Air Medical Transport
Perspective
The impact of AMT on the wounded soldier was clear. During World War II, the average time from injury to definitive care was 6 to 12 hours, with a mortality rate of 5.8%. In Korea, the time was 2 to 4 hours, with 2.4% mortality. In Vietnam, the time was 65 minutes, and mortality was less than 1%.1 Encouraged by the military experience, civilian AMT in the United States was propelled by the 1969 start of the first hospital-sponsored, fixed-wing air medical program. The first civilian helicopter emergency medical services (HEMS) program in the United States was established in 1972.
Aviation Physiology
A working knowledge of aviation physiology is vital to understanding of the effects of AMT on pilots, medical personnel, and patients.2
Boyle’s Law
Physiologic difficulties from expansion and contraction of gases within the closed spaces of the body may occur with altitude change. Squeeze injuries from contraction of air and associated soft tissues within closed cavities occur on descent and are common causes of barotitis, barosinusitis, and toothache. Reverse squeeze injuries occur on ascent, as decreasing barometric pressure leads to an increased volume of the air trapped within the space, exerting pressure on structures. Ascent injuries can include conversion of a simple pneumothorax into a tension pneumothorax or rupture of a hollow viscus by expansion of intestinal gas. The operation of medical equipment containing closed air spaces, such as intravenous tubing and pumps, air splints, ventilators, and endotracheal tube and laryngeal airway cuffs, may also be affected by altitude.3–7
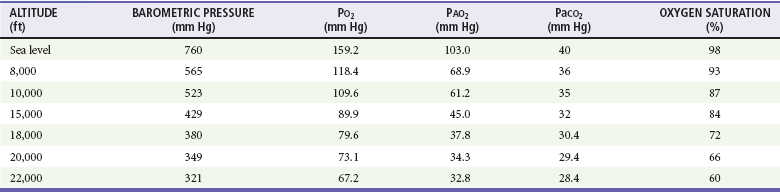
Dalton’s Law
Dalton’s law states that the total barometric pressure at any given altitude equals the sum of the partial pressures of gases in the mixture (Pt = P1 + P2 + P3 … Pn). Whereas oxygen still constitutes 21% of the atmospheric pressure at altitude, Boyle’s law notes that each breath brings fewer oxygen molecules per breath to the lungs, and hypoxia results (Table 191-1). The clinical effect of Dalton’s law is manifested as a decrease in arterial oxygen tension with increasing altitude.
Principles of Air Medical Transport Systems
Air medical services may take several forms. Despite a tremendous growth of operations in the past 20 years, the most common type of HEMS program in the United States remains the hospital-sponsored operation transporting patients from outlying referral centers or accident scenes to tertiary care centers. A single hospital or a consortium of institutions may sponsor these flight programs. In 2011, there were more than 220 dedicated HEMS programs operating more than 750 dedicated aircraft throughout the nation.8 Approximately 54% of the programs were hospital sponsored, and the balance were operated by privately owned or publically traded companies. Whereas these for-profit companies represent 46% of the programs, they operate more than 61% of the dedicated helicopters in the United States.8 Public service agencies may also sponsor air medical services or partner with private companies; vehicles used by these programs are often multifunctional aircraft that serve in medical, search and rescue, fire suppression, and law enforcement roles. The Military Assistance to Safety and Traffic (MAST) program operated by the U.S. Armed Forces provides additional HEMS resources to the community,9 but in recent years their role for civilian support has been generally limited to Hawaii and Alaska.9 Together, the public service and MAST helicopters add more than 120 additional aircraft available for patient transport.8 There is no accurate accounting of the number of fixed-wing air ambulance companies or airplanes. Although some hospitals do sponsor fixed-wing AMT, it is more common for these programs to be private fee-for-service operations.
Air Medical Aircraft
Helicopters (Rotor-Wing Aircraft)
Disadvantages to HEMS include noise, vibration, thermal variances, and other stressors on patients and crew exaggerated by rotor-wing flight. Weather considerations may significantly limit the availability of helicopter transport. In smaller aircraft, cramped spaces and weight limitations may limit the number of patients, transport personnel, or equipment that can be carried. This may sometimes compromise optimal patient care (Fig. 191-1).
