Aging, dementia, and disorders of cognition
OSA JACKSON SCHULTE, PT, PhD, GCFP/AT, JAMES STEPHENS, PT, PhD, CFP and JOYCE ANN, OTR/L, GCFP
After reading this chapter the student or therapist will be able to:
1. Define the basic terminology and discuss the prevalence of cognitive disturbances seen in older persons.
2. Describe normative changes in brain function with normal aging and their relevance to the diagnoses of delirium and dementias.
3. Discuss how symptoms are altered with normal aging (specifically related to the Arndt-Schultz principle, law of initial values, and habitual biorhythms) for an individual.
4. Describe normal sensory changes with aging and how they alter a person’s overall ability to adapt to stress.
5. Describe how, and for what type of patient, to use the Mini-Mental State Examination as a part of the physical or occupational therapy examination.
6. Describe common sensory changes with dementia and implications for adapting physical or occupational therapy evaluation and intervention.
7. Discuss common changes in learning styles with aging and implications for adapting physical or occupational therapy intervention to enhance patients’ ability to perform at their highest functional level.
8. Describe how environmental design and ergonomics can enhance patient performance in activities of daily living and instrumental activities of daily living.
9. Describe a strategy to evaluate a patient’s emotional capacity to participate in a learning task and its clinical relevance to both occupational and physical therapy outcomes.
10. Describe criteria for delirium and reversible dementia and sample strategies for modifying evaluation and treatment procedures.
11. Discuss symptoms and disease progression in irreversible dementia.
12. Discuss the therapist’s role on the treatment team in educating key caregivers and support personnel and sample training strategies.
13. Discuss treatment skills that are helpful in working with persons who have irreversible dementia.
14. Describe research activities and new findings that affect physical evaluation and treatment of the patient with dementia or delirium.
The starting point with older persons in physical or occupational therapy
1. Evaluate, document, and make available to the hands-on caregivers what the patient “likes”—his or her preferences and habits for all activities of daily living (ADLs) and instrumental activities of daily living (IADLs).
2. Train caregivers to create a care plan for daily living and nursing that builds in the patients’ preferences to support his or her personal identity and self-image.
3. Create specific physical therapy or occupational therapy functional goals that build on and reinforce patient preferences with regard to mobility, eating, bathing, grooming, dressing, socialization, and so on. (Note: If caregivers change, training needs to be added and new goals may need to be developed because not all caregivers have the same capacity to relate to the patient.)
4. Train caregivers with the older person to use specific neurofacilitation strategies to: (a) enhance breathing, (b) increase bed mobility, (c) improve balance in sitting and standing, (d) perform active range of motion (AROM) and active assisted range of motion (AAROM) for ADLs and IADLs, (e) achieve skeletal weight shift for ADLs and IADLs, (f) encourage head, neck, and spine to upright postural response during ADLs and IADLs, and (g) encourage walking and stair climbing safely and as able.
5. Screen for signs of reversible cognitive losses.
6. Provide adaptations and training for performance of ADLs when chronic cognitive problems exist.
7. Train caregivers and the older person in ways to adapt the ADLs and IADLs to maximize ability.
Paradigm for aging, the brain, and learning
Life involves ongoing learning. The brain and human nervous system have at least 3 × 1010 parts. As Feldenkrais stated, “This is large enough for its balanced functions to obey the law of large systems. The health of such a system can be measured by the shock (stimuli) it can take without compromising the continuation of its processes.”1 Adaptability and health can be measured by the number of stimuli or amount of shock people can tolerate without their usual way of life being compromised. Aging is a process that requires ongoing adaptation to and compensation for the losses that are imposed on human beings from the outside world and the internal physiological changes that occur with the passage of time, physical activities, emotional state, fatigue, digestive and elimination processes, and habitual rest-activity cycle. If a person’s health is altered by illness or trauma, then he or she goes through an adaptive process. If too many changes happen too quickly, the brain is not able to create a functional adaptive response, and the individual must alter or simplify her or his life processes or face negative mental or physiological reactions. The literature demonstrates that regression periods and illness seem to be linked.2–5 As human beings explore coping with unfamiliar experiences, they require more nurturing, rest, and physical contact that is perceived as empowering.
Human beings progress to adulthood through the millions of perceptions and choices that are recorded and responded to through the developmental years. Human beings are not born with the brain and nervous system having the skills of an adult. In infancy the brain begins to learn during interactions with the environment. The kinesthetic and sensory connections provide data about the internal and external environments. Through this interactive learning process each human being (with a nondifferentiated nervous system) discovers new differentiations and thus new strategies for relating to the world. With advancing age there is a gradual decrease in the acuity of the kinesthetic and sensory information received. These changes can affect interactive learning for the older adult.6–8 Active participation has a positive impact on recall and learning,9 predictable events support recall,10 and ordered events are easier to recall. Differentiation for human beings does not happen uniformly.11,12 As a person grows, the result of this lack of uniformity is that some adults prefer to relate to the world visually, others aurally, and still others by touch or kinesthetically. In other words, people specialize with their sensory processing and at the same time become more vulnerable to issues of sensory adaptation and selection.13
What if rehabilitation after illness or trauma invited a guided examination of self-awareness and habitual strategies as the basis for inventing new functional adaptive strategies? The Feldenkrais Method is one model for neurological facilitation and enhancement of human learning and adaptability that is built on the concept of starting from the current habits of action of the person.1,14,15 The Feldenkrais Method also uses several other basic learning strategies that make this approach helpful for the older patient: going slowly, simplifying the movement or stimuli, proceeding from the perception of the patient, learning to detect and respond to the smallest possible input, and increasing the awareness and use of the skeleton and the support it gives. Feldenkrais noted what a person automatically did during a crisis, such as a fall. He noted the automatic human response and then built in a self-defense response that took advantage of the innate reflex.16 The result is that exploratory learning is easy for the patient because it builds on the automatic response with which the person is already familiar. The goal is to invent physical therapy interventions that encourage patient participation and that feel safe and useful to the patient.
In this chapter the paradigm for aging and lifelong learning presumes the following:
1. The brain and central nervous system are viewed as the master system and the controller of the other human systems (e.g., digestive, cardiovascular, muscular, hormonal).
2. Capacity exists for ongoing learning (self-awareness), self-regulation, and adaptability through the life span.
3. The whole (human being) is greater than the sum of its parts.
4. Language shapes reality and the experience and perceptions of life.
5. Enjoying a comfortable and easy pace for new learning is beneficial. Being able to learn new skills is important for adaptability and for lifelong well-being.
6. The mind and body are not separate.
7. Personal variations in learning style and preferences for relating can be used to maximize adaptation throughout life.
8. The activation of the limbic system for “fight or flight” is normal, and the ability to release the limbic activation and find the resting state when the crisis (real or imagined) is over becomes a critical skill for adapting as people grow older.17
9. Creation of environments that encourage safe exploration of new ideas and ways of self-expression can generate lifelong human growth and development.
