmost importance.
The principles of an exercise prescription addressing mode, intensity, duration, and frequency, as well as principles of “warm up” and “cool down,” should be followed when using exercise as a form of airway clearance. Individualizing an exercise program for each patient is of the utmost importance.
 Patients hospitalized for an acute exacerbation may not be able to initially perform endurance exercise. These patients should be started slowly and progressed as tolerated; consider using interval training.
Patients hospitalized for an acute exacerbation may not be able to initially perform endurance exercise. These patients should be started slowly and progressed as tolerated; consider using interval training.
 The patient should be instructed in huffing or controlled coughing to expectorate secretions as they are loosened.
The patient should be instructed in huffing or controlled coughing to expectorate secretions as they are loosened.
 A regular, consistent program of exercise should be scheduled around the patient’s daily activities to achieve adherence (e.g., walking the dog, sports at school, stopping by the health club after work).
A regular, consistent program of exercise should be scheduled around the patient’s daily activities to achieve adherence (e.g., walking the dog, sports at school, stopping by the health club after work).
Advantages and Disadvantages of Exercise
Exercise has the advantage of being the only airway clearance technique that is performed regularly by people without lung disease. This factor can make it appealing to those patients who do not want to call attention to their differences from their peers. Exercise may improve self-esteem, a sense of well-being, and quality of life. Higher levels of exercise tolerance in patients with cystic fibrosis have been demonstrated to improve survival.37
Some patients may not tolerate the amount or frequency of exercise necessary for this to be the sole method of airway clearance. Thus various airway clearance techniques can be used as adjuncts to exercise. This is particularly true during an acute exacerbation when activity tolerance is limited, or in infants or patients with neurological or musculoskeletal limitations. Andreasson26 observed that regular contact with a caregiver seems to be necessary for successful exercise training, as does family support, especially in young children. This points out the difficulty with adherence to a home program. Adherence will also be affected by a patient’s preference for a particular activity, scheduling conflicts, and commitment by friends and family members.
Precautions for Using Exercise
Several precautions must be observed when using exercise as a form of airway clearance. Care must be taken in prescribing exercise to patients with hyperreactive airways or a tendency toward oxygen desaturation. Desaturation has been shown to occur with exercise in individuals with pulmonary disease,38,39 and therefore it becomes prudent to monitor oxygen saturation, providing supplemental oxygen for the exercise period when indicated. Exercise-induced bronchospasm must also be considered when pulmonary compromise is seen with exercise, especially with higher-intensity exercise.40 When medication is indicated, it is recommended to provide an inhaled bronchodilator 20 to 30 minutes before exercise to alleviate this symptom.41 Use of bronchodilator medication and supplemental oxygen may be necessary to improve exercise tolerance, but these patients require closer monitoring as well. Andreasson26 reports a risk for pneumothorax associated with exercise in patients with extensive bullae.
Contraindications and Precautions for Manual and Mechanical Airway Clearance Techniques
In patients who are very young, who have limited ability to cooperate, or who are not adherent to other ACTs, percussion, shaking, and vibration offer methods for dislodging retained secretions. However, because of the force transmitted to the thoracic cage with these techniques, there are many precautions and contraindications to consider. The therapist should not make this decision alone but should seek direction from the medical team. These treatments are not completely benign and should not be performed in the absence of good indications.42
Percussion has been shown to contribute to a fall in PaO2 in acutely ill patients,43 especially in patients with cardiovascular instability44 and in neonates.45 The factor that seems most closely associated with or predictive of this effect is the patient’s baseline PaO2.42 Cardiac dysrhythmias have been associated with chest percussion for bronchial drainage11 and Huseby46 hypothesizes that hypoxemia may be the underlying mechanism of CPT-caused cardiac arrhythmias.
Patients with hyperreactive airways (e.g., asthma) show intolerance for percussion as part of airway clearance. Campbell and colleagues47 demonstrated a fall in FEV1 associated with percussion; it was not evident when percussion was omitted. Administration of a bronchodilator before treatment with percussion precluded the fall in FEV1. Wheezing has also been associated with percussion and vibration in patients with cystic fibrosis and COPD.48,49
Box 21-1 summarizes the precautions and contraindications for external manipulation of the thorax associated with percussion, shaking, and high-frequency chest compression. Vibration involves less force to the thorax and may be better tolerated than the aforementioned techniques. A nebulized bronchodilator may be administered during a treatment of high-frequency chest compression to avoid the consequences of hyperreactive airways.
Postural Drainage
Postural drainage, also known as bronchial drainage, is a passive technique in which the patient is placed in positions that allow gravity to assist with the drainage of secretions from the bronchopulmonary tree. PD is accomplished by positioning the patient so that the angle of the lung segment to be drained allows gravity to have its greatest effect (Figure 21-2). Positioning the patient to assist the flow of bronchial secretions from the airways has been a standard treatment for some time in patients with retained secretions.50
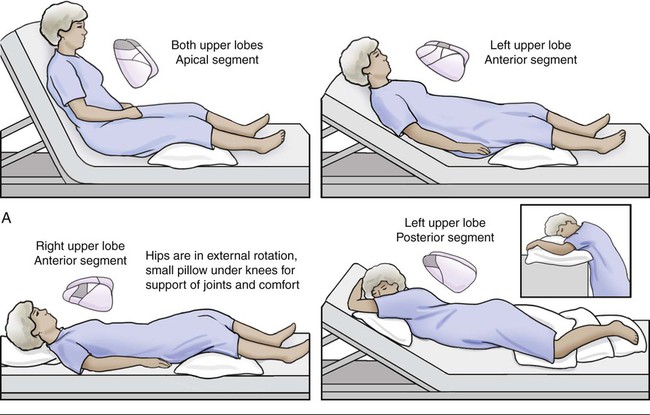
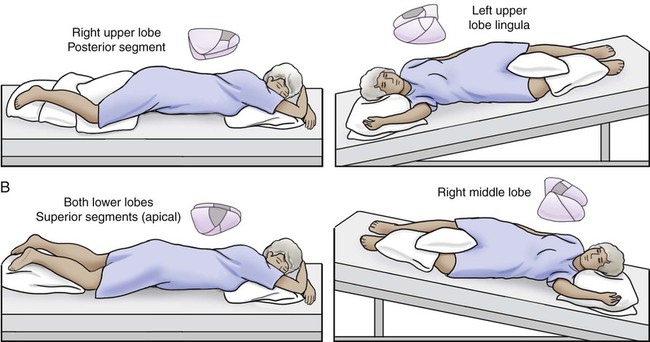
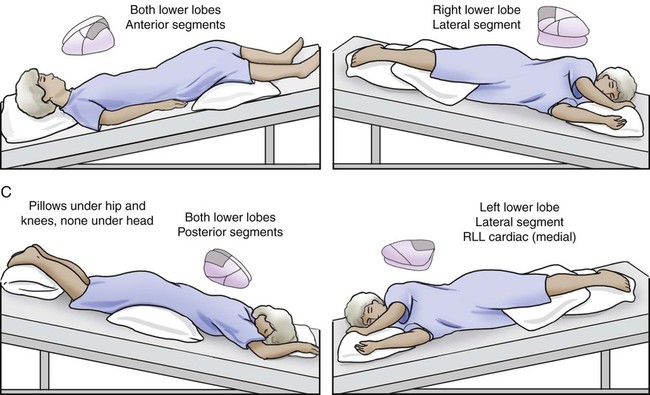
Knowledge of the anatomy of the tracheobronchial tree is vital to effective treatment. Each lobe to be drained must be aligned so that gravity can mobilize the secretions from the periphery to the larger, more central airways. The mechanism of postural drainage is considered to be a direct effect of gravity on bronchial secretions, although observations made by Lannefors (1992)32 that gravity also influences regional lung ventilation and volume suggest that these mechanisms are also involved.
PD has been shown to be effective in mobilizing secretions in patients with cystic fibrosis,51,52 bronchiectasis,10 and other pulmonary diseases.53,54 Other treatments, such as percussion, vibration, and the active cycle of breathing technique (ACBT), may be used while the patient is in postural drainage positions.
Preparation for Postural Drainage
 For the hospitalized patient, electric beds allow patients to be positioned more easily. Air therapy beds, most often used in the intensive care unit (ICU), are valuable aids for positioning, especially in patients who are large or unresponsive.
For the hospitalized patient, electric beds allow patients to be positioned more easily. Air therapy beds, most often used in the intensive care unit (ICU), are valuable aids for positioning, especially in patients who are large or unresponsive.
 In the ICU, it is imperative to be familiar with the multiple lines, tubes, and other devices attached to the patient (see Chapter 16). Allow enough slack from each device to position a patient for postural drainage.
In the ICU, it is imperative to be familiar with the multiple lines, tubes, and other devices attached to the patient (see Chapter 16). Allow enough slack from each device to position a patient for postural drainage.
 Ensure there are enough staff members to position the patient with as little stress to both patient and staff as possible.55
Ensure there are enough staff members to position the patient with as little stress to both patient and staff as possible.55
 For treatment in the clinic, have foam wedges or pillows available for positioning.
For treatment in the clinic, have foam wedges or pillows available for positioning.
 For home treatment, aids in positioning might include pillows, sofa cushions, or a bean-bag chair.
For home treatment, aids in positioning might include pillows, sofa cushions, or a bean-bag chair.
 Nebulized bronchodilators or mucolytics before PD may facilitate the mobilization of sputum.
Nebulized bronchodilators or mucolytics before PD may facilitate the mobilization of sputum.
 For the patient with an adequate cough to expectorate secretions, have tissues or a specimen cup available. Have suctioning equipment ready to remove secretions from an artificial airway or the patient’s oral or nasal cavity after the treatment. Refer to Chapter 43 for a discussion of suctioning.
For the patient with an adequate cough to expectorate secretions, have tissues or a specimen cup available. Have suctioning equipment ready to remove secretions from an artificial airway or the patient’s oral or nasal cavity after the treatment. Refer to Chapter 43 for a discussion of suctioning.
Treatment with Postural Drainage
 After determining the lobe of the lung to be treated by auscultation and chest x-ray, position the patient in the appropriate position, supporting the patient comfortably in the position indicated (see Figure 21-2).
After determining the lobe of the lung to be treated by auscultation and chest x-ray, position the patient in the appropriate position, supporting the patient comfortably in the position indicated (see Figure 21-2).
 If postural drainage is used exclusively, each position should be maintained for 5 to 10 minutes, if tolerated, or longer when focusing on a specific lobe. Coordinating the positioning with nursing care for skin pressure relief may allow the time spent in a position to be extended. If postural drainage is used in conjunction with another technique, the time in each position may be decreased. For example, if percussion and vibration are performed while the patient is in each PD position, 3 to 5 minutes is sufficient.
If postural drainage is used exclusively, each position should be maintained for 5 to 10 minutes, if tolerated, or longer when focusing on a specific lobe. Coordinating the positioning with nursing care for skin pressure relief may allow the time spent in a position to be extended. If postural drainage is used in conjunction with another technique, the time in each position may be decreased. For example, if percussion and vibration are performed while the patient is in each PD position, 3 to 5 minutes is sufficient.
 A patient who requires close monitoring should not be left unattended, but this may be appropriate if a patient is alert and able to reposition himself or herself.
A patient who requires close monitoring should not be left unattended, but this may be appropriate if a patient is alert and able to reposition himself or herself.