Air Medical Flight Crew
Air medical crew members represent the broad spectrum of health care providers. AMT services that provide critical care transport, advanced life support, or specialty care transport must staff the vehicle with a minimum of two medical personnel to provide direct patient care.10,11 The majority of AMT programs in the United States provide critical care transport teams composed of one registered nurse and an additional crew member (paramedic, respiratory therapist, physician, or a second nurse); most common is the nurse-paramedic crew.12 AMT crew configuration may also be mission dependent. A service may at times believe that it is appropriate to use a single medical crew member. For example, it may be appropriate while transporting a stable patient on a routine interfacility transport. Certain flight conditions and situations may also necessitate flying with a single crew member, including heat, humidity, altitude, distance, fuel on board, and weight of the patient.12
The AMT environment imposes unique considerations on the air medical flight crew that can influence their ability to provide patient care. Human factors work has shown that most medical care procedures are more difficult to perform in an AMT vehicle than in other ground-based settings.13 Auscultation of the heart and lungs, palpation of pulses, performance of cardiopulmonary resuscitation, endotracheal intubation, radio communications while using a respirator or face mask, and recognition of visual alarms may all be impaired while aloft.14–19 In addition, fatigue, motion sickness, exposure to engine exhausts, an erratic pattern of work activity, and the high risk involved in AMT operations may affect task performance significantly.20–22 Seizures from photic stimuli associated with rotor motion (“flicker illness”) has also been reported.23 High-fidelity simulation of air medical missions can acquaint flight crew to the novel environment, but fiscal and personnel costs may be prohibitive.24
Medical Direction
All air medical services require the active involvement of a physician as medical director responsible for supervising, evaluating, and ensuring the quality of medical care provided by the AMT team.25 Emergency physicians play a significant role, with nearly 50% of all air medical directors having a background in emergency medicine.26 The medical director must have the final authority over all clinical aspects of the air medical service and should ensure that the flight crew have adequate training and qualifications to optimize patient care. Medical care policies and procedures should be established, including specific provisions for on-line and off-line medical control. The Air Medical Physician Association and the National Association of EMS Physicians have established guidelines for the medical director of an air medical service.27,28
Safety
Safety is the predominant concern of air medical operations, and ensuring safe flight is a fundamental part of every flight program.29 Safety must also be an overriding consideration in weighing the risks and benefits of AMT. The role of aircraft pilots and mechanics is essential to the airworthiness of the vehicle, and medical personnel must also be proficient in both routine and emergency operations in and around the aircraft. Checklists may aid in safety practices but alone may not detect significant operational concerns.30 Crew fatigue and other self-imposed stresses that could affect safety, such as the use of prescription or over-the-counter medications, tobacco, and alcohol, must be scrupulously avoided.
The practice of “helicopter shopping” has been a major factor in a number of fatal HEMS events. Helicopter shopping refers to the practice of a requesting EMS agency or hospital calling numerous HEMS operators until one agrees to accept a flight without disclosure to the accepting HEMS operator that other programs have declined the flight because of bad weather or other safety concerns.31,32 The practice has been so common that in 2006, the Federal Aviation Administration issued a letter to all state EMS directors describing helicopter shopping and requesting that they take action to prohibit this practice.33
Landing Zones
Many hospitals have designated landing areas that are appropriately lit and secured (Fig. 191-2), with fixed coordinates and predesignated liftoff and approach patterns. However, most primary (scene) responses occur at unmarked sites. Ground personnel must be trained to designate and secure a safe landing zone for helicopter operations. AMT programs have an obligation to help train ground staff on proper landing zone setup and conduct (Boxes 191-1 and 191-2).

Figure 191-2 Landing zone safety is paramount to delivery of patients to hospitals. (Photograph courtesy Dan Lemkin, MD.)
Helicopter flights direct to the scene of an accident pose unique risks to AMT from hazards near the landing zone. This risk is heightened at night. In response to this concern, out-of-hospital care providers and flight programs have found it beneficial and safer to use a hospital helipad for rendezvous. This practice raised concerns about Emergency Medical Treatment and Active Labor Act (EMTALA) responsibilities to provide a medical screening examination for these patients. In May 2004, the Centers for Medicare and Medicaid Services resolved this issue, noting that the use of a helipad on hospital property does not trigger EMTALA provisions as long as the helipad is being used only as a stopping place for EMS personnel to rendezvous with AMT, facilitating transport of a patient to the closest appropriate facility.34
Clinical Concepts and Patient Care
Although virtually all types of patients have been transported by air medical services, available data do not allow prospective, definitive identification of which patients will benefit from flight. Many questions about the triage of patients to air or ground transport, the efficacy of air medical care, and the precise effects of AMT on morbidity and mortality in medical and surgical conditions remain unanswered. There are volumes of studies indicating what patients can be cared for in the air medical environment and what skills and equipment can be used, and there are also many studies demonstrating benefit to air transport. Unfortunately, there is a relative paucity of clinical investigation addressing potential solutions to the problems of triage and appropriate use. What does seem clear is that medical flight is generally associated with safe patient care and a low incidence of adverse effects.35 In an effort to ensure that AMT resources are used wisely, the Air Medical Physician Association (AMPA) has established a detailed medical condition list for the appropriate use of AMT.36 A more general approach to the need for AMT is illustrated in Box 191-3.