Framework for clinical problem solving
Therapists working with patients with cognitive impairments need to have received adequate advanced training in assessment of communication skills and neurological functioning as well as gerontology so they can work with maximal efficacy and enjoy the clinical interactions with each patient. In 37 bc the Roman poet Virgil wrote, “Age carries all things, even the mind, away.”18 Nearly 400 years ago, Shakespeare described the last stage of human life as “second childishness and mere oblivion, sans teeth, sans eyes, sans taste, sans everything.”19 This pessimistic view of the fate of the elderly persists among health care workers today despite the fact that significant cognitive deficits affect only 6.1% to 12.3% of the elderly (people older than age 65 years) in the United States.20,21
The clinician should not assume that an older person has impaired cognitive functioning. Perhaps the most crucial concept for clinical problem solving is that the clinician must not assume that the current abilities reflect the true capacity of the person. When a patient is observed to have altered brain function, description of the extent and type of the distortion of intellectual capacity and determination of the time of onset (sudden or gradual) are necessary to enable a diagnosis and the provision of appropriate and effective treatment and care. The capacity to learn is a possibility, although the process of learning may be altered or different from that of unaffected older adults.22–25 When age, illness, or medications create a temporary or permanent change in cognitive abilities, all functional training requires alteration to meet the unique cognitive abilities of the patient at the moment. For example, the son of a patient who needed physical and occupational therapy showed staff how to communicate with his mother so she did not get scared. The therapist walked slowly into the room and greeted the patient by touching her softly on the cheek with the back of her hand. The patient looked up and smiled. The therapist smiled back and stroked the patient softly on the top of her head. The patient smiled again. The therapist kneeled down so that she was eye to eye with the patient sitting in the wheelchair. She took the patient’s hand in her own hand and with her other hand slowly stroked the back of the patient’s hand. The patient smiled again. The therapy session had begun. For this patient, words were actually confusing so they were avoided.26 The need for tactile nurturing input stays and persists as people age.27 Nurturing tactile input done at a pace that is pleasant for the patient can actually support a positive clinical outcome.28
Definition of terms
1. Mental retardation: A person with mental retardation (also called developmental disability) has had some degree of intellectual impairment all her or his life. A person with mental retardation also can develop delirium or dementia. Delirium or dementia differs from mental retardation in that a change from the baseline level of functioning has occurred in that person.
2. Delirium: A person with delirium usually shows a change both in intellectual function and in level of consciousness.29,30 The patient may be perplexed, disoriented, fearful, forgetful, or all of these. The patient is often less alert than normal and may be sleepy or obtunded; however, many patients with delirium are hypervigilant and may be extremely agitated and suspicious. Delirium frequently occurs in the presence of a concurrent dementia. Early identification of the symptoms and formal medical assessment and treatment are critical to ensure the return of a normal level of alertness and intellectual function and to prevent the development of secondary functional impairments and possible dementia.31
3. Dementia: Dementia is the impairment of some or all aspects of intellectual functioning in a person who is fully alert. Some diseases that can cause dementia are treatable, and if treated early and aggressively, the patient’s deterioration of intellectual function may be either reversed or halted. Dementia usually involves cognitive impairment affecting memory and orientation and at least one of the following32,33:
 Abstract thinking. This is a common loss and involves an altered ability to relate to anything other than tangible reality. In dementia or Alzheimer disease (AD), this skill is predictably missing in most cases. This is exacerbated by fear and anxiety.
Abstract thinking. This is a common loss and involves an altered ability to relate to anything other than tangible reality. In dementia or Alzheimer disease (AD), this skill is predictably missing in most cases. This is exacerbated by fear and anxiety.
 Judgment and problem solving. This capacity decreases in the first stage of AD and is missing by the second stage.34–36
Judgment and problem solving. This capacity decreases in the first stage of AD and is missing by the second stage.34–36
 Language. Use of language for communication becomes altered in the second stage of AD, and by the third stage little verbal or no verbal communication is possible.37
Language. Use of language for communication becomes altered in the second stage of AD, and by the third stage little verbal or no verbal communication is possible.37
 Personality. A complex of all the attributes—behavioral, temperamental, emotional, and mental—that characterize a unique individual. A person makes choices that, whether remembered or not, make up his or her personality. Human beings live through these choices, which become filters for all future life experiences, and they believe that they are the truth. Caregivers and therapists must be aware of how the world is perceived by the patient. The staff must respect patients and their beliefs and work to minimize confrontation and agitation despite a person’s beliefs, prejudices, and biases.
Personality. A complex of all the attributes—behavioral, temperamental, emotional, and mental—that characterize a unique individual. A person makes choices that, whether remembered or not, make up his or her personality. Human beings live through these choices, which become filters for all future life experiences, and they believe that they are the truth. Caregivers and therapists must be aware of how the world is perceived by the patient. The staff must respect patients and their beliefs and work to minimize confrontation and agitation despite a person’s beliefs, prejudices, and biases.
4. Alzheimer disease: This is not synonymous with dementia but rather is one of the many causes of dementia. The term should be used only as a diagnosis when a complete clinical evaluation has been performed, a diagnosis of dementia has been made, and all other possible causes of the dementia have been ruled out. Definitive diagnosis of this disease is not possible until an autopsy or brain biopsy has been performed. Although multiple putative causes of the disease have been proposed, the cause and pathogenesis are unknown. No curative treatment for AD is currently available. Some drugs appear to slow the process of cognitive deterioration in some patients, and patients and their families can be helped through rehabilitation to cope better with the vicissitudes of the disease (see Chapters 6 and 36).
Epidemiology
Currently 5.3 million Americans are estimated to have AD. One in eight people over the age of 65 has AD.33 Researchers estimate that by 2050 13.2 million Americans will have AD if current trends continue and no cures are found.38 Half the people aged 85 years and older will have some form of dementia (9.5 million in 2050).39 Disorders causing cognitive deficits are expected to continue to be a growing public health problem for at least the next 50 years. The projected statistics, assuming no cures or effective means of preventing the common causes of dementia are discovered, are that by 2040 five times more individuals with dementia will be in society as today (7.4 million Americans). This increase is partially the result of the increased life expectancy of Americans.40 The most rapid population growth in this country is in the oldest age group, hence the increase in the prevalence of severe dementia. The prevalence of dementia rises from approximately 3% at ages 65 to 74 years to 18.7% at ages 75 to 84 years and to 47% of those older than 85 years.39 The increasing number of persons older than age 85 years will be paralleled by an increase in the incidence of dementia.
More than 70 conditions are known to cause dementia.33 Secondary behavioral problems in the patient with dementia can be interpreted as a response to somatic, psychological, or existential stress. Because memory impairments, impairments of abstract thinking or judgment, or global cognitive impairments in an elderly person may be symptoms of acute physical illness, the patient’s physical, emotional, social, and cognitive status and physical, social, and caregiver environment need to be systematically evaluated.33
Physiology of aging: relevance for symptomatology and diagnosis of delirium and dementias
The normal brain
The brain of a normal person at age 80 years shows several significant anatomical, physiological, and neurochemical changes when compared with the brain of a younger person. Brain weight decreases with advancing age.41 For example, the mean brain weight for women aged 21 to 40 years is 1260 g, whereas for women older than 80 years it is 1061 g.42 Dickstein and colleagues43 and Cabeza and colleagues44 have noted that although the brain loses thousands of cells daily, the areas of the brain involved in language, memory, and cognition are relatively spared from significant loss of neurons. Normal age-related changes vary from person to person in degree and severity and can include the following:
 Disturbance in ability to register, retain, and recall certain recent experiences
Disturbance in ability to register, retain, and recall certain recent experiences
 Slowed rate of learning new material24
Slowed rate of learning new material24
A motivated, upbeat elderly person who is not undergoing emotional stress will show few negative changes in intellectual capacity and may actually demonstrate an increase in intellectual functioning over time.19,53–55
A slowing of the natural pace of movement is commonly noted in people older than 80 years. This slowdown is manifested in the brain as a slowing of resting electroencephalogram (EEG) rhythms. At age 60 years, the mean frequency of the occipital rhythm is 10.3 Hz; at age 80 years, the mean frequency is 8.7 Hz. The average change in EEG frequency is approximately 1 cps per decade during these years.56 The speed of nerve conduction in the elderly can be 10% to 15% slower than in younger persons.57–59 Because of these physiological changes, if the process and structure of evaluation and care of the healthy older person emphasize speed of execution or timed activities, older adults will appear less capable than they really are. The therapist may need more time when working with persons older than 70 years than is generally required with the younger adult.