 It is not always necessary to treat each affected lung segment during every treatment; this may prove to be too fatiguing for the patient. The most affected lobes should be addressed with the first treatment of the day, with the other affected areas addressed during subsequent treatment(s).
It is not always necessary to treat each affected lung segment during every treatment; this may prove to be too fatiguing for the patient. The most affected lobes should be addressed with the first treatment of the day, with the other affected areas addressed during subsequent treatment(s).
 The patient should be encouraged to take deep breaths and cough after each position, if possible, and again after the treatment is completed. Having the patient sit upright or lean forward optimizes this effort by allowing the use of the abdominals for a stronger cough.55
The patient should be encouraged to take deep breaths and cough after each position, if possible, and again after the treatment is completed. Having the patient sit upright or lean forward optimizes this effort by allowing the use of the abdominals for a stronger cough.55
 Mobilization of secretions may not be apparent immediately after the treatment, but this may occur up to 1 hour later. The patient should be thus informed and reminded to clear secretions at a later time. A health care practitioner or family member should be included in this aspect of treatment, especially with patients who need encouragement.55
Mobilization of secretions may not be apparent immediately after the treatment, but this may occur up to 1 hour later. The patient should be thus informed and reminded to clear secretions at a later time. A health care practitioner or family member should be included in this aspect of treatment, especially with patients who need encouragement.55
General Precautions and Contraindications to Postural Drainage Positioning
It is essential that the therapist and the health care team discuss treatment priorities when deciding to use PD positions. A decision to use postural drainage might be made despite a contraindication if the benefits are thought to outweigh the risks in a particular case. For example, it is known that use of the Trendelenburg (head-down) position increases intracranial pressure in patients after neurosurgery.56 However, if the patient develops atelectasis, the stress of respiratory embarrassment may also increase intracranial pressure. In this instance, the decision may be made to position the patient to clear the atelectasis and subsequently return to a modified conservative regimen.55
A fall in arterial O2 saturation has been reported with the use of postural drainage for airway clearance, although the effects of PD were not separated from additional techniques.46,57 Therefore O2 saturation levels should be monitored during treatment, especially in patients with known low PaO2 values.
Caution must also be used in treating a patient with end-stage lung disease in postural drainage positions because of the risk for hemoptysis.58,59 Decreased cardiac output60,61 has been associated with chest physiotherapy treatment; however, the effects of postural drainage were not separated from those of percussion and vibration.
Many physical therapists working with the pediatric population almost never use the head-down position in treating infants but rather a modified routine that excludes the Trendelenburg position. The head-down position has been shown to increase the incidence of gastroesophageal reflux in neonates.16 Button and colleagues62 found that the head-down position is associated with gastroesophageal reflux, distressed behavior, and lower oxygen saturation in infants with cystic fibrosis. It should be noted that a finding of gastroesophageal reflux can occur even 1 hour after treatment. A modified routine that eliminates head-down positioning is associated with fewer respiratory complications.63 Box 21-2 summarizes the precautions and contraindications concerning postural drainage.
Percussion
Percussion, sometimes referred to as chest clapping, is a traditional approach to secretion mobilization. A rhythmical force is applied with a caregiver’s cupped hands against the thorax, over the involved lung segments, trapping air between the patient’s thorax and the caregiver’s hands (Figure 21-3), with the aim of dislodging or loosening bronchial secretions from the airways so they may be removed by suctioning or expectoration. This technique is performed during both the inspiratory and expiratory phases of breathing. Percussion is used in postural drainage positions for increased effectiveness64,65 and may also be used during ACBT. For individuals with pulmonary disease, percussion in conjunction with postural drainage continues to be a mainstay of the treatment, especially for pediatric patients and patients who are unresponsive.

The proposed mechanism of action of percussion is the transmission of a wave of energy through the chest wall into the lung. This wave loosens secretions from the bronchial wall and moves them proximally, where ciliary motion and cough (or suction) can remove them. The combination of postural drainage and percussion has been shown to be effective in secretion removal.66–68
A handheld mechanical percussor can be used by a caregiver to minimize fatigue or may be used by the patient to self-administer percussion. The effectiveness of mechanical as opposed to manual percussion has been studied. Maxwell and Redmond69 found mechanical percussion equivalent to manual percussion in effecting removal of secretions. Although there was a significant increase in pulmonary function with manual techniques, Pryor and colleagues70,71 supported the use of mechanical percussion in patients, using the forced expiration technique. A study by Rossman and colleagues72 was in disagreement, finding that mechanical percussion did not enhance postural drainage in secretion removal.
Preparation for Percussion
 The only equipment required for manual percussion is the caregiver’s cupped hands to deliver the force to mobilize secretions.
The only equipment required for manual percussion is the caregiver’s cupped hands to deliver the force to mobilize secretions.
 For the adult and older pediatric population, electric or pneumatic percussors that mechanically simulate percussion are available. This enables a patient to apply self-percussion more effectively. Several models have variable frequencies of percussion, as well as different levels of intensity.
For the adult and older pediatric population, electric or pneumatic percussors that mechanically simulate percussion are available. This enables a patient to apply self-percussion more effectively. Several models have variable frequencies of percussion, as well as different levels of intensity.
 Several devices, including padded rubber nipples, pediatric anesthesia masks, padded medicine cups, or the bell end of a stethoscope may be used to provide percussion to infants whose chest walls are too small to accommodate the size of an adult’s hand.
Several devices, including padded rubber nipples, pediatric anesthesia masks, padded medicine cups, or the bell end of a stethoscope may be used to provide percussion to infants whose chest walls are too small to accommodate the size of an adult’s hand.
 Placing the patient in appropriate PD positions (as the patient’s condition allows) enhances the effect of percussion.
Placing the patient in appropriate PD positions (as the patient’s condition allows) enhances the effect of percussion.
 A thin towel or hospital gown should cover the patient’s skin where the percussion is to be applied. The force of percussion over bare skin may be uncomfortable; however, padding that is too thick absorbs the force of the percussion without benefit to the patient.
A thin towel or hospital gown should cover the patient’s skin where the percussion is to be applied. The force of percussion over bare skin may be uncomfortable; however, padding that is too thick absorbs the force of the percussion without benefit to the patient.
 Adjust the level of the bed so that the caregiver may use proper body mechanics during the treatment. The caregiver may become excessively fatigued or injured as a result of lengthy or numerous treatments if proper body mechanics are ignored.
Adjust the level of the bed so that the caregiver may use proper body mechanics during the treatment. The caregiver may become excessively fatigued or injured as a result of lengthy or numerous treatments if proper body mechanics are ignored.
Treatment with Percussion
 Position the hand in the shape of a cup with the fingers and thumb adducted. It is important to maintain this cupped position with the hands throughout the treatment, while letting the wrists, arms, and shoulders stay relaxed.
Position the hand in the shape of a cup with the fingers and thumb adducted. It is important to maintain this cupped position with the hands throughout the treatment, while letting the wrists, arms, and shoulders stay relaxed.
 The sound of percussion should be hollow as opposed to a slapping sound. If erythema occurs with percussion, it is usually a result of slapping or not trapping enough air between the hand and the chest wall.73
The sound of percussion should be hollow as opposed to a slapping sound. If erythema occurs with percussion, it is usually a result of slapping or not trapping enough air between the hand and the chest wall.73
 The patient will better tolerate an even, steady rhythm. The rate of manual percussion delivered by caregivers can vary between 100 and 480 times per minute.73
The patient will better tolerate an even, steady rhythm. The rate of manual percussion delivered by caregivers can vary between 100 and 480 times per minute.73
 The force applied to the chest wall from each hand should be equal. If the nondominant hand is not able to keep up with the dominant hand, the rate should be slowed to match that of the slower hand. It might be helpful to start with the nondominant hand and let the dominant hand match the nondominant hand.55 The force does not have to be excessive to be effective; the amount of force should be adapted to the patient’s comfort.
The force applied to the chest wall from each hand should be equal. If the nondominant hand is not able to keep up with the dominant hand, the rate should be slowed to match that of the slower hand. It might be helpful to start with the nondominant hand and let the dominant hand match the nondominant hand.55 The force does not have to be excessive to be effective; the amount of force should be adapted to the patient’s comfort.
 If the size of an infant does not allow use of a full hand, percussion may be done manually with four fingers cupped, three fingers with the middle finger “tented,” or the thenar and hypothenar surfaces of the hand.74
If the size of an infant does not allow use of a full hand, percussion may be done manually with four fingers cupped, three fingers with the middle finger “tented,” or the thenar and hypothenar surfaces of the hand.74
 Hand position should be such that percussion does not occur over bony prominences of the patient. The spinous processes of the vertebrae, the spine of the scapula, and the clavicle should all be avoided. Percussion over the floating ribs should also be avoided because these ribs have only a single attachment.
Hand position should be such that percussion does not occur over bony prominences of the patient. The spinous processes of the vertebrae, the spine of the scapula, and the clavicle should all be avoided. Percussion over the floating ribs should also be avoided because these ribs have only a single attachment.
 Percussion should not be performed over breast tissue. This will produce discomfort and diminish the effectiveness of the treatment. In the case of very large breasts, it may be necessary to move the breast out of the way with one hand (or ask the patient to do this) and percuss with the other hand.
Percussion should not be performed over breast tissue. This will produce discomfort and diminish the effectiveness of the treatment. In the case of very large breasts, it may be necessary to move the breast out of the way with one hand (or ask the patient to do this) and percuss with the other hand.
 A patient may be taught to perform one-handed self-percussion to those areas that can be reached comfortably, either manually or with a mechanical percussor. This does, however, virtually preclude the treatment of the posterior lung segments.
A patient may be taught to perform one-handed self-percussion to those areas that can be reached comfortably, either manually or with a mechanical percussor. This does, however, virtually preclude the treatment of the posterior lung segments.
Advantages and Disadvantages of Percussion
Percussion is not well tolerated by many patients postoperatively without adequate pain control. The force of percussion may also be contraindicated in patients with osteoporosis or coagulopathy. Percussion has been associated with a fall in oxygen saturation, which can be eliminated with concurrent thoracic expansion exercises and pauses for breathing control.75
Vibration and Shaking
It is proposed that vibration and shaking enhance mucociliary transport from the periphery of the lung fields to the larger, central airways. Because the compressive force to the thorax is greater with shaking than vibration, it produces increased chest wall displacement, and the stretch of the respiratory muscles may produce an increased inspiratory effort and lung volume.76 The same relative contraindications for percussion should be observed for shaking, because it involves the application of force to the thorax.
Pavia77 demonstrated a higher, though not statistically significant, rate of secretion clearance and sputum production with vibration. However, this study was conducted while subjects were in the upright position only, which does not replicate the use of vibration clinically. Many studies do not separate the effects of vibration from the components of PD and percussion because they are often used in conjunction. In fact, many studies describe the techniques of PD, percussion, and vibration or shaking as a single entity and refer to the treatment as chest physical therapy or postural drainage therapy. Mackenzie and colleagues78 demonstrated significant improvement in total lung/thorax compliance after treatment with postural drainage, percussion, and vibration in mechanically ventilated patients. Feldman and colleagues48 demonstrated improved ventilatory function by improved expiratory flow rates in patients receiving postural drainage, percussion, vibration, and directed coughing.
Preparation for Vibration and Shaking
 For manual techniques, the caregiver’s hands are the only “equipment” required.