Trauma
Most trauma studies have addressed air medical use for scene response.37 Methodological heterogeneity precludes formal meta-analysis of the AMT outcomes data. However, existing data support an estimate of 20 to 35% improvement is survival rates, or the saving of three to six lives (fewer for pediatric patients) per 100 air medical trauma flights.38–46 As demonstrated by a large 2011 study assessing nearly 75,000 secondary HEMS transports, interfacility air transport of the more seriously injured patient (but not those with lesser severity) is also associated with improved outcomes.47 Two studies also found improved outcomes with seriously injured patients transported by HEMS while also concluding that stable patients may be transported from outlying hospital to definitive care by ground with equal effect.47,48 Noting that HEMS represents the only modality by which nearly 28% of U.S. residents have timely (within 1 hour) access to level I or level II trauma centers emphasizes the vital role of AMT in care of the injured patient.49 Studies have also presented data that suggest lack of HEMS benefit for the trauma victim, but these studies represent a minority of works and are limited by confounding factors such as inclusion of transports to nontrauma centers.50 Whereas caution should be exercised in definitive statements about the criteria for and the value of AMT, and such statements can be interpreted only in light of the overall local environment in which the transport system exists, the clear message from the literature is that HEMS functions best as a part of a comprehensive trauma system and not as an isolated entity.51–53
Work in HEMS casts doubt on the supposed logistical advantages of the helicopter itself.54 Faster times to trauma centers are not required for the accrual of better outcomes. It is true that in some studies, subgroup analyses suggest improved trauma outcomes due to HEMS scene response for the more severely injured.55 However, studies conducted in regions as disparate as California and The Netherlands demonstrate HEMS mortality benefit but find similar scene–to–trauma center times for ground and air transports.45,56 It seems clear that for many patients, factors other than speed (such as the provision of advanced levels of care over that provided by ground personnel) are responsible for AMT’s benefits.
In terms of specific populations of patients, some studies suggest that most trauma victims transported by air have non–life-threatening injuries.57 Fortunately, the best large-scale population analysis, of more than 40,000 HEMS transports from the 2007 American College of Surgeons National Trauma Data Bank, clearly demonstrates that HEMS-transported patients are indeed of much higher acuity than ground-transported patients.37 For example, the median Injury Severity Score of HEMS patients exceeded the commonly used “severe injury” cutoff of 15; HEMS patients also had a 43% rate of intensive care unit admission.37 If we look more specifically within the trauma population, we find that data from Pennsylvania and California of head injury patients undergoing out-of-hospital intubation demonstrate HEMS-associated improvements in both morbidity and mortality.58,59 A 2009 study from Italy confirmed the association between HEMS transport and improved head injury outcome as assessed by either mortality or functional endpoints.60
AMT is unlikely to improve outcome in those whose injuries are either trivial or grave. However, if the Injury Severity Score is collapsed into five ordinal categories, a significant association between helicopter transport and improved mortality is found in the middle three categories (survival odds ratios range from 2.1 to 2.6). Other work has also found that AMT shows benefit over ground transport only for those more seriously injured patients in both rural and urban environments.61,62 In all these cases, it remains uncertain if improvements in outcome are related to the provision of improved on-scene care or the integration of HEMS into a comprehensive trauma system as opposed to the air transport itself. Fortunately, even the acknowledged imprecision of triage to HEMS does not preclude “real-world” identification of AMT-associated trauma outcomes benefit. In a 2010 population-based study in Canada, patients were entered into the study if HEMS services were requested, and outcomes were compared between those who actually underwent AMT and those who went by ground because of the unavailability of HEMS. The study identified a benefit of HEMS, compared with ground transport, of 5.61 more lives saved per 100 transports.62
Cardiac Disorders
The ability to study HEMS-related outcomes benefit in acute coronary syndrome is limited by the lack of validated scores that can be used to stratify risk and to predict outcome. Works have noted that helicopter transport extends the geographic referral base of primary angioplasty centers and that outcomes of patients flown from a distance for definitive care equal outcomes of patients presenting primarily to the referral center.63 AMT systems have been shown to be able to safely transport complicated cardiovascular patients with conditions such as acute coronary syndrome, ST segment elevation myocardial infarction, and aortic aneurysm.64–67
Stroke