 A constant supply of nutrients, neurotransmitters, and other neurochemicals from a personally suitable diet
A constant supply of nutrients, neurotransmitters, and other neurochemicals from a personally suitable diet
 An unfailing supply of oxygen (implying appropriate blood count, collateral circulation, normal respiratory exchange and ruling out sleep apnea)
An unfailing supply of oxygen (implying appropriate blood count, collateral circulation, normal respiratory exchange and ruling out sleep apnea)
 Fluid, rhythmic breathing that adapts to needed changes in posture and exertion of the activity
Fluid, rhythmic breathing that adapts to needed changes in posture and exertion of the activity
 Normal blood biochemistry, especially fluid and electrolytes; adequate fluid intake is critical, and dehydration can contribute to altered brain function
Normal blood biochemistry, especially fluid and electrolytes; adequate fluid intake is critical, and dehydration can contribute to altered brain function
 Normal hepatic and renal function
Normal hepatic and renal function
 Freedom from noxious stimuli such as trauma, infection (including periodontal and gum disease), or toxins (including medications)
Freedom from noxious stimuli such as trauma, infection (including periodontal and gum disease), or toxins (including medications)
 Optimal levels of sensory stimulation and emotional stimulation balance
Optimal levels of sensory stimulation and emotional stimulation balance
The brain is the most physiologically active organ in the body. The brain represents only 2% of the total body weight, yet it consumes up to 20% of the oxygen and 65% of the glucose available in the circulation in the entire body.18 The minimal cardiovascular output required to deliver this is 0.75 L/min, which is equal to 20% of the total circulation (also dependent on body size). Because of the high level of nutrient use by the brain, it is one of the organs of the body most likely to be affected by any acute change in homeostasis. The homeostasis of the elderly brain is more vulnerable to disruption because of the normal age-related changes already discussed, as well as the increased permeability of the blood-brain barrier and increased sensitivity of neurons to the effects of outside agents such as drugs,60 junk food, allergies, and food sensitivities.
Arndt-schultz principle
The Arndt-Schultz principle summarizes the differences between the abilities of the younger brain and the aged brain to discriminate or respond to stimuli61:
1. The elderly require a higher level or a longer period of stimulation before the threshold for initial physiological response is reached. A related safety issue is that heat takes longer to be perceived, so the elderly are more likely to get a severe burn.
2. The physiological response in the aged is rarely as large, as visible, or as consistent as noted in younger people. In response to a heat pack, for example, the elderly skin may not turn bright red in response—the skin may turn white instead. When fever is present, they may not feel warm to the touch but instead may be very tired or clumsy.
3. The only similarity between the responses of the young and the elderly to stimuli is that once the threshold has been reached, then more stimuli result in an increase in response.
4. On average, the range of safe therapeutic stimulation is narrower for the elderly than for the young.
Law of initial values
The law of initial values is both a physiological and a psychological principle stating that with a given intensity of stimulation, the degree of change produced tends to be greater when the initial value of that variable is low at the onset of stimulation. In other words, the higher the initial level of functioning, the smaller the change that can be produced.62,63 The law of initial values, when defined and applied to younger persons, presumes that homeostasis is a stable and consistent process. When the law is used to describe physiological and psychological responses in older persons, it cannot be presumed that homeostasis for any variable is predictable or consistent from one person to the next, or even within a 24-hour period for the same individual. For example, an older person with mild dementia may eat only sweets if left without companionship at a meal. As a result, after the meal the individual may feel unsteady and afraid to walk back to the room. (Clinical consideration—Check blood sugar for all diabetics on evaluation before exertion.) In the young, defining the average times of peak activity for most physiological processes as well as for intellectual capacity is possible. In the clinical assessment of the older persons, defining the peak times of day for awareness and intellectual capacity for each individual is necessary. For example, some patients are best able to participate in learning a new skill in the early morning, and some only in the late afternoon.
Biorhythms
The brain has a biological clock that controls all physiological functions in a precise temporal course, whether daily (e.g., secretion of some hormones), monthly (e.g., menstruation), or during a certain period of the life cycle (e.g., ability to become pregnant).2,64,65 Before evaluating a geriatric patient with dementia or disturbance of intellectual functioning, assessment of the patient’s premorbid biorhythm is helpful. What was her or his daily schedule of activities before the medical crisis? The assessment or time study can map such things as rest periods, activities and level of exertion, sleep or rest periods, mental stimulation, emotional stimulation, eating, and elimination cycles across a 24-hour period. The patient assessment must allow for and assess the current and past variability of individual biorhythms. These biorhythms should be clearly documented and their stability evaluated and maintained as much as possible (critical if the patient will be going back to the family). For example, if a woman has worked for 40 years as a night nurse, being primarily active from 11 pm to 7 am, she will most likely be alert and best able to participate in a rehabilitation program during those hours. In most cases the patient should be allowed to choose the best time for treatment. For patients whose dementia is too severe for them to make this determination, the staff, by monitoring the patient’s behavior, can choose a time for treatment when the person is most alert. For the elderly, and particularly for those who have dementia, the time of assessment and treatment must be documented to maximize the person’s rehabilitation potential.66,67
Sensory changes with aging
Aging can also be defined in terms of adaptation. Aging is the progressive and usually irreversible diminution, with the passage of time, of the ability of a person or body part to perform efficiently or adapt to changes in the environment. The consequence of the process is manifested as decreased capacity for function and for withstanding stresses.68 Because the rehabilitation evaluation identifies functional problems, therapists should examine the possibility that sensory losses or disturbances (e.g., vision, hearing, touch, taste, smell, proprioception, temperature, and kinesthesia) are contributing to the functional impairments.61 A partial or total loss of one or more of the normal sensory inputs can result in disturbance of an individual’s mental status.
The more sudden the loss of a sense, the more difficult is the adaptation to the sensory disability. This is especially true for elderly persons because several mild sensory changes related to normal aging are already taxing their capacity to adapt. Adaptation to a sensory loss in one modality is typically accomplished through increased use of the other senses. For example, a young blind patient can adapt by using hearing and kinesthesia and usually learns to function well in spite of the loss of visual input. The older the patient is when blinded, however, the more difficulty she or he will have in making this adaptive crossover to other senses. At some time in any person’s life, adaptive crossover from one sense to another becomes exceedingly difficult, if not impossible. Thus psychopathological or behavioral changes may occur if a sensory impairment develops.69 This situation becomes more likely if the disruption is caused by a central nervous system deficit with multiple and abrupt simultaneous sensory input loss, such as might occur from a stroke.
The poliomyelitis epidemics of the early 1950s demonstrated the relationship between sensory input and abnormal behavior. Patients with poliomyelitis who were placed in tank-type respirators developed intermittent disruptions in mental state, including hallucinations, delusions, and dreamlike experiences while awake. The patients were deprived of normative input to the senses (kinesthesia and proprioception) and had severely restricted vision and hearing because of the nature of the construction of and the noise that emanated from the respirator. Solomon and Shackson70 and Solomon71 called this problem “sensory deprivation psychosis,” but this clinical situation may include cognitive changes in addition to psychotic symptoms. This type of problem often occurs today after a hip fracture when, to control the pain, a patient is given a medication that has the side effect of disrupting orientation to time and place. Until other medication can be tried to control the pain, the patient is described as “out of his or her mind,” especially at night. The patient may try to remove all clothing or call out to people for help, often a mother or father. The psychosis stops when the medication is removed. Recovery is also enhanced when consistent nurturing is provided. Note: Other common triggers can be the requirement to stay in one position (e.g., sleep on the back after surgery) or the need to have a spacer between the knees after surgery.