For manual techniques, the caregiver’s hands are the only “equipment” required.
 Mechanical vibrators are available to administer the treatment and are useful for self-treatment by a patient or to reduce fatigue in the caregiver.
Mechanical vibrators are available to administer the treatment and are useful for self-treatment by a patient or to reduce fatigue in the caregiver.
 For infants, a padded electric toothbrush may be used.74
For infants, a padded electric toothbrush may be used.74
 Place the patient in the appropriate PD position or modified position, as the patient’s status allows.
Place the patient in the appropriate PD position or modified position, as the patient’s status allows.
 Place a thin towel or hospital gown over the patient’s skin. The material should not be thick enough to absorb the effect of the vibration or shaking.
Place a thin towel or hospital gown over the patient’s skin. The material should not be thick enough to absorb the effect of the vibration or shaking.
 Proper body position of the caregiver is important to deliver an effective treatment and to decrease caregiver fatigue.
Proper body position of the caregiver is important to deliver an effective treatment and to decrease caregiver fatigue.
Treatment with Vibration and Shaking
 For vibration, the hands may be placed side by side or on top of each other, as shown in Figure 21-4. As with shaking, the patient is instructed to take in a deep breath while in a proper PD position. A gentle but steady co-contraction of the upper extremities is performed to vibrate the chest wall, beginning at the peak of inspiration and following the movement of chest deflation. The frequency of manual vibration is between 12 and 20 Hz.44,53
For vibration, the hands may be placed side by side or on top of each other, as shown in Figure 21-4. As with shaking, the patient is instructed to take in a deep breath while in a proper PD position. A gentle but steady co-contraction of the upper extremities is performed to vibrate the chest wall, beginning at the peak of inspiration and following the movement of chest deflation. The frequency of manual vibration is between 12 and 20 Hz.44,53
 For shaking, with the patient in the appropriate PD position, place your hands over the lobe of the lung to be treated and instruct the patient to take in a deep breath. At the peak of inspiration, apply a slow (approximately 2 times per second), rhythmic bouncing pressure to the chest wall until the end of expiration. The hands follow the movement of the chest as the air is exhaled. The frequency of shaking is 2 Hz.44,53
For shaking, with the patient in the appropriate PD position, place your hands over the lobe of the lung to be treated and instruct the patient to take in a deep breath. At the peak of inspiration, apply a slow (approximately 2 times per second), rhythmic bouncing pressure to the chest wall until the end of expiration. The hands follow the movement of the chest as the air is exhaled. The frequency of shaking is 2 Hz.44,53
 If the patient is mechanically ventilated, the previously described techniques needs to be coordinated with ventilator-controlled exhalation.
If the patient is mechanically ventilated, the previously described techniques needs to be coordinated with ventilator-controlled exhalation.
 If the patient has a rapid respiratory rate, either voluntary or ventilator-controlled, it may be necessary to apply vibration or shaking only during every other exhalation.
If the patient has a rapid respiratory rate, either voluntary or ventilator-controlled, it may be necessary to apply vibration or shaking only during every other exhalation.
 A mobile chest wall is necessary to apply a compressive force without causing discomfort. If a patient has limited chest wall compliance, vibration will probably be better tolerated than shaking.
A mobile chest wall is necessary to apply a compressive force without causing discomfort. If a patient has limited chest wall compliance, vibration will probably be better tolerated than shaking.
 Mechanical vibrators may be used by the unattended patient, although only limited attention can be paid to the posterior portions of the lungs.
Mechanical vibrators may be used by the unattended patient, although only limited attention can be paid to the posterior portions of the lungs.
Manual Hyperinflation
The technique of manual hyperinflation was used more commonly in the past for patients requiring mechanical ventilation. However there is not enough evidence to promote the regular use of this technique that has many contraindications and that is not well known in the United States.80 A brief description of the technique and its precautions follows. Two caregivers are needed to perform the technique with the patient placed in PD positions.79 One caregiver uses a manual inflation bag to hyperinflate the lungs with a slow, deep inspiration and, after a short pause, provides a quick release to allow rapid exhalation. A second caregiver applies shaking or vibration at the beginning of exhalation to mobilize secretions. The technique is promoted to mobilize secretions and reinflate collapsed areas of the lung and is likened to simulating a cough—deep inspiration, pause, and forceful exhalation.
Clement80 reported that this method of airway clearance enabled patients to be maintained on ventilators for long periods while retaining normal lung function. It was also demonstrated that the addition of positioning and vibrations enhanced the treatment of atelectasis by hyperinflation and suctioning.81
The risks to using manual hyperinflation are numerous. There are several adverse hemodynamic effects of this technique and hyperinflation has the potential to cause barotraumas.61,80,83
Active Cycle of Breathing Technique
In New Zealand, Thompson85 described clearing bronchial secretions in patients with asthma by using a technique of forced expirations and diaphragmatic breathing. British physiotherapists modified the technique and further described it in the literature, first as the forced expiration technique (FET)70 and later as the active cycle of breathing technique.86
As described by Webber and Pryor,86 ACBT consists of repeated cycles of three ventilatory phases: breathing control, thoracic expansion exercises, and FET. Breathing control is described as gentle tidal volume breathing with relaxation of the upper chest and shoulders. The thoracic expansion phase consists of deep inspiration and may be accompanied by percussion or vibration performed by a caregiver or the patient. This phase helps to loosen secretions. The forced expiration technique involves one or two huffs, as when fogging a window or cleaning glasses with one’s breath. Slow huffing from a middle lung volume (a medium-sized inspiration) down to a low lung volume moves secretions from the peripheral to the upper airways, whereas upper airway secretions may be cleared by a quicker huff from a high lung volume or deeper inspiration.86
The period of breathing control between the other phases is essential in order to prevent bronchospasm.87 The period of thoracic expansion, which increases lung volume and promotes collateral ventilation, allows air to get behind secretions and assist in their mobilization.88 Mead and colleagues89 described the physiological theory of the equal pressure point (EPP), which is the basis for FET. EPP is the point in the airways where the pressure is equal to the pleural pressure. The forced expiratory maneuver produces compression of the airway peripherally to EPP. A huff from high lung volume causes compression within the trachea and bronchi, which moves secretions from these larger airways. A huff continued to low lung volume shifts the EPP more peripherally, which mobilizes more peripheral secretions.84
Because huffing has been shown to stabilize collapsible bronchial walls, it increases the expiratory flow in patients with obstruction without causing airway collapse.90 Another benefit of this technique is its ability to maintain oxygen saturation. The decrease in oxygen saturation that has been demonstrated with postural drainage and percussion has been prevented by the use of ACBT.75 Hassani and colleagues (1994)91 showed that unproductive cough and FET resulted in the movement of secretions proximally from all regions of the lung in patients with mild hyposecretion. Therefore, FET may help to avoid prolonged retention of secretions, even in patients who produce little sputum.
ACBT may be performed in the sitting position but has been shown to be more effective in gravity-assisted positions; although horizontal side lying may have fewer adverse effects than the head-down position.50,92 This method encourages active participation of the patient and has been shown to be as effective when performed by the patient alone or with the aid of a caregiver.70 FET performed by patients independently has been shown to clear more sputum in a shorter amount of time than PD with self-percussion combined with percussion and shaking by a physical therapist.70 Improvements in pulmonary function93 and sputum clearance94 have been demonstrated in patients with cystic fibrosis who incorporated FET into their postural drainage treatments. ACBT has been shown to be equally effective as positive expiratory pressure (PEP) in a year-long study.50 Additionally, this method of airway clearance may be used with some children as young as 3 or 4 years of age. The sequence of ACBT is shown in Box 21-3.
Preparation for Active Cycle of Breathing Technique
 The only equipment required for this manual technique is the patient’s or caregiver’s hands to percuss or shake/vibrate the chest wall during the thoracic expansion phase.
The only equipment required for this manual technique is the patient’s or caregiver’s hands to percuss or shake/vibrate the chest wall during the thoracic expansion phase.
 Mechanical percussors or vibrators may be used during the thoracic expansion phase, either for self-percussion by the patient or for use by the caregiver.
Mechanical percussors or vibrators may be used during the thoracic expansion phase, either for self-percussion by the patient or for use by the caregiver.
 To teach the huffing maneuver (part of FET), it may be helpful to use a peak flow meter mouthpiece to maintain the mouth and glottis open (Figure 21-5). Young children may be taught games of huffing at cotton balls or tissue to improve the effect of the technique.86 To help them focus on the expiratory maneuver, small children may also be taught to flap their arms to their lateral chest as they perform the huff, a technique referred to as the “chicken breath.”95
To teach the huffing maneuver (part of FET), it may be helpful to use a peak flow meter mouthpiece to maintain the mouth and glottis open (Figure 21-5). Young children may be taught games of huffing at cotton balls or tissue to improve the effect of the technique.86 To help them focus on the expiratory maneuver, small children may also be taught to flap their arms to their lateral chest as they perform the huff, a technique referred to as the “chicken breath.”95
 The patient should be in a PD position to stimulate drainage of a productive area of the lungs, although the entire treatment may also be performed in the upright sitting position. If PD positions are used, equipment for positioning will be required.
The patient should be in a PD position to stimulate drainage of a productive area of the lungs, although the entire treatment may also be performed in the upright sitting position. If PD positions are used, equipment for positioning will be required.
 Most patients tolerate treatment of two or three productive areas during one session.
Most patients tolerate treatment of two or three productive areas during one session.
 A minimum of 10 minutes in any productive position may be necessary to clear a patient with a moderate amount of secretions. Patients after surgery or with minimal secretions may not require as much time, and very ill patients may fatigue before optimal treatment is given.86
A minimum of 10 minutes in any productive position may be necessary to clear a patient with a moderate amount of secretions. Patients after surgery or with minimal secretions may not require as much time, and very ill patients may fatigue before optimal treatment is given.86
Treatment with Active Cycle of Breathing Technique
 During the breathing control phase, the patient is instructed to breathe in a relaxed manner using normal tidal volume. The upper chest and shoulders should remain relaxed, and the lower chest and abdomen should be active. The breathing control phase should last as long as is required for the patient to relax and prepare for the next phases, usually 5 to 10 seconds.
During the breathing control phase, the patient is instructed to breathe in a relaxed manner using normal tidal volume. The upper chest and shoulders should remain relaxed, and the lower chest and abdomen should be active. The breathing control phase should last as long as is required for the patient to relax and prepare for the next phases, usually 5 to 10 seconds.
 The emphasis during the thoracic expansion phase is on inspiration. The patient is instructed to take in a deep breath to the inspiratory reserve volume; expiration is passive and relaxed. The caregiver or the patient may place a hand over the area of the thorax being treated to facilitate increased chest wall movement.
The emphasis during the thoracic expansion phase is on inspiration. The patient is instructed to take in a deep breath to the inspiratory reserve volume; expiration is passive and relaxed. The caregiver or the patient may place a hand over the area of the thorax being treated to facilitate increased chest wall movement.
 Chest percussion, shaking, or vibration may be performed in combination with thoracic expansion as the patient exhales. For surgical patients or those with lung collapse, a breath hold or a sniff at the end of inspiration encourages collateral ventilation to redistribute air into collapsed segments and assist with reexpansion of the lung.