With the advent of time-critical therapy for ischemic stroke, HEMS has played an increasing role in the regionalization of acute neurologic care. Early studies demonstrating safety of transport of post-thrombolysis stroke patients have been complemented by case series illustrating the increasing use of helicopter interfacility transport for stroke.68,69 Case reports and series have demonstrated the utility of air medical dispatch for primary (scene) transport of patients with strong suspicion of stroke.70–72 In one region, ground EMS providers were able to identify stroke with accuracy, and helicopter-transported patients composed nearly 25% of the stroke center’s thrombolytic volume. The use of strict triage definitions kept inappropriate calls for AMT to acceptably low levels while allowing a significant extension of the geography served by an individual stroke center.71 Performance measurement programs can monitor the efficacy of the AMT service.72
Pregnancy
With appropriate triage, the speed of air transport of the high-risk pregnancy can counterbalance the risk of delivering an infant in an aircraft’s confined space.73,74 Case series demonstrate that high-risk obstetric patients transported by air from distant hospitals have outcomes as good as those of patients presenting primarily to an obstetric referral center.73,75 Common reasons for obstetric transport include preterm labor and premature rupture of membranes.76
Neonates and Children
The use of AMT to extend the geographic reach of neonatal care centers is reported from many settings.77,78 The most rigorous analysis suggests that long-distance AMT allows infants with medical complications born in remote areas to achieve outcomes equal to those of infants born in urban centers. Although neonates are vulnerable to physiologic deterioration, specialty team air transport is associated with no more derangement in oxygenation and ventilation than is transport by ground vehicle.77 As in the case of trauma, the question remains if the advantage of AMT is related to the use of air transport or specialty services brought to the patient’s side.
Many areas depend on AMT to deliver critically ill or injured children to regional pediatric centers. Although speed of transport may be an important consideration, as with neonates it seems the emphasis is often more on the transport team than on the mode of transport. Experienced pediatric transfer teams often bring a level of expertise unavailable to the pediatric patient in the outlying hospital and are noted to have fewer adverse events during transport than nonspecialty teams.79–81 Appropriate training, experience, and competency are essential for those responsible for transport.82 AMT has been shown to be safe for moving of even the most critical children requiring extracorporeal membrane oxygen support.83
Efficacy and Cost-Effectiveness
Cost-benefit is an area of increasing focus for AMT. The crux of the problem lies in the inability to precisely identify in a prospective manner which patients will truly benefit from fixed-wing or rotor-wing flight. As a result, in many cases there is little if any guidance regarding when air medical dispatch is indicated.84 With use of endorsed guidelines (such as those endorsed by the AMPA) for air medical dispatch, EMS regional authorities should collaborate to generate criteria best for their own systems, with constant refinement guided by rigorous use review.85 Despite this ideal, however, in practice the lack of firm indications and guidelines means that AMT often acts more as a “taxi service” responding to the needs of referring physicians, hospitals, and EMS services rather than the actual needs of the patient. There is a strong economic argument to be made for maintaining this “looseness” of service, as flight revenues keep AMT services available for those truly in need.
Compared with the cost-benefit ratios of other medical interventions, AMT is well within the accepted range per quality-adjusted life-year saved.86–88 One Scandinavian study concluded that the benefits of ambulance missions flown by helicopters exceed the costs by a factor of almost six.89 Another group from the region estimated that HEMS contributes to the cost-effectiveness of primary PCI, and other investigators have demonstrated the favorable cost-effectiveness of helicopter stroke transports.90,91 However, these results cannot be taken as definitive statements on a global basis, as any cost-benefit calculation is applicable only within the health care environment of the system under study.92
Cost-effectiveness determinations are not straightforward. It is difficult to calculate true cost-effectiveness for transports that are not likely to occur (as with high-risk obstetrics cases at risk of precipitous delivery)73 or that would deliver patients outside critical time windows (as for stroke or cardiac transports) in the absence of AMT.68,93 Cost-efficiency is also difficult to demonstrate when there are no comparison options (such as transport from coastal islands or locations without road access) or when integrated ground and air transport systems have already become established in ways that effectively prohibit head-to-head comparisons of risks and outcomes (as is true in most of the United States). If we accept that HEMS represents the only mechanism by which more than 80 million U.S. citizens have timely access to mortality-improving high-level trauma center care,49 it is obvious that some form of air transport is a “must-have” for some EMS regions, and calculations of cost-efficiency fall away in favor of service provision.