Sensory changes associated with normal aging can lead to the same degree of loss or distortion of significant sensory input as previously described.72–74 A bilateral loss of vision may lead to agitation and disorientation. Elderly people with hearing impairments often have grave difficulty relating to the world. Elderly persons who become deaf commonly experience some episodes of paranoid behavior.69 The problems for hearing-impaired elderly persons are often exacerbated by health care professionals who do not know how to place a hearing aid in a patient’s ear, replace a battery, adjust the volume on the aid, remove excess ear wax from the aid, identify the need to trim ear hair, or consider the possibility of a malfunctioning aid. Finally, sensory impairments may become exacerbated by surgical or medical interventions.
Certain medications, as well as some diseases, can also distort kinesthesia or retard the activity and movement of the patient.60 Movement is significant in the maintenance of an efficient nervous system. Anything that denies a person the ability to perform physical movement (e.g., drugs, restraints, traction, passive motion machine, positional props, or architectural designs not adapted to the elderly) hastens and increases the difficulty of adapting to functional limitations. The patient loses her or his freedom to move and may feel trapped and helpless. This can trigger memories of other trauma or violent experiences that involved feeling helpless or victimized. Movement is necessary for accurate sensation.14,75 It has been demonstrated that if movement of the eyes does not occur properly, vision becomes ineffective. The same is true to a lesser degree for hearing. If movement does not occur in the course of the hearing process, hearing can become distorted and misrepresented at the central level.
1. Evaluate the capacity to demonstrate the visual search response. This eye response is a tool to verify that the patient is relaxed and ready for new learning. A clinical example would be to have the person rest supine (with props for comfort as needed under the head, wrists, knees, ankles) and then begin a very slow passive rolling of the head 1 to 4 degrees per second to one direction and observe the eye response. The eyes of a relaxed person will naturally follow objects in the visual field in a functional tracking response as the head is rolled. The skill of visual search is altered (i.e., eyes dart around in a rapid visual search process or rest passively and do not move actively in the direction of the rolling of the head) when limbic activation or actual brain damage is present (90% discrimination).13,76,77 When the visual search is compromised, the Feldenkrais Method or other neurofacilitation techniques can be used to normalize the resting pattern of the neck and chest and invite the enhanced functional response for eye-head righting. Therapeutic exercise and neurofacilitation to encourage eye participation and other eye-body coordination training strategies have resulted in good functional improvements for persons with AD.78
2. Evaluate the capacity to use symbols. Assess the capacity to use signage in the building; does the patient comprehend and demonstrate comprehension by performance? For example, when an arrow points left, does the patient turn left?
3. Evaluate the capacity to perform complex motor skills (e.g., consistent step-by-step sequence). Even if the skill is not mastered, does the patient show improvement in the speed of a repetition task or increased emotional ease and willingness to participate even if verbal or physical cuing is still needed? Even if the patient cannot perform one motor skill, she or he may still show normal capacity to learn another motor skill.
4. If anxiety is present, try to alleviate it because anxiety interferes with integration of sensory learning (e.g., try a hot pack to the belly area for 5 to 10 minutes to promote relaxation).
Cognitive changes in normal aging
The idea that cognitive decline is a necessary part of aging is a myth. This belief has been debunked by research on crystallized and fluid intelligence.79,80 Crystallized and fluid intelligence are components of general intelligence. Crystallized intelligence involves the ability to perceive relationships, engage in formal reasoning, and understand intellectual and cultural heritage. Crystallized intelligence can be affected by the environment and the attitude of the individual.81 Crystallized intelligence can increase with self-directed learning and education as long as a person is alive. The measurement of crystallized intelligence is usually in the form of culture-specific items such as number facility, verbal comprehension, and general information.
Fluid intelligence, what has been called “native mental ability,” is the product of the brain’s information processing system. It includes attention and memory capacity and the speed of information processing used in thinking and acting.82 It is not closely associated with acculturation. It is generally considered to be independent of instruction or environment and depends more on the genetic endowment of the individual.9 The items used to test fluid intelligence include memory span, inductive reasoning, and figural relationships, all of which are presumed to be unresponsive to training. Because fluid intelligence involves those intellectual functions most affected by changes in neurophysiological status, it has been generally assumed to decline with age. Several studies have shown this to be untrue; one study noted that during middle age, scores on tests for fluid intelligence are similar to scores in midadolescence.53,83 These changes, however, are primarily associated with processing speed and working memory and executive function.12,84
Recent studies that have looked at the effects of cognitive changes in activities have shown that older people perform activities at a slower rate and use different areas of the brain in the process compared with younger people. Those additional areas of the brain used have mostly to do with monitoring and processing the ongoing activity.13,85 Activities are therefore performed more in a feedback rather than a feed-forward manner, which also requires more time. So, if older adults are given time to complete tasks, they usually do well.
Botwinick35 described the classic pattern of changes in intelligence with aging. In the adult portion of the life span, verbal abilities decline little, if at all, whereas psychomotor abilities decline earlier and to a greater extent (greater decline if the individual is not engaged in regular physical activity). The period between ages 55 and 70 years is a transition time, and some decreases in performance are noted on many cognitive tests. A substantial decline on laboratory tests of cognitive function is generally limited to those older than 75 years.40 In these latter years, however, the decline in fluid intelligence is offset by the growth in crystallized intelligence for most people unless dementia is present. Although changes may be demonstrated in the laboratory, they may not be significant in the “real world,” and the elderly may be as capable as the young of participating in rehabilitation training. For elderly people to benefit maximally, however, they must control the pace of training because the tasks that are the most difficult for older adults are those that are fast paced, unusual, and complex.86 All physical and occupational therapy treatments with older patients need to be structured to encourage the patient to set his or her own pace. The goal is to have a pace that allows ease of breathing and a comfortable, functional upright posture so that the person can enjoy the experience. Interventions should be predictable and progress by adding one new concept at a time.
“Terminal drop” is another type of cognitive change that differs from those that occur in normal aging and in those with dementia. This involves a decline in IQ scores in persons within the year before their death. This change in intellectual function is thought to result from some predeath changes in brain physiology. Research studies that show drastic decreases in intellectual function with advanced age may have a large percentage of subjects who were near death as a part of the sample.87 Subjects who did not experience this terminal drop would then appear similar to those in studies on normal elderly persons.
Stress and intellectual capacity
Selye55 defined stress as the nonspecific response of the body to any demand made on it. All human beings require a certain amount of stress to live and function effectively. When a stressor (stimulus) is applied, the body predictably goes through the three stages of response called the general adaptation syndrome (GAS). The first response is a general alarm reaction, a “fight-or-flight” response that mobilizes all senses in an effort to make a judgment about the response needed. The older person is at a disadvantage because collecting and processing accurate sensory data are decreased with normal aging owing to short-term memory loss. This will manifest in a patient asking the same question repeatedly during a crisis. The sensory memory in an older person lasts less than 1 second.24 The next stage involves judgment and the selective adaptation to the stressor. A decision is made regarding which action is needed, and all other bodily activities return to homeostasis. The older person is slower to search and retrieve the information from storage. If the stimulus continues and goes beyond the therapeutic or functional level, then the body system or part will gradually experience physiological exhaustion. A person in physiological exhaustion is likely to manifest abnormal responses to any new stimulus. Paradoxical reactions are unusual physiological or psychological responses to stimuli (e.g., an erythematous response when an ice pack is applied or a patient becoming more agitated after receiving a sedative).