Chest percussion, shaking, or vibration may be performed in combination with thoracic expansion as the patient exhales. For surgical patients or those with lung collapse, a breath hold or a sniff at the end of inspiration encourages collateral ventilation to redistribute air into collapsed segments and assist with reexpansion of the lung.
 The FET phase consists of huffing interspersed with breathing control. A huff is a rapid, forced exhalation without maximal effort. This maneuver is comparable to fogging a pair of eyeglasses with warm breath so they may be cleaned. Unlike a cough, in which the glottis is closed, a huff requires the glottis to remain open. In an effective huff, the muscles of the abdomen should contract to provide greater expiratory force. Other characteristics of effective versus ineffective huffing are shown in Box 21-4.
The FET phase consists of huffing interspersed with breathing control. A huff is a rapid, forced exhalation without maximal effort. This maneuver is comparable to fogging a pair of eyeglasses with warm breath so they may be cleaned. Unlike a cough, in which the glottis is closed, a huff requires the glottis to remain open. In an effective huff, the muscles of the abdomen should contract to provide greater expiratory force. Other characteristics of effective versus ineffective huffing are shown in Box 21-4.
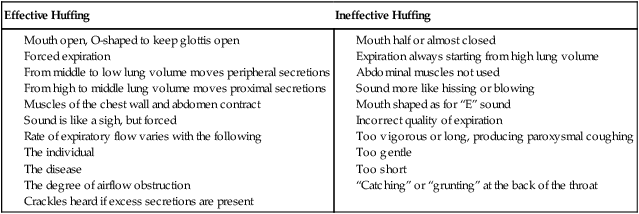
From Partridge C, Pryor J, Webber B: Characteristics of the forced expiration technique, Physiotherapy 75:193-194, 1989.
 Two different levels of huffing are characterized in FET. To mobilize secretions from peripheral airways, a huff after a medium-sized inspiration will be effective. This huff will be longer and quieter. To clear secretions that have reached the larger, proximal airways, a huff after a deep inspiration will be effective. This huff will be shorter and louder.
Two different levels of huffing are characterized in FET. To mobilize secretions from peripheral airways, a huff after a medium-sized inspiration will be effective. This huff will be longer and quieter. To clear secretions that have reached the larger, proximal airways, a huff after a deep inspiration will be effective. This huff will be shorter and louder.
 The patient must pause for breathing control after one or two huffs. This will prevent any increase in airflow obstruction.
The patient must pause for breathing control after one or two huffs. This will prevent any increase in airflow obstruction.
 ACBT should be adapted to the individual patient’s needs. If secretions are tenacious, two cycles of the thoracic expansion phase may be necessary to loosen secretions before FET can follow. In a patient with bronchospasm or unstable airways, the breathing control phase may be as long as 10 to 20 seconds.86 After surgery, the patient may be shown how to support the incision with her hands during FET to achieve sufficient expiratory force.
ACBT should be adapted to the individual patient’s needs. If secretions are tenacious, two cycles of the thoracic expansion phase may be necessary to loosen secretions before FET can follow. In a patient with bronchospasm or unstable airways, the breathing control phase may be as long as 10 to 20 seconds.86 After surgery, the patient may be shown how to support the incision with her hands during FET to achieve sufficient expiratory force.
 When a huff from a medium-sized inspiration through complete expiration is nonproductive and dry sounding for two cycles in a row, the treatment may be concluded.96
When a huff from a medium-sized inspiration through complete expiration is nonproductive and dry sounding for two cycles in a row, the treatment may be concluded.96
Advantages and Disadvantages of Active Cycle of Breathing
The technique may be adapted for patients with gastroesophageal reflux, bronchospasm, and an acute exacerbation of their pulmonary disease. A decrease in oxygen saturation caused by chest percussion may be avoided by using ACBT.75 When the technique is performed independently, the cost of using ACBT for the long term is minimal.
Autogenic Drainage
In Belgium in 1976, Chevaillier introduced autogenic drainage (AD), or self-drainage, for the treatment of asthmatic patients. He observed that during sleep, as well as while playing and laughing during the day, mucus was mobilized better than it was during PD and clapping. AD is an “antidyspnea” technique based on quiet expirations in a relaxed state and without use of postural drainage positions.97
Schoni98 eloquently explained the physiology of AD’s three phases, which use diaphragmatic breathing to mobilize secretions by varying expiratory airflow (Figure 21-6). The first phase starts with a normal inspiration and is followed by a breath hold to ensure equal filling of lung segments by collateral filling; then a deep exhalation is made into the expiratory reserve volume range. By lowering the middle tidal volume below the functional residual capacity level, secretions from peripheral lung regions are mobilized by the compression of peripheral alveolar ducts. Mid-expiratory tidal volume is lowered in the range of normal expiratory reserve volume. Chevaillier97 named this phase the “unsticking” phase. The second phase of AD consists of tidal volume breathing gradually changing from the expiratory reserve volume into the inspiratory reserve volume range, which mobilizes secretions from the apical parts of the lungs. The velocity of the airflow must be adjusted at each level of inspiration so that the maximal expiratory airflow is reached without being high enough to cause collapse of the airways. Flow volume curves show that higher flows of longer duration can be achieved with AD,99 demonstrating that mucus can be moved farther and at a faster rate. This is the “collecting” phase97 The third phase consists of deeper inspiration into the inspiratory reserve volume, with huffing often used to help in evacuating the mobilized secretions. Control of airflow during this final phase is essential to the avoidance of uncontrolled, unproductive coughing. Chevaillier97 named this phase the “evacuating” phase.
The Belgian method of AD has been modified by German practitioners using a combination of diaphragmatic and costosternal breathing in a treatment that is not separated into phases.100 This modification resulted from the observation that many patients had difficulty breathing in the expiratory reserve volume range. The patient varies his or her mid-tidal volume in a passive exhalation followed by an active exhalation through pursed lips or through the nose. The German method of airway clearance includes other maneuvers in conjunction with AD, including inhalation therapy, FET, chest wall exercises, and physical activity.
Assisted AD has been described for use in treating infants and patients who are unable to participate.50 Gentle manual pressure is applied to the chest during inspiration in an effort to vary the volume of breath inhaled; no pressure is applied during exhalation. This technique is often applied while gently bouncing the infant on a therapy ball.
AD has been compared with positive expiratory pressure and PD with percussion and/or vibration. It was reported that more sputum was produced with AD in patients with hyperreactive airways.101 In a 2-year crossover trial, AD was found to be as effective as conventional CPT among patients with cystic fibrosis for improving pulmonary function.102 However, patients exhibited a strong preference for AD over CPT, increasing the likelihood of adherence. Miller103 showed greater clearance of inhaled radioisotopes with AD than with ACBT, with no significant differences in sputum weight, spirometry, or transcutaneous oxygen saturation. Giles104 also studied oxygen saturation in AD and found greater levels with AD than with PD with percussion; there was also greater sputum evacuated with AD.
Preparation for Autogenic Drainage
 No equipment is needed for a patient to perform the technique of AD. The patient must possess good proprioceptive, tactile, and auditory perception of the mucus moving—this feedback makes it possible to adjust the technique of AD.
No equipment is needed for a patient to perform the technique of AD. The patient must possess good proprioceptive, tactile, and auditory perception of the mucus moving—this feedback makes it possible to adjust the technique of AD.
 To teach this method to a patient, a caregiver needs keen tactile and auditory senses to coach a patient to move between the phases by listening to and palpating the chest to identify the location and the quality of the secretions.
To teach this method to a patient, a caregiver needs keen tactile and auditory senses to coach a patient to move between the phases by listening to and palpating the chest to identify the location and the quality of the secretions.
 The patient should be seated upright in a chair with a back for support. The surroundings should be devoid of distractions, allowing the patient to concentrate on the breathing technique.
The patient should be seated upright in a chair with a back for support. The surroundings should be devoid of distractions, allowing the patient to concentrate on the breathing technique.
 The upper airways (nose and throat) should be cleared of secretions by huffing or blowing the nose.
The upper airways (nose and throat) should be cleared of secretions by huffing or blowing the nose.
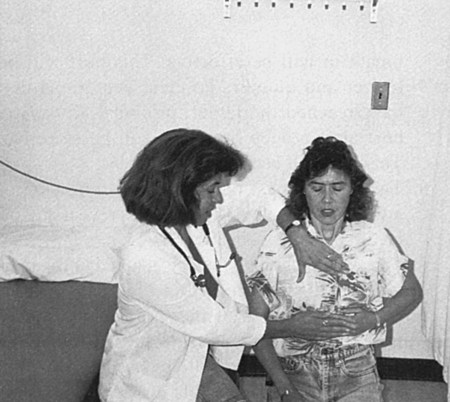
 The caregiver should be seated to the side and slightly behind the patient, close enough to hear the patient’s breathing. One hand should be placed to feel the work of the abdominal muscles and the other hand placed on the upper chest (Figure 21-7).
The caregiver should be seated to the side and slightly behind the patient, close enough to hear the patient’s breathing. One hand should be placed to feel the work of the abdominal muscles and the other hand placed on the upper chest (Figure 21-7).
Treatment with Autogenic Drainage
 In all phases, inhalation should be done slowly, through the nose if possible, using the diaphragm or lower chest. A 2- to 3-second breath hold should follow, allowing collateral ventilation to get air behind the secretions.
In all phases, inhalation should be done slowly, through the nose if possible, using the diaphragm or lower chest. A 2- to 3-second breath hold should follow, allowing collateral ventilation to get air behind the secretions.
 Exhalation should occur actively with the mouth and glottis open, listening for the movement of mucus while avoiding a wheeze. The vibrations of the mucus may also be felt with the hand placed on the upper chest. The frequency of these vibrations reveals their location. High frequencies mean that the secretions are located in the small airways; low frequencies mean that the secretions have moved to the large airways.97
Exhalation should occur actively with the mouth and glottis open, listening for the movement of mucus while avoiding a wheeze. The vibrations of the mucus may also be felt with the hand placed on the upper chest. The frequency of these vibrations reveals their location. High frequencies mean that the secretions are located in the small airways; low frequencies mean that the secretions have moved to the large airways.97
 In practice, inspiration is followed by a deep expiration into the expiratory reserve volume. The patient attempts to exhale as far into the expiratory reserve volume as possible, contracting the abdominal muscles to achieve this. This low lung volume breathing continues until the mucus is loosened and starts to move into the larger airways.
In practice, inspiration is followed by a deep expiration into the expiratory reserve volume. The patient attempts to exhale as far into the expiratory reserve volume as possible, contracting the abdominal muscles to achieve this. This low lung volume breathing continues until the mucus is loosened and starts to move into the larger airways.
 The second phase collects the mucus in the middle airways by increasing the lung volume to a greater level than in the initial phase. Tidal volume breathing is then changed gradually from expiratory reserve volume toward the inspiratory reserve volume range98 so that the lungs are expanded more with each inspiration. The patient increases both inspiration and expiration to move a greater volume of air. This low to middle lung volume breathing continues until the sound of the mucus decreases, signaling its movement into the central airways to be evacuated.
The second phase collects the mucus in the middle airways by increasing the lung volume to a greater level than in the initial phase. Tidal volume breathing is then changed gradually from expiratory reserve volume toward the inspiratory reserve volume range98 so that the lungs are expanded more with each inspiration. The patient increases both inspiration and expiration to move a greater volume of air. This low to middle lung volume breathing continues until the sound of the mucus decreases, signaling its movement into the central airways to be evacuated.