Although transport by air is nearly always more expensive than that by ground, the costs of air medical flight should be viewed in contrast with the “real-life” alternative mode of transport. In many cases, and especially where time and distance are significant factors, the total fiscal and opportunity costs of AMT are arguably less expensive than the alternative.94 Unfortunately, the work of assessing the cost-effectiveness of AMT is complicated by the extremely limited amount of information on the cost-effectiveness of ground-based modes of transport.95 Experts assessing existing literature have concluded that although the available data do not enable rigorous meta-analysis, most investigations do demonstrate that appropriately used HEMS is cost-effective.
Future of Air Medical Transport
This work has noted that the major challenge within the AMT community is to determine not whether but rather in whom there is benefit to air medical flight. Currently, the major dilemma facing helicopter transport outcomes researchers is the identification of triage variables that can prospectively (i.e., at the time of transport vehicle selection) guide use of the air medical resource.84,85,96 It also seems that over time, advances in ground-based EMS and the availability of critical care ground ambulances for interfacility transports are beginning to offset many of the assumed benefits of AMT. Nonetheless, the regionalization of specialty services, development of new therapies that are highly time sensitive, and inflexible geography mean that there will always be a role for AMT in emergency care.
References
1. Lindsay, MB. Trauma management: Issues for the air medical crew. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association; 2006:386–398.
2. Blumen, IJ, Callejas, S. Transport physiology. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association; 2006:357–377.
3. Wilson, GD, Sittig, SE, Schears, GJ. The laryngeal mask at altitude. J Emerg Med. 2008;34:171.
4. Rodriquez, D, Jr., et al. Effects of simulated altitude on ventilator performance. J Trauma. 2009;66:S172.
5. Miyashiro, RM, Yamamoto, LG. Endotracheal tube and laryngeal mask airway cuff pressures can exceed critical values during ascent to higher altitude. Pediatr Emerg Care. 2011;27:367–370.
6. Tollefsen, WW, et al. Endotracheal tube cuff pressures in pediatric patients intubated before aeromedical transport. Pediatr Emerg Care. 2010;26:361–363.
7. Bassi, M, Zuercher, M, Erne, JJ, Ummenhofer, W. Endotracheal tube intracuff pressure during helicopter transport. Ann Emerg Med. 2010;56:89–93.e1.
8. Blumen, IJ, HEMS Accident Analysis—The State of the Union. October 2011.
9. Data compiled from the Atlas and Database of Air Medical Services. Center for Transportation Injury Research in alliance with the Association of Air Medical Services and the air medical industry, with support from the Federal Highway Administration and the National Highway Traffic Safety Administration. www.adamsairmed.org.
10. Warren, J, Fromm, RE, Jr., Orr, RA, Rotello, LC, Horst, HM. Guidelines for the inter- and intrahospital transport of critically ill patients. Crit Care Med. 2004;32:256–262.
11. Commission on Accreditation of Medical Transport Systems, Accreditation Standards. 8th ed. Anderson, SC:Commission on Accreditation of Medical Transport Systems; 2010. www.camts.org/component/option,com_docman/task,cat_view/gid,17/Itemid,44/.
12. Stocking, JC. Crew configuration. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association; 2006:36–42.
13. Myers, KJ, Rodenberg, H, Woodard, D. Influence of the helicopter environment on patient care capabilities: Flight crew perceptions. Air Med J. 1995;14:21.
14. Blumen, IJ, Thomas, F, Williams, D. Transportation of the critically ill patient. In: Hall J, ed. Principles of Critical Care. 3rd ed. New York: McGraw-Hill; 2005:79–91.
15. Bott, S. Patient care capabilities and limitations. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association; 2006:30–35.
16. Driscoll, K, Saia, M, Thomas, S. Considerations in air medical transport of the critically ill patient. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association; 2006:399–405.
17. Eljaik, LF, Davidiff, JB, Stubba, W. Biomedical equipment and technology in critical care transport. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association; 2006:449–457.
18. Havel, C, et al. Quality of closed chest compressions in ambulance vehicles, flying helicopters, and at the scene. Resuscitation. 2007;73:264.
19. Thomas, F, et al. Does wearing a surgical facemask or N-95 respirator impair radio communication? Air Med J. 2011;30:97.