With aging, the brain undergoes physiological changes that make the older person less physiologically efficient in her or his response to stressors. The general alarm reaction is poorly mobilized and takes longer to become activated (Arndt-Schultz principle). The stage of resistance should yield a series of responses that allows the body to economize in its response to stress. In persons of all ages who receive too many different stimuli and in the elderly who experience normal levels of stimuli, the body becomes less efficient at turning off the general alarm response and replacing it with more appropriate and limited responses. When a person is overwhelmed by this type or level of stress, the individual may demonstrate mild global or specific cognitive impairments, especially mild short-term memory loss.88
The assessment of an elderly person, with or without dementia, must include a determination of the type, number, and severity of the patient’s current stressors. Positive life events (e.g., marriage or the birth of a grandchild) are also stressful life events. Scores that rate stressful life events can identify patients who are at greatest risk of physiological and emotional exhaustion.89 Developed in the 1970s, the Holmes-Rahe Social Readjustment Rating Scale is still a commonly used life stress evaluation tool (see www.stresstips.com).90 Elderly patients, with their numerous psychosocial problems and chronic and acute illnesses, are likely candidates for physiological and emotional exhaustion and the development of psychopathology. Thus the environment and process of rehabilitation care need to be modified to counteract the effect of stress on the intellectual capacity of the older patient. Any action that modifies stress so that a deterioration of intellectual function is stopped or reversed is an efficient and cost-effective part of the total rehabilitation effort.
Strategies for assessing, preventing, and minimizing distortions in information processing
Mini-mental state examination and other cognitive scales
The Mini-Mental State Examination (MMSE) was developed as a result of a study noting that 80% of cognitive disorders among elderly people were not detected by the general practitioner.20,91 It appears to be the most predictable test but is only helpful if all caregivers can monitor the cognitive state of the older patient. All caregivers must be part of the team effort to get a real 24-hour picture of the cognitive capacities of the patient. Although training is improving in this area, most professionals on the rehabilitation team (physicians, nurses,92,93 physical therapists94 and social workers95) are likely to have had only minimal specialty training in gerontology and the unique symptoms and needs of the elderly.
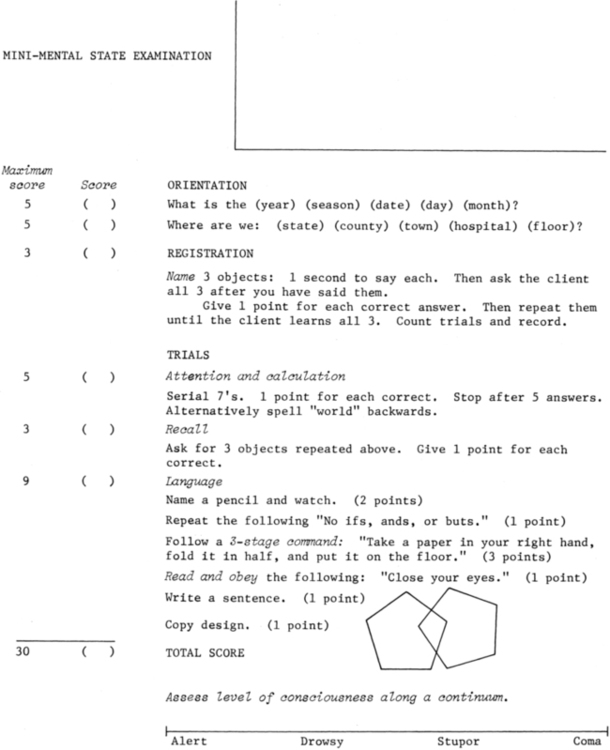
The MMSE provides a screening test for identifying unrecognized cognitive disorders in the elderly (Figure 27-1).21,96,97 The MMSE assesses only cognition and does not examine other aspects of the traditional mental status examination such as mood, delusions, or hallucinations. The test can identify whether the patient is oriented; remembers (short term); and can read, write, calculate, and see and reproduce in drawing the relation of one object or figure to another. The examination is used to screen for cognitive dysfunctions, much as a measurement of blood pressure or blood sugar is used to screen for significant medical disorders. The MMSE also may be used in a serial fashion to quantify changes in a patient’s cognitive status over time. This examination can be used as a springboard for planning how to carry out the traditional rehabilitation evaluation of a patient who has some intellectual dysfunction.98,99
The MMSE has been standardized for elderly persons living in the community. The scores on this test correlate significantly with the Wechsler Adult Intelligence Scale and the Wechsler Memory Test. The MMSE is reported to have a high test-retest reliability for both normal and psychiatric sample populations with r = 0.89 or greater. It has been found that when a cutoff score of 24 is used for the detection of dementia, the MMSE had a sensitivity of 87.6% and a specificity of 81.6%.96 Several studies have noted that interviews with informants are highly consistent with elderly persons’ scores on the MMSE.100
The examination takes only a few minutes to administer, is scored immediately, and can be administered by any member of the rehabilitation team. The entire examination grades cognitive performance on a scale from 0 to 30. A score of 24 or less usually indicates some degree of cognitive dysfunction, but some patients with dementia may score above 24 and some with depression or delirium may score significantly below 24. A low score on this examination can mean that the patient probably has dementia, delirium, mental retardation, amnestic syndrome, or aphasia. A low score on the MMSE can indicate the areas of specific cognitive impairment and gives the rehabilitation team data about how to best communicate with the patient. MMSE scores are also correlated with educational level, with scores dropping 10% to 20% for people with an eighth-grade education or less if older than 70 years.101 A shortened version of the MMSE has been developed that uses only 12 of the 20 original variables. Although the original study suggested that the shortened version of the MMSE is equally as effective as the full MMSE in identifying elderly patients with cognitive deficits, more recent studies have questioned these findings. Another test recently developed to screen for cognitive deficits is the Mini-Cog. It is reported to have higher sensitivity and accuracy of classification because it is not biased by language or educational level.102
Sensory and perceptual changes with dementia
Patients with dementia may have specific problems that inhibit the integration of sensory input. Aphasias and disruption of association pathways may inhibit the patient’s ability to integrate accurately perceived sensory information in a meaningful way. Bassi and colleagues103 and Fozard104 have demonstrated that patients with AD, multiinfarct dementia,105 and alcoholic dementia may demonstrate disturbances in visual acuity, depth perception, color differentiation, and differentiation of figure from ground when compared with normal age-matched control subjects and normal younger subjects.