 In the evacuation phase, the patient increases inspiration into the inspiratory reserve volume range. This middle-to-high lung volume breathing continues until the secretions are in the trachea and are ready to be expectorated. The collected mucus can be evacuated by a stronger expiration or a high-volume huff. Nonproductive coughing should be avoided, since it may result in collapse of airways. See Figure 21-6 for a diagram of the three phases of AD.
In the evacuation phase, the patient increases inspiration into the inspiratory reserve volume range. This middle-to-high lung volume breathing continues until the secretions are in the trachea and are ready to be expectorated. The collected mucus can be evacuated by a stronger expiration or a high-volume huff. Nonproductive coughing should be avoided, since it may result in collapse of airways. See Figure 21-6 for a diagram of the three phases of AD.
 Compression of the airways should be avoided. If wheezing is heard, the expiratory flow rate must be decreased. Beginners may have to use pursed lips to avoid airway compression.97 Instructing the patient to roll the tongue (if possible) may assist in controlling the expiratory flow rate.
Compression of the airways should be avoided. If wheezing is heard, the expiratory flow rate must be decreased. Beginners may have to use pursed lips to avoid airway compression.97 Instructing the patient to roll the tongue (if possible) may assist in controlling the expiratory flow rate.
 In the simplified German procedure, the patient begins by varying the mid-tidal volume without excessive effort. After a passive but rapid expiration, an actively performed expiration follows, achieving exhalation to a low expiratory reserve volume (Figure 21-8).
In the simplified German procedure, the patient begins by varying the mid-tidal volume without excessive effort. After a passive but rapid expiration, an actively performed expiration follows, achieving exhalation to a low expiratory reserve volume (Figure 21-8).
 The duration of each phase of AD depends on the location of the secretions. The duration of a session depends on the amount and viscosity of the secretions. An average treatment will be 30 to 45 minutes in length. However, a patient who is experienced in performing AD will clear secretions in a shorter amount of time than a beginner.
The duration of each phase of AD depends on the location of the secretions. The duration of a session depends on the amount and viscosity of the secretions. An average treatment will be 30 to 45 minutes in length. However, a patient who is experienced in performing AD will clear secretions in a shorter amount of time than a beginner.
Advantages and Disadvantages of Autogenic Drainage
When learned effectively, AD may be performed independently by patients over 12 years of age and requires no additional equipment. It is ideal for the adolescent or adult who prefers an independent method. Because it does not require the use of PD positions, it is appropriate for patients with gastroesophageal reflux. It is also recommended for use in patients with airway hyperreactivity.105 The technique of AD requires attention to airflow and volume and to cough suppression until secretions are mobilized; this is a key factor to success.106 Learning AD requires tactile and auditory feedback and continued modifications of the patient’s technique, at least initially, to achieve a good result.
Although widely used in Europe, the use of AD in the United States is limited by the lack of trained caregivers but is growing in popularity. To learn this technique, patients must demonstrate good self-discipline and concentration. This method takes more practice than others. AD is not the treatment of choice for a patient who is unmotivated or uncooperative, and a study of flow volume curves suggests that AD would not be appropriate for small children even if they were cooperative.99 A patient must also be available for periodic reevaluation and refinement of the technique. During early hospitalization for patients admitted with an acute exacerbation is a challenging time in terms of learning AD. Patients who are skilled in the technique may choose a more passive form (one consuming less energy) of airway clearance at such times until they return to their baseline pulmonary status.
Positive Expiratory Pressure
Positive expiratory pressure includes a one-way breathing valve and an adjustable level of expiratory resistance that creates a back pressure to stent the airways open during exhalation. It is theorized that PEP breathing reinflates collapsed alveoli by allowing air to be redistributed through collateral channels—the pores of Kohn and the Lambert canals—allowing pressure to build up distal to the obstruction and promoting the movement of secretions toward the larger airways.107,108 In addition, supplemental oxygen and nebulized medication can be effectively delivered during treatment with PEP.109 A manometer in the circuit determines and monitors the pressure generated by the patient. In low-pressure PEP breathing, the resistance is regulated to achieve 10 to 20 cm of H2O during slightly active expiration. The appropriate resistor is one that produces a flow volume curve demonstrating a maximal forced vital capacity, good plateau, and no curvilinearity.88 Low-pressure PEP breathing is used more often than high-pressure PEP, as it offers equal effectiveness at a lower presumed risk for pneumothorax.
Airway stability is maintained with PEP breathing, which results in improved ventilation and gas exchange as well as airway clearance.110 PEP breathing has been shown to benefit patients at risk for postoperative atelectasis but has gained wider practice in the area of airway clearance, especially in patients with cystic fibrosis.95 Numerous studies have demonstrated the effectiveness of PEP breathing. Tyrrell111 has shown the PEP mask to be as effective as conventional physiotherapy over a 1-month period, with no difference in pulmonary function. Falk112,113 demonstrated increased sputum production and clearance with the use of PEP over FET alone. However, Hofmeyer114 found FET produced a greater quantity of sputum without the addition of PEP. Oberwaldner115 evaluated lung function during 10 months of regular treatments with high-pressure PEP and found reduced pulmonary hyperinflation and airway instability and higher flow rates with PEP than with conventional CPT. These improvements in lung function deteriorated only 2 months after a return to conventional CPT. A study by Pfleger and colleagues105 compared PEP with AD and found that PEP cleared higher amounts of sputum and demonstrated increased lung function. Finally, decreased duration of hospitalization has been cited as a benefit of using PEP breathing for airway clearance.116
Two of the most commonly used devices in the United States are the Acapella (Figure 21-9, A and B) and TheraPEP (DHD Healthcare, Wampsville, New York) (Figure 21-9, C). The TheraPEP device consists of a mouthpiece and an expiratory resistor that can accommodate many levels of expiratory flow. It comes with a detachable pressure monitoring port and indicator to show 10 to 20 cm of H2O. The TheraPEP can accommodate a mask of different sizes. The Acapella has performance characteristics similar to those of the Flutter.117 It comes in several models: green for patients who can maintain an expiratory flow of 15 L/min or more, blue for patients whose expiratory flow rate is less than 15 L/min, and the Acapella Choice. The Acapella Choice disassembles more easily than the original models for ease of cleaning (Figure 21-9, D). The Acapella consists of a mouthpiece attached to the body of the unit that uses a counterweighted plug and magnet to create airflow oscillation and a dial for expiratory resistance at the other end.
A device developed in Switzerland to deliver high-frequency oscillation PEP breathing and decrease the collapsibility of the airways is the Flutter VRP1 (VarioRaw, Aubonne, Switzerland). Axcan Pharma (Birmingham, Alabama) markets the Flutter VRP1 valve in the United States, the first oscillatory PEP device available in this country. This pipelike device consists of a steel ball, a plastic cone, a perforated cover, and a mouthpiece. Exhaled air causes the steel ball to roll up and down the cone causing airflow vibration. The PEP maintained by the Flutter (5 to 35 cm of H2O) prevents dynamic airway compression and improves airflow acceleration.118 The full effects of the vibration induced by the Flutter (6 to 20 Hz) may be received by changing the angle of the device. Movement of the Flutter upward increases the pressure and frequency while movement of the device downward results in lower pressure and frequency.118 The vibration of the chest can be palpated to provide feedback as to the optimal angle of the device. The recommended procedure for use of the Flutter is shown in Box 21-5.
This early form of oscillatory PEP has been well studied. Konstan and colleagues119 compared the amount of sputum expectorated with the Flutter with that expectorated with vigorous voluntary cough, with PD, with percussion, and with vibration. Subjects with cystic fibrosis produced more than three times the amount of sputum when using the Flutter than when using the other two methods, and no adverse effects were reported. The improvement in expectoration is based on the increase in airway diameter and the improvement in airflow acceleration.120 Ambrosino121 reported success in the treatment of patients with chronic obstructive pulmonary disease by using the device. When compared with AD, the Flutter was found to produce equal amounts of expectorated mucus.122 The advantages of the Flutter device lie in its portability and the ease with which its use can be learned. Increased independence and better compliance have also been cited as advantages of this technique. However, frequent assessment of patient technique and appropriate level of resistance is recommended.87
Preparation for Positive Expiratory Pressure
 Several different devices are available to deliver positive expiratory pressure with a steady level of resistance or oscillatory flow. The practitioner should be familiar with the specific device being used to provide adequate instructions to the patient and family.
Several different devices are available to deliver positive expiratory pressure with a steady level of resistance or oscillatory flow. The practitioner should be familiar with the specific device being used to provide adequate instructions to the patient and family.
 A mask can be used in place of the mouthpiece on most PEP devices (for adults and children) and is preferred by some practitioners. The rationale for using a mask is that the lung volumes should be increased during the entire phase of exhalation through the PEP device, which is more difficult to achieve when using a mouthpiece because the patient may open the mouth around the mouthpiece at the end of expiration causing a fall in lung volumes.123 The use of nose clips is recommended when using a mouthpiece.
A mask can be used in place of the mouthpiece on most PEP devices (for adults and children) and is preferred by some practitioners. The rationale for using a mask is that the lung volumes should be increased during the entire phase of exhalation through the PEP device, which is more difficult to achieve when using a mouthpiece because the patient may open the mouth around the mouthpiece at the end of expiration causing a fall in lung volumes.123 The use of nose clips is recommended when using a mouthpiece.
 A manometer can be placed proximal to the resistor in the initial stages of instruction in the use of PEP in most devices. First, the manometer helps to determine and monitor the appropriate level of resistance needed for the patient to achieve 10 to 20 cm of H2O throughout exhalation. Second, the visual display of the manometer serves as feedback to assist the patient in mastering the technique.95
A manometer can be placed proximal to the resistor in the initial stages of instruction in the use of PEP in most devices. First, the manometer helps to determine and monitor the appropriate level of resistance needed for the patient to achieve 10 to 20 cm of H2O throughout exhalation. Second, the visual display of the manometer serves as feedback to assist the patient in mastering the technique.95
 Aerosol medication delivered by nebulizer may be placed inline in many devices to be delivered simultaneously with PEP for airway clearance, improving the deposition of medication.109,124 If aerosolized medication is to be used simultaneously, the patient should be instructed in how to stop the flow of the aerosol when the mask or mouthpiece is removed during the PEP treatment session for coughing. Supplemental oxygen may also be placed inline in many devices for patients who require this.
Aerosol medication delivered by nebulizer may be placed inline in many devices to be delivered simultaneously with PEP for airway clearance, improving the deposition of medication.109,124 If aerosolized medication is to be used simultaneously, the patient should be instructed in how to stop the flow of the aerosol when the mask or mouthpiece is removed during the PEP treatment session for coughing. Supplemental oxygen may also be placed inline in many devices for patients who require this.