20. Braude, D, Goldsmith, WeissSJ. Assessing air medical crew real-time readiness to perform critical tasks. Prehosp Emerg Care. 2011;15:254.
21. Gregory, KB, Winn, W, Johnson, K, Rosekind, MR. Pilot fatigue survey: Exploring fatigue factors in air medical transport. Air Med J. 2010;29:309.
22. MacDonald, RD, Thomas, L, Rusk, FC, Marques, SD, McGuire, D. Occupational health and safety assessment of exposure to jet fuel combustion products in air medical transport. Prehosp Emerg Care. 2010;14:202.
23. Cushman, JT, Floccare, DJ. Flicker illness: An under-recognized but preventable complication of helicopter transport. Prehosp Emerg Care. 2007;11:85.
24. Wright, SW, et al. High fidelity medical simulation in the difficult environment of a helicopter: Feasibility, self-efficacy, and cost. BMC Med Educ. 2006;6:49.
25. Carrubba, C. Role of the medical director in air medical transport. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association; 2006:113–119.
26. Rinnert, KJ, Blumen, IJ, Gabram, SGA, Zanker, M. A descriptive analysis of air medical directors in the United States. Air Med J. 1999;18:6.
27. Medical direction and medical control of air medical services: Position statement of the Air Medical Physician Association. Revised April 13, 2002. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association; 2006:727–728.
28. Thomas, SH, Williams, KA, Claypool, D. Medical director for air medical transport programs: Position paper of the National Association of EMS Physicians. Prehosp Emerg Care. 2002;6:455.
29. Blumen, IJ, Lees, D. Air medical safety: Your first priority. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association; 2006:519–532.
30. Frakes, MA, Van Voorhis, S. Effectiveness of a challenge-and-respond checklist in ensuring safety behavior compliance by medical team members at a rotor-wing air medical program. Air Med J. 2007;26:248.
31. Alexander, RJ, Indiana Association of Air Medical Services. Helicopter shopping: What hospitals and first responders need to know. www.in.gov/dhs/files/helicopter_shopping.pdf.
32. Larrabee, C, International Association of Flight Paramedics. Position paper on helicopter shopping. www.flightparamedic.org/docs/HelicopterShopping.pdf.
33. Federal Aviation Administration. FAA letter to state EMS Director on helicopter shopping. http://data.memberclicks.com/site/nemsp/FAAStateLetter.pdf, August 2006.
34. Department of Health and Human Services, Centers for Medicare & Medicaid Services, Revised Emergency Medical Treatment and Labor Act (EMTALA) Interpretive Guidelines. Baltimore, Md:Department of Health and Human Services; May 13, 2004. www.cms.hhs.gov/SurveyCertificationGenInfo/downloads/SCLetter04-34.pdf.
35. Macdonald, RD, Banks, BA, Morrison, M. Epidemiology of adverse events in air medical trnapsort. Acad Emerg Med. 2008;15:923.
36. Air Medical Physician Association. Medical condition list and appropriate use of air medical transport: Position statement of the Air Medical Physician Association. Prehosp Emerg Care. 2002;6:464.
37. Brown, JB, et al. Helicopters and the civilian trauma system: National utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69:1030–1034.
38. Schiller, J, et al. Improvement of trauma-related mortality with implementation of helicopter transport [abstract]. J Trauma. 2006;61:1572.
39. Baxt, W, Moody, P, Cleveland, H. Hospital-based rotorcraft aeromedical emergency care services and trauma mortality: A multicenter study. Ann Emerg Med. 1985;14:859–864.
40. Oppe, S, DeCharro, F. The effect of medical care by a helicopter trauma team on the probability of survival and the quality of life of hospitalized victims. Accid Anal Prev. 2001;33:129–138.
41. Mitchell, AD, Tallon, JM, Sealy, B. Air versus ground transport of major trauma patients to a tertiary trauma center: A province-wide comparison using TRISS analysis. Can J Surg. 2007;50:129–133.
42. Thomas, S, et al. Helicopter transport and blunt trauma outcome. J Trauma. 2002;52:136–145.
43. McVey, J, Petrie, D, Tallon, J. Air versus ground transport of the trauma patient: A natural experiment [abstract]. Prehosp Emerg Care. 2007;11:128.
44. Davis, D, et al. The impact of aeromedical response to patients with moderate to severe traumatic brain injury. Ann Emerg Med. 2005;46:115–122.
45. Frankema, S, et al. Beneficial effect of helicopter emergency medical services on survival of severely injured patients. Br J Surg. 2004;91:1520–1526.