An assessment of specific sensory systems is necessary when a person demonstrates cognitive losses. The challenge in rehabilitation is to design a process and environment of care so that compensation and modification maximize the ability of the elderly patient with sensory deficits to adapt to most life situations. The example of visual deficits is a case in point. One of every two blind persons in the United States is older than 65 years (see www.afb.org/ and click on AFB senior site).106 Techniques of environmental adaptation and special measures to organize care to help elderly blind people have allowed many of them to live independently in the community.107 However, many elderly people with visual impairments are not blind. Some of the structural changes that result in mild to moderate deficits of vision include yellowing; uneven growth, striation, and thickening of the lens; increasing weakness of the muscles controlling the eye; alteration in the perception of color (especially fine distinctions in tone and brightness); and slower adaptation to light.104 Modifications of the environment can include adequate effective lighting (including adequate intensity and controlling of reflection), dark and clear large-print, low-vision aids (e.g., magnifying glass), verbal orientation and escort by persons accompanying patients in a new environment, consistent furniture placement, explanation when changes occur, clear hallways, a systematic storage system for clothes and toilet articles, and the use of consistent contrasting colors to identify doors, windows, baseboards, and corners.77,92,104,108
Older adult learning styles and communication
Learning occurs throughout life.86 In physical and occupational therapy, habilitation occurs when the client learns new skills, and rehabilitation occurs when the person relearns old adaptive skills. As with intelligence, the learning process does not change abruptly when an individual reaches old age, but differences in performance have been reported. One challenge for rehabilitation therapy is to find ways to improve the efficiency of learning by the older person.
Botwinick35 has noted that learning and performance are not the same. Poor performance on a learning task may mean that insufficient learning has occurred, that learning has not transferred to a new environment or task, or that the performance does not accurately reflect the extent of learning achieved.9 The key variables that affect a person’s ability to participate in a learning task can include intelligence, learning skills acquired over the years, and flexibility of learning style. Noncognitive factors also can have a strong bearing on an individual’s performance. The noncognitive factors include visual and auditory acuity, health status, motivation to learn, level of anxiety, the speed at which stimuli and learning are paced, and the meaningfulness to the individual of the items or tasks to be learned. Research has shown that learning styles change over the life span and that people learn better when instructional approaches are matched to their learning style.25 Therefore a rehabilitation assessment needs to include a review of the preferred learning style of the patient. This is particularly important before discharging a patient from a rehabilitation program. The rationale is that a lack of progress may not reflect the patient’s lack of capacity for rehabilitation, but rather may reflect a dissonance between the patient’s learning style and skills with the presentation of materials in the treatment program (e.g., verbal input has not been adapted to match the level or pace of comprehension of a person who may have a strong preference for visual learning and slower pace).
Interference
Interference can make the learning process less efficient in two major ways.109 First, interference can result from a conflict between present knowledge and the new knowledge to be learned. Second, if the task to be learned has two or more components, secondary components may interfere with the learning of the primary components. This is particularly true if secondary components overlap in time or use the same sensory modality.82 The elderly have special difficulties if they must concentrate on intake, attention, and retrieval processes at the same time. Therefore the process and therapeutic environment of rehabilitation for the elderly patient must not be disturbed by background noise, other stimuli in the environment, or anxiety. When learning a new task, the elderly patient may require a quiet room with no stimuli other than that offered by the therapist. The need to rid the environment of distractions is particularly important when working with an elderly patient with dementia because this patient will have greater difficulty filtering out irrelevant sensory inputs compared with elderly patients without dementia.
Pacing
The pacing of therapeutic intervention is a significant variable in helping an elderly person learn. Elderly persons (with or without dementia) perform best if they are given as much time as they need and when learning is self-paced.35 The major drawback of a fast pace (as perceived by the patient) is that the elderly person generally chooses not to participate rather than risk making a mistake. A lack of response by the patient is often interpreted as apathy, poor motivation, or “confusion.”110 Patient participation is increased when extra time to complete a rehabilitation task is offered. After the individual assessment, group work (where concepts can be presented, reviewed, and examined at leisure) also can be used to reduce the psychological pressure of faster paced one-on-one learning. The details of therapy must be planned carefully, including how questions are asked (this involves asking clear and precise questions in nonmedical language) and, most important, setting aside enough treatment time so the patient can respond at a manageable pace.
Organization
If data are organized in the brain as part of the learning process, the retrieval of these data becomes easier. Older persons are less likely than members of other age groups to organize data spontaneously to facilitate learning and later retrieval (memory) of that learning.37 Elderly people who are highly verbal show fewer weaknesses in the ability to organize stimuli. Elderly persons with poor verbal skills show significant improvement in data retrieval when strategies for organization of data are provided by others (e.g., the therapist). Older learners have difficulty following content because they cannot anticipate what will be taught and do not see the “whole picture” of what is being presented.111 This is an example of how organization may influence the learning process.
Organizing therapy by beginning with an overview in outline form of the entire lesson is helpful. This presents the patient with a conceptual map of the upcoming experience. The use of purposeful organizing also can help bridge the gap between what the older person knows and the new information or task to be learned. The use of neurolinguistic programming (NLP) is especially effective with elderly patients and patients with cognitive deficits because it builds consciously—through language, kinesthesia, and visual input—a picture of a new concept from a known and familiar frame of reference.111
Several other strategies exist for maximizing the efficiency of older adult learners based on awareness of normal age-related changes. Some of the more frequently used techniques are summarized in Box 27-1.
Communication
For persons with cognitive disturbances, familiarity and rituals are keys to ease of adaptability. The basis for rituals is well-organized documentation to which all caregivers have access and contribute on an ongoing basis. This information needs to be filtered and organized so that each shift can see what is working for the patient today. Even a nonverbal patient can relate effectively to bathing if a ritual exists regarding dressing and undressing (e.g., the socks always come off first). Mace and Rabins99 spelled out the details of the importance of caregivers being aware of the power of familiarity and rituals. Mintzer and colleagues112 reinforced the same idea in their research on the effectiveness of alternative care environments for agitated patients with dementia. Another detail that requires staff or caregiver attention, evaluation, and adaptation in daily care is ideational apraxia. LeClerc and Wells113 described this as “a condition in which an individual is unable to plan movement related to an object because he or she has lost the perception of the object’s purpose.” This is especially important in relation to feeding, dressing, toileting, and bathing. The authors described a tool that can help caregivers assess ideational apraxia and problem-solving compensations to prevent unnecessary agitation or disability and take actions to preserve existing abilities. Savelkoul and colleagues114 emphasized the importance of effective communication between staff and patients and the importance of routines for patient care to maximize functional behaviors for institutionalized elderly living in residential homes. Another key point noted was that staff corrected and tested residents too often, which can create agitation and anxiety. This appeared to be related to lack of training and information on the part of the staff about the dementia and cognitive status of patients as well as a lack of support from other staff.
The research findings and techniques previously discussed describe many of the aspects of the Feldenkrais approach to learning.1,14 The Feldenkrais Method has been applied to the needs of elderly persons with good results. The principle that learning needs to be pleasurable is especially applicable to elderly clients (with or without dementia) because they are often under more stress and have fewer supportive resources to cope with a crisis. Despite changes in learning style, the older person (with or without dementia) can be helped to learn more efficiently through well-planned instruction. The use of techniques to increase learning efficiency in the elderly has been demonstrated to decrease the stress that at times may result in emotional or cognitive overload and abnormal cognitive reactions.