 Bubble PEP is a variation of positive expiratory pressure that is particularly useful when treating children. Equipment needed includes a length of tubing 15 to 18 inches long and a plastic container filled with a column of water 13 cm high (this will generate a positive expiratory pressure of around 20 cm of H2O). A few drops of food coloring and/or 3 to 6 squirts of liquid detergent or bubble liquid may be added to make the treatment more entertaining. Place the tubing at the very bottom of the container—it is important that the tube remain at the base of the column of water to generate the required expiratory pressure. If detergent or bubbles are included, place the container in a large bowl or on a towel to contain the overflow.123
Bubble PEP is a variation of positive expiratory pressure that is particularly useful when treating children. Equipment needed includes a length of tubing 15 to 18 inches long and a plastic container filled with a column of water 13 cm high (this will generate a positive expiratory pressure of around 20 cm of H2O). A few drops of food coloring and/or 3 to 6 squirts of liquid detergent or bubble liquid may be added to make the treatment more entertaining. Place the tubing at the very bottom of the container—it is important that the tube remain at the base of the column of water to generate the required expiratory pressure. If detergent or bubbles are included, place the container in a large bowl or on a towel to contain the overflow.123
 All PEP devices should be cleaned regularly with hot, soapy water; many can be cleaned in a dishwasher. In the hospital, the equipment should be sterilized according to infection control recommendations.
All PEP devices should be cleaned regularly with hot, soapy water; many can be cleaned in a dishwasher. In the hospital, the equipment should be sterilized according to infection control recommendations.
Treatment with Positive Expiratory Pressure
 To determine the correct level of resistance for PEP, the patient inhales using tidal volume and exhales actively into the mask or mouthpiece. The resistor valve is adjusted while the level of PEP is monitored on the manometer. The resistance is gradually decreased until the PEP level supplying 10 to 20 cm of water pressure has been identified.113 Mahlmeister95 reports most patients achieve this pressure range with flow resistors of 2.5 to 4.0 mm in diameter. Selection of the proper resistor produces the desired inspiratory to expiratory ratio of 1 : 3 or 1 : 4.95 The use of too great a resistance will create an increased respiratory rate or too low a pressure, whereas too small a resistor will create a slow respiratory rate or too high a pressure.125
To determine the correct level of resistance for PEP, the patient inhales using tidal volume and exhales actively into the mask or mouthpiece. The resistor valve is adjusted while the level of PEP is monitored on the manometer. The resistance is gradually decreased until the PEP level supplying 10 to 20 cm of water pressure has been identified.113 Mahlmeister95 reports most patients achieve this pressure range with flow resistors of 2.5 to 4.0 mm in diameter. Selection of the proper resistor produces the desired inspiratory to expiratory ratio of 1 : 3 or 1 : 4.95 The use of too great a resistance will create an increased respiratory rate or too low a pressure, whereas too small a resistor will create a slow respiratory rate or too high a pressure.125
 For high-pressure PEP, appropriate resistance is determined by connecting the outlet of the PEP mask to a spirometer. The resistor producing the highest forced vital capacity through the PEP mask is selected for continued use.115 The patient breathes in and out through the mask at tidal volume for 6 to 10 breaths; then inspiration is done to total lung capacity and a forced expiratory maneuver is performed against the PEP mask. This is repeated until all the mucus is mobilized.125
For high-pressure PEP, appropriate resistance is determined by connecting the outlet of the PEP mask to a spirometer. The resistor producing the highest forced vital capacity through the PEP mask is selected for continued use.115 The patient breathes in and out through the mask at tidal volume for 6 to 10 breaths; then inspiration is done to total lung capacity and a forced expiratory maneuver is performed against the PEP mask. This is repeated until all the mucus is mobilized.125
 For a PEP therapy treatment, the patient should be seated upright with elbows resting on a table. Use of a mask may require securing the device with both hands for a tight seal. If needed, the patient may be in a reclining position for all PEP devices except the Flutter, which is position dependent. To use the Flutter valve, the patient should be seated upright (Figure 21-10).
For a PEP therapy treatment, the patient should be seated upright with elbows resting on a table. Use of a mask may require securing the device with both hands for a tight seal. If needed, the patient may be in a reclining position for all PEP devices except the Flutter, which is position dependent. To use the Flutter valve, the patient should be seated upright (Figure 21-10).
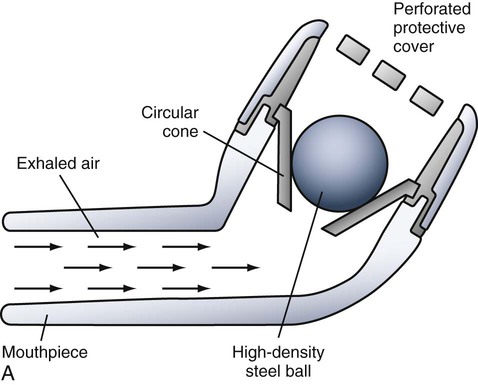
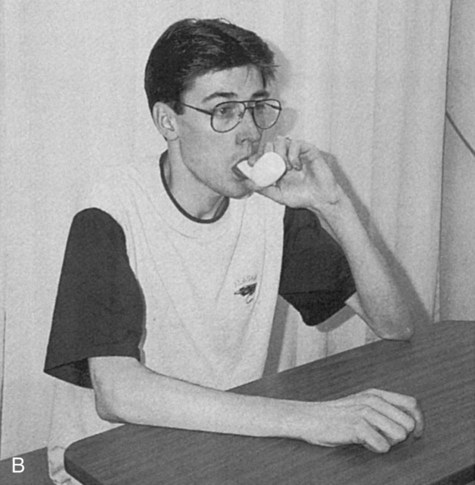
 The patient should be instructed to breathe into the mask or mouthpiece to tidal volume, using the lower chest and abdomen, and pause for an inspiratory hold for 2 to 3 seconds to equalize ventilation before exhaling.123 Exhalation into the mask or mouthpiece should be slightly active but not forced. The patient continues breathing into the mask or mouthpiece for 10 to 15 breaths, using a normal respiratory rate. After a series of 10 to 15 breaths, the mask or mouthpiece is removed from the face and the patient performs a series of huffs and/or coughing to expectorate any mucus that has been mobilized.126 It may be necessary to pause every 5 to 10 exhalations before resuming the session.118
The patient should be instructed to breathe into the mask or mouthpiece to tidal volume, using the lower chest and abdomen, and pause for an inspiratory hold for 2 to 3 seconds to equalize ventilation before exhaling.123 Exhalation into the mask or mouthpiece should be slightly active but not forced. The patient continues breathing into the mask or mouthpiece for 10 to 15 breaths, using a normal respiratory rate. After a series of 10 to 15 breaths, the mask or mouthpiece is removed from the face and the patient performs a series of huffs and/or coughing to expectorate any mucus that has been mobilized.126 It may be necessary to pause every 5 to 10 exhalations before resuming the session.118
 The series of PEP breaths followed by huffs should be repeated about four to six times. The total treatment lasts about 15 to 20 minutes and should be performed twice during the day or as needed. The frequency and duration of the treatment must be individualized for each patient. During periods of pulmonary exacerbation, patients are encouraged to increase the frequency of PEP treatments rather than extend the length of individual sessions.95 Some patients have a tendency to hyperventilate and become dizzy; an inspiratory pause will prevent this.123
The series of PEP breaths followed by huffs should be repeated about four to six times. The total treatment lasts about 15 to 20 minutes and should be performed twice during the day or as needed. The frequency and duration of the treatment must be individualized for each patient. During periods of pulmonary exacerbation, patients are encouraged to increase the frequency of PEP treatments rather than extend the length of individual sessions.95 Some patients have a tendency to hyperventilate and become dizzy; an inspiratory pause will prevent this.123
 Initially, the patient and caregiver monitor the effort by means of the manometer, ensuring that a pressure of 10 to 20 cm of H2O is achieved throughout exhalation (this is not possible with the Flutter). After the technique is mastered with the appropriate resistor, the manometer may be removed from the system. The appropriate resistance should be rechecked periodically during clinical visits or periods of hospitalization.
Initially, the patient and caregiver monitor the effort by means of the manometer, ensuring that a pressure of 10 to 20 cm of H2O is achieved throughout exhalation (this is not possible with the Flutter). After the technique is mastered with the appropriate resistor, the manometer may be removed from the system. The appropriate resistance should be rechecked periodically during clinical visits or periods of hospitalization.
 For Bubble PEP, the patient is instructed to blow through the tube with enough force to cause the bubbles to rise up to the top of the container. After a number of breaths, the patient is asked to do huffing or coughing before resuming the treatment. The therapist may prescribe the height of the column of water to alter the pressure, the number of breaths taken, and the huffs or coughs needed to tailor the treatment to each patient.123
For Bubble PEP, the patient is instructed to blow through the tube with enough force to cause the bubbles to rise up to the top of the container. After a number of breaths, the patient is asked to do huffing or coughing before resuming the treatment. The therapist may prescribe the height of the column of water to alter the pressure, the number of breaths taken, and the huffs or coughs needed to tailor the treatment to each patient.123
Advantages and Disadvantages of Positive Expiratory Pressure
PEP therapy does not possess some of the limitations of conventional PD and percussion for secretion clearance and is therefore applicable to a wider patient population. It is relatively easy to learn in one or two sessions and may be applied equally to the pediatric (children over 4 years of age) and adult populations. PEP is appropriate for use during acute episodes in hospitalized patients, as well as for long-term use for chronic pulmonary conditions. The expense of the equipment is minimal, and once the patient is competent in the technique, it provides independence (except for small children). All PEP devices are quite portable, making airway clearance easier to perform during travel or when away from home during the day. PEP devices can be used in any position except the Flutter, which is position dependent. Some musical instruments can provide a form of PEP therapy because of the manner in which they are played, with an inspiratory pause and resisted exhalation.123 These instruments include the clarinet, oboe, bassoon, French horn, trumpet, flute, and voice. Low-pressure PEP is more commonly used in North America because it is believed to be not only as effective as high-pressure PEP, but also easier and safer to use and monitor. In those patients in whom PEP is an appropriate airway clearance technique, a high degree of acceptance has been shown.112,117,127 This may translate into better adherence in the long term.
A decision to use PEP should be carefully evaluated in cases of acute sinusitis, ear infection, epistaxis, and recent oral or facial surgery or injury.95 For PEP therapy to be effective, a patient should be able to cooperate and actively participate with the treatment. Although rare, pneumothorax has been reported with high-pressure PEP.115
Precautions for Positive Expiratory Pressure
The use of PEP for airway clearance carries an increased risk for pneumothorax.115 Bronchodilator premedication should be considered when applying PEP in patients who show clinical or physiological signs of airway hyperreactivity.105
The increased airflow produced by the huff cough, as in the ACBT, may aggravate bronchospasm.90 Additionally, Hietpas90 cautions that the movement of secretions into the larger airways by the huff cough may precipitate spontaneous explosive coughing.
High-Frequency Chest Wall Oscillation
Efforts aimed at mucus clearance by creating a differential airflow rate led to the development of a high-frequency chest wall oscillation (HFCWO) system. Hansen and Warwick128 designed a large-volume, variable-frequency air-pulse delivery system that can be used by patients with obstructive lung disease to promote mucus clearance.
High-frequency chest wall oscillation, also referred to as high-frequency chest compression, consists of an inflatable vest linked to an air-pulse generator. Although the sensation of the device is somewhat akin to mechanical percussion, it differs significantly in its mechanism of action. HFCWO works by differential airflow (i.e., the expiratory flow rate is higher than the inspiratory flow rate), allowing the mucus to be transported from the periphery to the central airways for expectoration (Figure 21-11). HFCWO has also been shown to decrease the viscosity of mucus, making it easier to mobilize.