46. Ringburg, AN, et al. Lives saved by helicopter emergency medical services: An overview of literature. Air Med J. 2009;28:298–302.
47. Brown, JB, et al. Helicopters improve survival in seriously injured patients requiring interfacility transport for definitive care. J Trauma. 2011;70:310.
48. Svenson, JE, O’Connor, JE, Lindsay, MB. Is air transport faster? A comparison of air versus ground transport times for interfacility transfers in a regional referral system. Air Med J. 2006;25:170.
49. Branas, CC, et al. Access to trauma centers in the United States. JAMA. 2005;293:2626.
50. Chappell, VL, Mileski, WJ, Wolf, SE, Gore, DC. Impact of discontinuing a hospital-based air ambulance service on trauma patient outcomes. J Trauma. 2002;52:486–491.
51. Stewart, KE, Cowan, LD, Thompson, DM, Sacra, JC. Factors at the scene of injury associated with air versus ground transport to definitive care in a state with a large rural population. Prehosp Emerg Care. 2011;15:193.
52. Karanicolas, PJ, et al. The fastest route between two points is not always a straight line: An analysis of air and land transfer of non-penetrating trauma patients. J Trauma. 2006;61:396.
53. Butler, DP, Anwar, I, Willet, K. Is it the H or the EMS in HEMS that has had an impact on trauma patient mortality? A systematic review of the evidence. Emerg Med J. 2010;27:692.
54. Ringburg, AN, et al. Helicopter emergency medical services (HEMS): Impact on on-scene times. J Trauma. 2007;63:258–262.
55. Talving, P, et al. Helicopter evacuation of trauma victims in Los Angeles: Does it improve survival? World J Surg. 2009;33:2469–2476.
56. Davis, DP, et al. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J Trauma. 2005;58:933.
57. Bledsoe, BE, Wesley, AK, Eckstein, M, Dunn, TM, O’Keefe, MF. Helicopter scene transport of trauma patients with non life-threatening injuries: A meta-analysis. J Trauma. 2006;60:1257.
58. Wang, H, et al. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;44:439.
59. Davis, D, Stern, J, Ochs, M. A follow-up analysis of factors associated with head-injury mortality after paramedic rapid sequence intubation. J Trauma. 2005;59:486.
60. Berlot, G, et al. Influence of prehospital treatment on the outcome of patients with severe blunt traumatic brain injury: A single-centre study. Eur J Emerg Med. 2009;16:312–317.
61. Talving, P, et al. Helicopter evacuation of trauma victims in Los Angeles: Does it improve survival? World J Surg. 2009;33:2469.
62. McVey, J, Petrie, DA, Tallon, JM. Air versus ground transport of the major trauma patient: A natural experiment. Prehosp Emerg Care. 2010;14:45.
63. Grines, C, Westerhausen, D, Grines, L. A randomized trial of transfer for primary angioplasty versus on-site thrombolysis in patients with high-risk myocardial infarction (Air PAMI trial). J Am Coll Cardiol. 2002;39:1713.
64. Youngquist, ST, McIntosh, SE, Swanson, ER, Barton, ED. Air ambulance transport times and advanced cardiac life support interventions during the interfacility transfer of patients with acute ST-segment elevation myocardial infarction. Prehosp Emerg Care. 2010;14:292.
65. Trojanowski, J, Macdonald, RD. Safe transport of patients with acute coronary syndromes or cardiogenic shock by skilled air medical crews. Prehosp Emerg Care. 2011;15:240.
66. Shewakramani, S, Thomas, SH, Harrison, TH, Gates, JD. Air transport of patients with unstable aortic aneurysms directly into operating rooms. Prehosp Emerg Care. 2007;11:337.
67. Stewart, AM, McNay, R, Thomas, R, Mitchell, AR. Early aeromedical transfer after acute coronary syndromes. Emerg Med J. 2011;28:325.
68. Thomas, SH, et al. The evolving role of helicopter emergency medical services in the transfer of stroke patients to specialized centers. Prehosp Emerg Care. 2002;6:210.
69. Konstantopoulos, WM, et al. Helicopter emergency medical services and stroke care regionalization: Measuring performance in a maturing system. Am J Emerg Med. 2007;25:158.
70. Thomas, SH, Schwamm, LH, Lev, MH. Case records of the Massachusetts General Hospital. Case 16-2006. A 72-year-old woman admitted to the emergency department because of a sudden change in mental status. N Engl J Med. 2006;354:2263.