Ann115 notes that because habits and procedural memory (behaviors learned by doing) are two of the last areas of the brain affected by AD and dementia, individuals with these diseases can often walk around after they are no longer able to be aware of their surroundings, consistently communicate, or reason. The Feldenkrais Method taps into an individual’s habits, producing positive and lasting results through the capacity of the individual to still use procedural learning (even though she or he is not able to describe verbally or be consciously aware of the learning that is achieved). One example of how the Feldenkrais Method taps into procedural memory follows. Lee, a man of age 92 years with advanced dementia, was able to achieve changes in his behaviors, even though he was worked with while he was sleeping, which changed his behavior while he was awake. Because of Lee’s constant walking and potentially combative behavior, working with him initially was difficult. When he was asked to sit or lie down, he complained loudly and told the therapist to get away. Instead, the therapist worked with him during his frequent naps. He walked bent over with his feet and legs turned out and a wide stance. He held both arms close to his sides, with his elbows bent and no arm swing. He was unable to move isolated areas of his torso; he therefore did not turn his head to look at something next to him. Instead, he turned his whole body. Lee would decide to sit down without looking to see if a chair was behind him, partially because he did not have safety awareness and partially because he did not have the capability to rotate his body. Immediately after waking up or finishing a meal, he would start to walk. As a result of these limitations and actions, Lee was constantly falling. Lee needed to learn how to differentiate the movement pattern of turning his head separate from his trunk. Lee had a pattern that was “un”differentiated in which he moved his head and trunk as a single unit; he had no choice to do anything else. Through gentle movements while Lee was lying on his back or side, the first several sessions involved exploring passive movement of his pelvis and spine. The focus was to explore with Lee his capacity to move in diagonal patterns and to create a kinesthetic relationship between his right shoulder and his left hip and vice versa, the sensation of elongating his spine and learning to twist his torso. He began to demonstrate the capacity to breathe by allowing his chest to expand in the lower rib area. The passive movement explorations involved exploring upper torso rotation, including head turning, shoulder blade differentiation, and the ability to move the shoulder blades independently of his ribs, and connecting movements of the ribs and chest to flow with the movements of the upper spine. After the third session, Lee stopped falling while walking. Although he still exhibited rigid movements and difficulty moving his arms away from his body, he shifted weight a little more easily and demonstrated minimal trunk rotation for walking in both directions. Lee did not fall for several months until he stopped walking because of a sore on the ball of one foot. Lee gradually discovered how to allow the therapist to work with him and the protest stopped. This ability to learn to allow the therapist to sit next to him and touch him is an example of learning through use of emotional memory, another type of memory that seems to work in conjunction with procedural learning. Both procedural and emotional memory are preserved long after other memories are lost. Even without cognitive recognition, emotional memory capabilities in persons with AD allow them to communicate and establish trust with another human being and learn new functional ways to balance in gravity.
Another example is Dina, an 83-year-old with advanced AD, Parkinson disease, depression, and cataracts. The Feldenkrais sessions with her demonstrated the power of focusing the communication and interaction on keeping the activities pleasant and working within the comfort zone of the patient. The chief problem was that the patient had swollen knees and had not been able to straighten her knees past 90 degrees for the previous 2 years. Dina had received traditional physical therapy in which the intervention included attempting to straighten the knees by placing a weight on top of them. Dina cried during this treatment and reported pain. She could not propel her own wheelchair, and it took two staff members to transfer her to and from her wheelchair. Her reaction to their attempt to transfer her was to lift her legs off the floor and give them her entire weight. She did not rest her feet on the floor, even in sitting. Dina had difficulty lying in all positions. When on her back, her lower body twisted to the side. She stayed where she was placed and in the position she was placed in. Dina was unable to specifically point to a body part and say it hurt her. The focus of the first session was to explore how to help her rest more comfortably. The first efforts were to try to enhance mobility in her ribs and spine. After the first session, she was able to rest more fully on one side. After the second session she was able to rest more fully on both shoulder blades and on her pelvis evenly. After the fourth session, Dina began wheeling herself in the wheelchair with her feet, and staff reported that later in the day they saw her stand up from the wheelchair for about 1 minute by herself. None of the sessions had involved direct work with her legs, and the progress in her ability to participate in her life points to the fact that movement deficits are not always the root of problems. The capacity to feel safe and allow touch and other physical and social communication can create improvements in the ability to live in gravity and assist caregivers with the chores of life. The Feldenkrais Method is an example of effective, functional communication, manual therapy, and neurological rehabilitation that enhances daily living skills in people with AD and other dementias.1,14,115
Environmental considerations
Hypothermia
The temperature of the living environment must be carefully controlled because aged clients may not perceive that the environment is cold and may not experience shivering. Accidental hypothermia can develop in an older person even at temperatures of 60° F (15.5° C) to 65° F (18.3° C). Accidental hypothermia is a drop in the core body temperature to less than 95° F (35° C). Patients at risk for hypothermia are presented in Box 27-2.
The symptoms of hypothermia may include a bloated face, pale and waxy or pinkish skin color, trembling on one side of the body without shivering, irregular and slowed heartbeat, slurred speech, shallow and slow breathing, low blood pressure, drowsiness, and symptoms of delirium. The two principles of treatment of hypothermia are that the person will stay chilled unless the body temperature is slowly increased and that he or she should be evaluated by a physician, regardless of the apparent severity of the hypothermia.9,116
Patients and their caregivers may attempt to save money by lowering room temperatures and thus inadvertently cause hypothermia. To prevent accidental hypothermia in institutions with central air conditioning, special accommodations for the elderly, such as a special wing of the building or individual temperature controls in the rooms, are required.116
Emotional capacity to participate in a learning task
Many elderly persons who come for physical therapy are in a state of emotional overload, as evidenced by disorientation, depression, anger, or a withdrawn and apparently uncooperative attitude. A person who is at or near the point of emotional overload needs to be evaluated regarding his or her ability to be involved in learning tasks that require active participation. If the patient is in emotional overload, forms of therapeutic intervention that temporarily allow the patient to be a passive recipient of therapeutic intervention can be used. Various types of therapeutic interventions, including massage, connective tissue massage, heat, breathing exercises, relaxation exercises, and Feldenkrais Functional Integration, can promote a relaxation response, lower the anxiety level, reinforce self-pacing of activity, and thereby prepare the patient to participate in more physically active types of therapeutic exercise.117 If asked directly, most patients will state whether they feel able to participate actively.1,14,115
Delirium and reversible dementia: evaluation and treatment
 The amount of time that has elapsed since the onset of symptoms
The amount of time that has elapsed since the onset of symptoms
 The progression or lack of progression of symptoms
The progression or lack of progression of symptoms
 Associated functional impairments and associated medical signs and symptoms
Associated functional impairments and associated medical signs and symptoms
 Use of prescription drugs, over-the-counter medications, home remedies, illegal drugs, alcohol, caffeine, and nicotine
Use of prescription drugs, over-the-counter medications, home remedies, illegal drugs, alcohol, caffeine, and nicotine
The causes of delirium and reversible dementia are many. In the elderly person, however, certain causes are more common than others (Box 27-3). Alcohol and drugs (prescribed, over-the-counter, or illegal medications and home remedies) are prime offenders (see Chapter 36). The delirium may be the result of intoxication, side effects, or withdrawal syndromes.70 Benzodiazepines are among the most commonly prescribed offenders; even a low dose (2 mg) may cause demonstrable cognitive changes.54 Other common drugs that cause delirium or reversible dementia are alcohol, oral narcotics, psychotropic medications, steroids, antineoplastic drugs, digoxin, anesthetic agents, antiparkinsonian drugs, and antihistamines. However, all drugs have the potential to cause significant cognitive problems in the elderly.118 These symptoms often resolve with discontinuation of the offending agent or treatment of the withdrawal syndrome. For some patients a medication holiday of longer than 24 hours may be needed before a positive change in cognition can be noted.67
At times, the symptoms may be clearly correlated with the pharmacokinetic profiles of the medications taken by the client. The dose or frequency of administration of medications can be a contributing factor to a delirious state.119 Every member of the rehabilitation team needs to document the patient’s ability to participate in learning tasks and the time of the assessment because timing of medication administration can affect functional performance. The rehabilitation team needs the input of a clinical pharmacologist who can help the team focus on concepts such as biological half-life, clearance, bioavailability of drugs, and the time course of drug concentration in plasma as a function of dose and frequency.