The first HFCWO system developed was the Vest (Hill ROM, St. Paul, Minnesota), consisting of an inflatable fitted vest connected to an air-pulse generator by flexible tubing. This device provides oscillation of the entire thoracic cavity at varying frequencies (5 to 25 Hz). The lung volume expired tends to increase with lower frequencies (less than 10 to 12 Hz), whereas the flow rates tend to increase with higher frequencies (12 to 20 Hz). Continuous aerosolized medication or saline administered concurrently may assist with secretion mobilization.129 The original, larger unit of the Vest is best used in a clinical setting; it can be placed on a wheeled stand for easy mobility. Newer models weigh as little as 17 pounds, providing more mobility than earlier models; these units fit under an airplane seat and are easier to manage during travel.
Two probable mechanisms of action have been offered to explain the significant increase in sputum mobilization that occurs with HFCWO.130 One mechanism proposes that oscillatory airflow leads to changes in the consistency of mucus, which results in increased mobilization of secretions. Considerable decreases in mucus viscoelasticity were observed during administration of oscillatory airflow.131 Another mechanism proposes that the difference between the expiratory and inspiratory velocities produces shear forces strong enough to move mucus. Chang and colleagues132 demonstrated that nonsymmetrical airflow (peak expiratory flow rates greater than inspiratory flow rates) could be an important factor leading to increases in mucus clearance during the administration of HFCWO. The chest compressions produce a transient flow pulse similar to that observed during coughing, and by using the flows with the greatest rates and volumes, sufficient force is obtained to move mucus in the airway.133
HFCWO has been shown to increase mucus clearance rates in animal models, with the most pronounced effect in the 11 to 15 Hz frequency range.134 Radford and colleagues68 used bronchoscopy to demonstrate a marked increase in the speed and flow of mucus produced by oscillations at even higher frequencies than those attainable by manual percussion. Results of short-term use of the Vest have been mixed, but they show HFCWO to be at least as effective as conventional CPT. Robinson135 showed no significant improvement or deterioration of lung function with its use. In additional studies, Kluft and Faverio136,137 demonstrated increased wet and dry sputum weights using HFCWO as opposed to manual CPT, and Arens (1993)138 showed similar dry sputum weight but an increase in wet sputum weight and a significant improvement in pulmonary function with HFCWO as opposed to conventional CPT. One 2-year study showed improved lung function and greater sputum production in subjects with cystic fibrosis with the use of HFCWO rather than manual CPT.133 No adverse effects were observed with long-term use of the Vest. Hospitalized patients with acute exacerbation of lung disease have been shown to tolerate HFCWO well,139 and the safety and tolerance of this method have been demonstrated in long-term mechanically ventilated patients.140
The fit of the vest requires attention because nausea, abdominal and chest wall discomfort, and complaints of urinary urgency may occur with an ill-fitting vest.106 HFCWO systems are much more costly than other mechanical aids for airway clearance; thus expense may be a deterrent for some potential users. However, in a study of HFCWO users insured by Blue Cross and Blue Shield, a 49% reduction in health care costs was shown in the year following initial use of the vest as compared with the year before HFCWO use.141 The impact of the use of the HFCWO device in a hospital department demonstrated a substantial savings resulting from therapy self-administration by patients.142
Preparation for High-Frequency Chest Wall Oscillation
 In order to provide adequate instructions to the patient and family, the practitioner should be familiar with the specific HFCWO device being used. The various models of inflatable vests are constructed to fit the thorax differently and are available in different sizes (from toddler to large adult). A full vest model should extend to the top of the thigh when the patient is sitting upright. A shorter vest (chest vest) is also available, resulting in less pressure to the abdominal area and less gastric discomfort. The vest should fit properly, but breathing should not feel restricted while the vest is deflated. A single layer of clothing or patient gown should be worn under the vest. For the hospital setting, adjustable vests are available for use with multiple patients (following appropriate infection control guidelines for cleaning). For home use, each patient should be fitted for his or her own vest.
In order to provide adequate instructions to the patient and family, the practitioner should be familiar with the specific HFCWO device being used. The various models of inflatable vests are constructed to fit the thorax differently and are available in different sizes (from toddler to large adult). A full vest model should extend to the top of the thigh when the patient is sitting upright. A shorter vest (chest vest) is also available, resulting in less pressure to the abdominal area and less gastric discomfort. The vest should fit properly, but breathing should not feel restricted while the vest is deflated. A single layer of clothing or patient gown should be worn under the vest. For the hospital setting, adjustable vests are available for use with multiple patients (following appropriate infection control guidelines for cleaning). For home use, each patient should be fitted for his or her own vest.
 Simultaneous use of aerosolized medication is recommended for use throughout the treatment. This humidifies the air to counteract the drying effect of the increased airflow.
Simultaneous use of aerosolized medication is recommended for use throughout the treatment. This humidifies the air to counteract the drying effect of the increased airflow.
Treatment with High-Frequency Chest Wall Oscillation
 The patient should be seated upright in a chair, and the tubing should be securely connected to the air pulse generator. Start the aerosol therapy before turning on the HFCWO system.
The patient should be seated upright in a chair, and the tubing should be securely connected to the air pulse generator. Start the aerosol therapy before turning on the HFCWO system.
 The pressure control setting should be adjusted according to patient comfort, opting for the highest pressure that is well tolerated.
The pressure control setting should be adjusted according to patient comfort, opting for the highest pressure that is well tolerated.
 The treatment should progress through different frequencies, from low (7 to 10 Hz) to medium (10 to 14 Hz) and then to high (14 to 20 Hz), to achieve both higher flow rates and increased lung volume. Warwick133 reported that the frequencies associated with the highest flow rates were usually greater than 13 Hz, whereas those associated with the largest volume were usually less than 10 Hz. The average length of time spent at each frequency is 10 minutes, but this will vary according to patient tolerance, amount and consistency of secretions, and the acuity of the patient’s illness. After treatment at each frequency for the prescribed length of time, the patient should be instructed to huff or cough to clear loosened secretions.
The treatment should progress through different frequencies, from low (7 to 10 Hz) to medium (10 to 14 Hz) and then to high (14 to 20 Hz), to achieve both higher flow rates and increased lung volume. Warwick133 reported that the frequencies associated with the highest flow rates were usually greater than 13 Hz, whereas those associated with the largest volume were usually less than 10 Hz. The average length of time spent at each frequency is 10 minutes, but this will vary according to patient tolerance, amount and consistency of secretions, and the acuity of the patient’s illness. After treatment at each frequency for the prescribed length of time, the patient should be instructed to huff or cough to clear loosened secretions.
 HFCWO has also been used with patients requiring long-term mechanical ventilation. Whitman and colleagues140 found use of HFCWO to be safe and effective and concluded that it resulted in time savings over conventional PD and percussion.
HFCWO has also been used with patients requiring long-term mechanical ventilation. Whitman and colleagues140 found use of HFCWO to be safe and effective and concluded that it resulted in time savings over conventional PD and percussion.
 Patients with long-term central intravenous access such as a Porta-Cath or Hickman are able to use HFCWO with sufficient padding (such as a foam doughnut pillow) to relieve pressure around the access site.
Patients with long-term central intravenous access such as a Porta-Cath or Hickman are able to use HFCWO with sufficient padding (such as a foam doughnut pillow) to relieve pressure around the access site.
Advantages and Disadvantages of High-Frequency Chest Wall Oscillation
A disadvantage of HFCWO as a method of airway clearance is the cost of the equipment. A study by Ohnsorg,141 however, demonstrated a decline in total health care costs for the year after HFCWO was put into use by 11 patients. A study of the impact of the device in a hospital setting142 reported a substantial savings as a result of therapy self-administration. Replacement of the equipment should not be a factor, because a lifetime warranty is available for the devices.
Intrapulmonary Percussive Ventilation
Intrapulmonary percussive ventilation (IPV) is an airway clearance method that simultaneously delivers intrathoracic percussion and aerosolized solution for bronchodilation.143 An apparatus known as the Phasitron is the functional component in the intrapulmonary percussive ventilator. The Phasitron provides high-frequency impulses during inspiration, while positive expiratory pressure is maintained throughout passive exhalation. The pressure generated is between 10 and 30 cm of H2O.
It is theorized that changes in the frequency and pressure of the airflow delivered through the IPV device assist in stabilizing the airways and decrease the viscosity of the secretions; this results in increased sputum mobilization.106 IPV has been found to be as effective as postural drainage and percussion in improving pulmonary function and sputum expectoration.144 Marks145 found no difference between IPV and Flutter in number of hospital or antibiotic days required to treat an exacerbation and reported good acceptance of this method of airway clearance by patients. IPV may be beneficial for patients with asthma and neuromuscular disease, as well as those with cystic fibrosis.146,147
Treatment with Intrapulmonary Percussive Ventilation
 One IPV model meant for institutional use is the Percussionaire Model IPV-1, which is powered by 50 psi of gas. Percussive rates or frequencies range from less than 100 to greater than 225 cycles per minute. This model has the capability to be used with an endotracheal tube and can be installed on a wheeled stand for greater mobility. Use of the hospital unit must be supervised by a respiratory care practitioner.
One IPV model meant for institutional use is the Percussionaire Model IPV-1, which is powered by 50 psi of gas. Percussive rates or frequencies range from less than 100 to greater than 225 cycles per minute. This model has the capability to be used with an endotracheal tube and can be installed on a wheeled stand for greater mobility. Use of the hospital unit must be supervised by a respiratory care practitioner.
 The Percussionaire Impulsator is self-contained for home use and powered by a compressor, but it may also be used in a clinical situation. It generates 40-psi source pressure, which provides for efficient delivery of impulses and aerosolized medication. Condensation is minimal compared with institutional models, so maintenance on the unit is low. The patient and caregivers must receive training to use the home unit.
The Percussionaire Impulsator is self-contained for home use and powered by a compressor, but it may also be used in a clinical situation. It generates 40-psi source pressure, which provides for efficient delivery of impulses and aerosolized medication. Condensation is minimal compared with institutional models, so maintenance on the unit is low. The patient and caregivers must receive training to use the home unit.
 A new model by Percussionaire, the HC Impulsator, is a portable IPV device that weighs less than 15 pounds, allowing patients to use it when traveling.
A new model by Percussionaire, the HC Impulsator, is a portable IPV device that weighs less than 15 pounds, allowing patients to use it when traveling.
 Aerosolized medication in saline solution is delivered via the nebulizer component of the IPV unit.
Aerosolized medication in saline solution is delivered via the nebulizer component of the IPV unit.
 Treatment with IPV is titrated for patient comfort and visible thoracic movement. A thumb button is held for 5- to 10-second intervals to initiate the percussive impulses and released after an interval to allow exhalation. After each deep exhalation, the percussive interval starts again. When the patient needs to cough or expectorate, the thumb button is released until coughing is completed or secretions are cleared.
Treatment with IPV is titrated for patient comfort and visible thoracic movement. A thumb button is held for 5- to 10-second intervals to initiate the percussive impulses and released after an interval to allow exhalation. After each deep exhalation, the percussive interval starts again. When the patient needs to cough or expectorate, the thumb button is released until coughing is completed or secretions are cleared.
 The clinician or the patient at home programs each percussive interval. An average treatment lasts about 20 minutes.
The clinician or the patient at home programs each percussive interval. An average treatment lasts about 20 minutes.