71. Silliman, S, et al. Use of a field-to-stroke-center helicopter transport program to extend thrombolytic therapy to rural residents. Stroke. 2003;34:729.
72. Konstantopoulos, WM, et al. Helicopter emergency medical services and stroke care regionalization: Measuring performance in a maturing system. Am J Emerg Med. 2007;25:158.
73. Elliott, J, O’Keeffe, D, Freeman, R. Helicopter transportation of patients with obstetric emergencies in an urban area. Am J Obstet Gynecol. 1982;143:157.
74. Ohara, M, et al. Safety and usefulness of emergency maternal transport using helicopter. J Obstet Gynaecol Res. 2008;34:189.
75. van Hook, J, Leicht, T, van Hook, C. Aeromedical transfer of preterm labor patients. Tex Med. 1998;94:88.
76. Jony, L, Baskett, TF. Emergency air transport of obstetric patients. J Obstet Gynaecol Can. 2007;29:406.
77. Hon, K, Olsen, H, Totapally, B, Leung, TF. Air versus ground transportation of artificially ventilated neonates: Comparative differences in selected cardiopulmonary parameters. Pediatr Emerg Care. 2006;22:107.
78. Berge, S, Berg-Utby, C, Skogvoll, E. Helicopter transport of sick neonates: A 14-year population-based study. Acta Anaesthesiol Scand. 2005;49:999–1003.
79. Hanson, JH, Orr, RA. The air medical transfer process of the critically ill or injured pediatric patient. In: Blumen IJ, ed. Principles and Direction in Air Medical Transport. Salt Lake City, Utah: Air Medical Physician Association, 2006.
80. Coppola, CP, Tyree, M, Larry, K, De Geronimo, R. A 22-year experience in global transport extracorporeal membrane oxygenation. J Pediatr Surg. 2008;43:46.
81. Orr, RA, et al. Pediatric specialty care teams are associated with improved outcomes. Pediatrics. 2009;124:40–48.
82. American Academy of Pediatrics, Section on Transport Medicine. Guidelines for Air and Ground Transportation of Neonatal and Pediatric Patients, 3rd ed. Elk Grove Village, Ill: American Academy of Pediatrics; 2007.
83. Cabrera, AG, et al. Interhospital transport of children requiring extracorporeal membrane oxygenation support for cardiac dysfunction. Congenit Heart Dis. 2011;6:202–208.
84. Shatney, C, Homan, J, Sherck, J, Ho, CC. The utility of helicopter transport of trauma patients from the injury scene in an urban trauma system. J Trauma. 2002;53:817–822.
85. Thomson, D, Thomas, S. Guidelines for air medical dispatch: Position statement for National Association of EMS Physicians. Prehosp Emerg Care. 2003;7:265.
86. Kurola, J, et al. Paramedic helicopter emergency service in rural Finland—do benefits justify the cost? Acta Anaesthesiol Scand. 2002;46:771.
87. Wood, AJ. When increased therapeutic benefit comes at increased cost. N Engl J Med. 2002;346:1819.
88. Nicholl, J, et al. A Review of the Costs and Benefits of Helicopter Emergency Ambulance Services in England and Wales: Report to the Department of Health. London: Department of Health; 2003.
89. Elvik, R. Cost-benefit analysis of ambulance and rescue helicopters in Norway: Reflections on assigning a monetary value to saving a human life. Appl Health Econ Health Policy. 2002;1:55.
90. Selmer, R, et al. Cost-effectiveness of primary percutaneous coronary intervention versus thrombolytic therapy for acute myocardial infarction. Scand Cardiovasc J. 2005;39:276.
91. Silbergleit, R, et al. Cost-effectiveness of helicopter transport of stroke patients for thrombolysis. Acad Emerg Med. 2003;10:966.
92. Taylor, CB, et al. A systemic review of the costs and benefits of helicopter emergency medical services. Injury. 2010;41:10.
93. Thomas, S, et al. Prehospital EKG and early helicopter dispatch to expedite interfacility transfer for percutaneous coronary intervention. Crit Pathways Cardiol. 2006;5:155.
94. Hankins, DG. Air medical transport of trauma patients. Prehosp Emerg Care. 2006;10:324–327.
95. Lerner, EB, et al. Economic value of out-of-hospital emergency care: A structured literature review. Ann Emerg Med. 2006;47:515.
96. Thomas, SH, Biddinger, PD. Helicopter trauma transport: An overview of recent outcomes and triage literature. Curr Opin Anesth. 2003;16:153–158.