Advantages and Disadvantages of Intrapulmonary Percussive Ventilation
IPV is available for home use and can be continued during hospitalization. IPV allows for greater independence for adolescents and adults with long-term need for airway clearance. Homnick143 reported that three-fourths of the patients using IPV in one study estimated increased sputum production, and satisfaction was high for comfort and independence. IPV provides a safe and effective form of airway clearance.148
IPV is neither appropriate for nor tolerated by young children. In other patients, a feeling of claustrophobia or chest fullness may be a factor in deciding whether to use IPV.106 The IPV device is more expensive than a PEP device but less costly than a unit for HFCWO. The availability of IPV in the clinical setting is not as common as other airway clearance devices; therefore, respiratory care practitioners may not be as familiar or comfortable with its application. The use of IPV may increase as more patients request alternative methods of airway clearance and as more research is done to demonstrate its benefits.
Acoustic Airway Clearance
A recent form of airway clearance uses acoustic vibrations to clear secretions from the lungs. The Frequencer (Dymedso Inc., Boisbriand, Quebec) is a device that provides mechanical vibration in addition to acoustic oscillation to mobilize secretions through a variety of tissue depths. The sound level (56-78 dB) generated at maximal power is below the level that would cause hearing damage.149 Normal human hearing is limited to frequencies of 20 to 20,000 Hz, and the Frequencer operates between 20 and 65 Hz. The device adjusts to the resonant frequency of the airways of the lungs and is able to target small portions of the lungs as opposed to affecting the entire lung fields at once. It is similar to HFCWO in that the vibrations thin the viscosity of the pulmonary secretions. However, unlike HFCWO, which has an upper frequency of 25 Hz, the frequency of oscillation provided by the Frequencer is substantially higher at 20 to 65 Hz.
In a pilot study comparing the Frequencer with traditional postural drainage and percussion, the amount of sputum produced by the Frequencer was the same as or more than PD and patients reported less discomfort.149 Another small study by Vallejos150 described the use of the Frequencer in a clinical environment; treatment with the device produced sputum 75% of the time, and patients showed a preference for ACT by this method.
Treatment with Acoustic Airway Clearance
 The Frequencer consists of a control unit that generates acoustic waves in a range of frequencies and a transducer head to deliver the oscillation to a specific area of the lung. The treatment settings are changed by using a touch screen, and the settings can be locked to prevent accidental alterations. Intensity and frequency levels can be adjusted by sliding buttons up and down.
The Frequencer consists of a control unit that generates acoustic waves in a range of frequencies and a transducer head to deliver the oscillation to a specific area of the lung. The treatment settings are changed by using a touch screen, and the settings can be locked to prevent accidental alterations. Intensity and frequency levels can be adjusted by sliding buttons up and down.
 Four sizes of adapters for the transducer are available to accommodate patients of varying body sizes. The control unit displays suggested levels of treatment for babies, children, and adults.
Four sizes of adapters for the transducer are available to accommodate patients of varying body sizes. The control unit displays suggested levels of treatment for babies, children, and adults.
 There are six suggested chest treatment areas with a recommended 3-minute duration for each area.
There are six suggested chest treatment areas with a recommended 3-minute duration for each area.
Factors Affecting Selection of Airway Clearance Techniques
Among patients with pulmonary disorders, poor adherence to the performance of airway clearance on a regular basis has been well documented.4,151–153 Litt151 has shown that the complexity and increased duration of a prescribed treatment has a negative influence on patient adherence. It has been suggested that better adherence may be achieved if the treatment is specifically tailored to the individual patient’s needs with regard to clinical status, family functioning, and family concerns (Box 21-6). Negotiation between the patient and the caregiver is also effective; patients are more likely to adhere to a prescribed treatment regimen to which they have agreed in collaboration with their caregiver.154 The regular use of a particular ACT by a patient is governed by personal belief in the effectiveness of the method for his or her own disease process, the manner in which the method affects the family’s life habits, and the patient’s willingness to use the technique on a daily basis. Adherence is ultimately the best index of an ACT’s effectiveness. For this reason, it is incumbent upon caregivers to consider the many factors that may alter a patient’s adherence to a particular method when recommending a specific technique, especially in a patient with a chronic disease. These factors include the availability of the caregiver to teach the technique and the willingness of the patient to learn it; the patient’s concurrent medical problems; the effectiveness of the technique (subjective and objective); support for the technique from family, friends, and health care personnel; age and lifestyle of the patient; and the cost of the treatment.106 Table 21-1 summarizes factors that can influence the choice of an airway clearance technique.
Table 21-1
Considerations When Selecting an Airway Clearance Technique
| Technique | Age of Patient | Assistant Needed | Equipment Needed | During Acute Exacerbation | Concurrent Nebulizer | Precautions | Cost |
| PD, percussion, vibration/shaking | Any age | Yes | Positioning aids; percussor/vibrator; devices for infants | Yes | Only in upright or side-lying | May need to modify positions; repetitive motion injuries | Expensive if performed by caregiver over long term |
| ACBT | Begin to teach at 3-4 years of age | Until 8-10 years of age | Positioning aids; percussor/vibrator | Yes | Only in upright or side-lying | Precautions for head-down positions | Inexpensive if done independently |
| AD | Age ≥12 years | No | None | Best to use an alternative | No | Takes time to learn | No cost |
| HFCWO | Age ≥2-3 years | For young children | Air pulse generator; appropriately sized vest | Yes | Yes | Chest tube, indwelling catheter, or other device in chest area | Very expensive |
| IPV | Adolescents and adults | While in hospital | Home unit or hospital unit | May not be well tolerated | Yes | Titrate for comfort and visible chest movement | Moderately expensive |
| Acoustic Airway Clearance | All ages | For children | Acoustic generator and appropriate size transducer | Possibly; further studies are needed | Yes | Further studies are needed | Very expensive |
| Exercise | Children, adolescents, and adults | For young children | Variable | No | Premedicate before exercise | Exercise-induced bronchospasm; oxygen desaturation; adjunct to ACT | Depends on type of exercise |
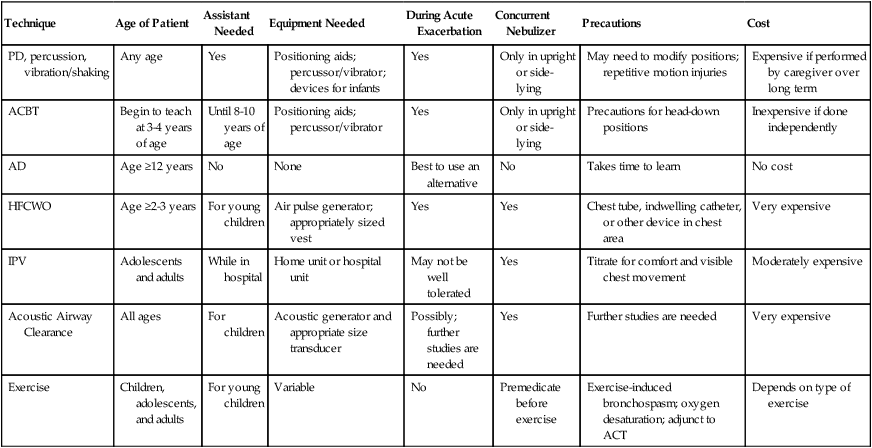
Summary
Numerous ACTs have been shown to reduce obstruction, enhance mucociliary clearance, and improve ventilation, accomplishing the goal of improved oxygen transport. The effectiveness of various techniques has been demonstrated in multiple studies and evaluated with numerous outcome measures. In some cases, routine application of ACTs has not been shown to be effective in achieving improved oxygen transport. Acute asthma, bronchitis, pneumonia without copious secretions, bronchiolitis, and routine postoperative conditions were not shown to benefit from PD, percussion, and vibration.18,21 ACTs are not without side effects or complications; routine use of these methods is not recommended without clear indications. Indications for ACTs have been established for acute illness and for chronic conditions. In acute illness, traditional methods (i.e., PD, percussion, and vibration) have been shown to be beneficial in patients with copious secretions and in the treatment of atelectasis.155 For patients with cystic fibrosis, treatment with PEP and exercise in conjunction with PD, percussion, and vibration were also shown to be effective in an acute exacerbation.156 In chronic disease states, patients with cystic fibrosis and bronchiectasis have been found to benefit from PD, percussion, and vibration, as well as PEP, autogenic drainage, ACBT, acoustic airway clearance, IPV, and exercise.106,149,155,156








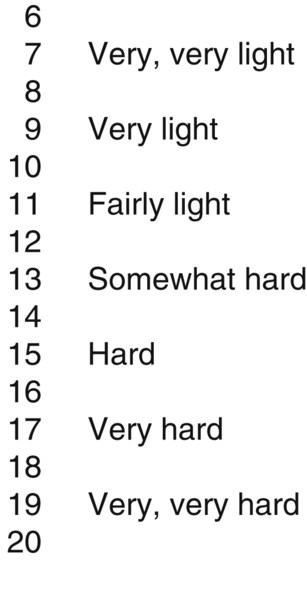





















































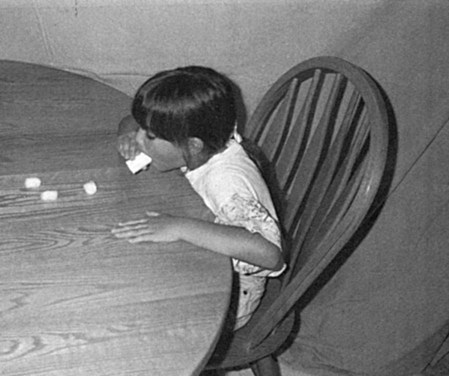
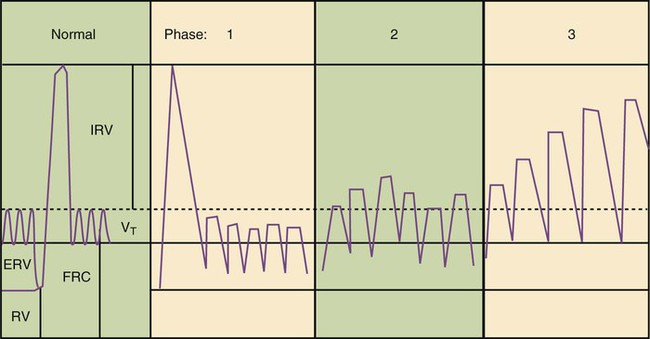
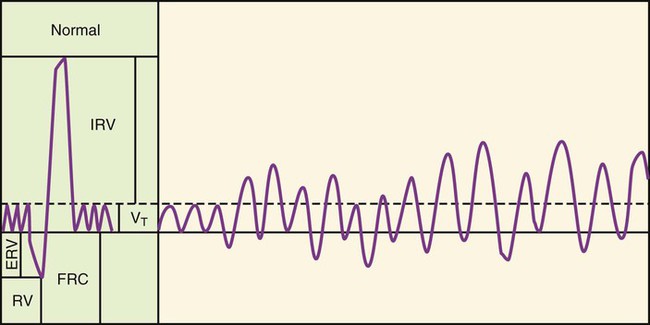
 -mm resistor is used for infants, a resistor of up to
-mm resistor is used for infants, a resistor of up to  to 3 mm for older children and adults, and
to 3 mm for older children and adults, and  mm for adults with COPD.
mm for adults with COPD.




