Several medical diseases are likely to cause symptoms of delirium or reversible dementia, which will also reverse with treatment of the underlying disease. Urinary tract infections, more common in women, are the cause of delirium in 28%120 of elderly patients. Fecal impaction is another common cause of acute cognitive change in elderly persons. Others are distended bladder caused by prostate enlargement or drug-induced urinary retention, dehydration, malnutrition, cardiovascular disorders,116 metabolic disturbances (particularly undiagnosed diabetes mellitus),18 endocrine diseases, renal diseases, hematological diseases, pneumonia or bronchitis,116 and vitamin B12 deficiency.
Transient (and usually mild) cognitive deficits may be the result of a cerebrovascular accident (CVA). The cognitive deficits after a CVA are often reversible, although they may last for several months after the stroke. The rehabilitation team needs to evaluate and regularly reevaluate the patient’s cognitive capacity and build a program of care around current abilities. A program of therapeutic intervention that allows the older person to work in a self-paced program for 1 to 3 months can yield good therapeutic results and also prevent unnecessary secondary deconditioning until part or all of the patient’s cognitive capacity returns.121
Depression is commonly misdiagnosed as dementia in the elderly.116,122 For many years depression was thought to be a form of “pseudodementia” or false dementia.123 Depression can result in mild and subtle cognitive changes affecting immediate recall, attention, and the ability to perform basic ADLs. Some reports noted that as many as 31% of those thought to have dementia have depression instead.124 However, recent research has clarified the close relationship between structural changes in the elderly brain and the onset of depression, thus bringing the concept of pseudodementia, or depression as a reversible dementia, into disrepute.125,126 Depression is a treatable disorder, and many patients with cognitive impairments show some improvement in their cognitive functioning if the depression is treated; however, the underlying cognitive problem does not resolve with treatment of the depression.127
Because the presence of depression can interfere with the progress of rehabilitation through cognitive deficits or its effects on motivation, this disorder needs to be diagnosed early and accurately. The Geriatric Depression Scale, a 30-item yes-no questionnaire, screens for this disorder.128 No arbitrary cutoff score signifies depression in this test, and most individuals with a score of 15 or higher have this disorder. The higher the score, the more likely that the patient has depression and the severity of the depression is greater.
Depression after a stroke can produce a reversible decline in cognitive performance.129 Depression after a stroke is more likely to occur in patients with left hemisphere lesions and as the site of the lesion moves toward the frontal pole.9 The relation between site of lesion and depression also has been noted on neuropsychological testing.87
The treatment of major depression generally involves pharmacotherapy, psychotherapy, and environmental manipulation, which can require support from the entire rehabilitation team.130 In the treatment of a patient with depression, therapeutic techniques can promote a relaxation response, enhance upright posture, decrease anxiety level (massage, heat, or Feldenkrais Functional Integration), and help bring the patient to the point at which aerobic training is possible, which is known to have a beneficial effect. All aerobic training for the elderly needs to begin with a stress test, modified as necessary to determine the patient’s exercise target heart rate. The modification most commonly required is use of the upper extremities to achieve the training effect, because lower- extremity function may be limited, or use of major ADLs involving the upper extremities as the stress test or training program.
The causes of delirium and reversible dementia are usually treatable, and if diagnosis and care are provided in a timely fashion, the patient can likely regain full command of his or her cognitive processes. When this does not happen, the patient probably had mild, irreversible dementia that remained hidden until the onset of an acute problem that uncovered the poor cognitive functioning. The length of time in an institution (hospital or nursing home) needs to be kept as short as possible to avoid learned dependency and learned helplessness,130 which make a return to full cognitive functioning and independent living difficult.122
Irreversible dementia
The course of irreversible dementia is unique for each patient. The variation in clinical course occurs based on the cause of the underlying disease and superimposed biological and psychosocial factors, including medications, concurrent illness (including delirium), the nature of the social support system, and the patient’s premorbid personality structure. The causes of irreversible dementia are summarized in Box 27-4.
Regardless of the cause of the dementia, the clinical course of these disorders has several commonalities.83 Most of these diseases are progressive. Symptoms may be subtle early in the course of the illness, and the onset of disease is usually noted by the person with the disorder, family members, friends, or colleagues at work rather than by a physician. The signs of impairment of mental ability are typically memory loss, poor judgment, or incompetence at work. The patient can often succeed at hiding his or her symptoms for a while. The social consequences of the cognitive impairment usually bring the patient to the attention of health care professionals. In addition, the patient with dementia can manifest a variety of psychiatric symptoms, including mood disturbance, agitation, violent behavior, socially inappropriate behavior, delusions, hallucinations, catastrophic reactions, and perseveration.99,131 The pattern of onset and the types of psychiatric symptoms are often directly related to the underlying pathological condition.
When a physician is finally consulted, the diagnostic process can begin. When a complete diagnostic evaluation—including history, physical examination, neurological examination, neuropsychological testing, and laboratory testing (Box 27-5)—is performed, an accurate diagnosis can be made in approximately 90% of patients, although experienced geriatric psychiatrists can make an accurate diagnosis in more than 95% of patients.132
Once the diagnostic process is completed, treatment can be started. Medications can assist in reversing underlying causes in only a small percentage of cases; patients in whom drug therapy is successful usually have potentially reversible dementia that has gone untreated and now have permanent sequelae of the disorder. Medications may be able only to slow the process of an irreversible disorder (e.g., tacrine for AD) or prevent further deterioration (e.g., aspirin for multiinfarct dementia). Psychotropic drugs may reverse depression or the behavioral symptoms associated with dementia.124,130,133 Medical management also involves the prevention and treatment of other medical conditions and side effects of the new interventions as they are added.
Medical management of irreversible dementia focuses on maximizing the patient’s remaining functions and roles, rehabilitating some lost functions, and providing family education and support.99 Training caregivers to adapt to the patient (e.g., modifications for getting the patient out of bed, bathing), simplifying the individual’s living space, and referring relatives to family support services are some of the issues to be addressed.134
Alzheimer disease
The treatment of irreversible dementia is a long-term process. Recent studies have found that the average duration of illness from first onset of symptoms to death is 8.1 years for AD, 6.7 years for multiinfarct dementia,135 and 5.6 years for Pick disease.124 Medical and nursing care can extend the life expectancy of patients with dementia for up to 20 years or more.
In 1907, Alois Alzheimer34 described the case and the neuropathology of a 54-year-old woman who developed morbid jealousy, which was followed by loss of memory, inability to read and understand, and death 4.5 years after onset of the illness. Since then, it has been noted that 50% of patients with dementia have AD.101 In making the diagnosis of AD, all other causes of cognitive dysfunction must be ruled out. The disease can occur at any age, but the onset of the disease is almost always after age 65 years. The prevalence of the disease gradually increases to a rate of 20% in persons older than 85 years.33
Traditionally the symptoms of AD have been thought to progress in three stages.
Stage 1 lasts from 2 to 4 years and involves loss of functional skills or orientation, memory loss, and lack of spontaneity. The patient is often aware of the losses and is, in many cases, able to cover up the cognitive losses by talking around the issues. During this stage the patient and family may need to deal with the issue of giving up a job, hobbies, or other types of meaningful activity because of the patient’s inability to carry them out safely and independently. The patient begins to lose the ability to handle money and a personal budget, drive a car safely, and tell time. The family or significant others may have to come to terms with the question of whether the patient can live alone. Depression is common during this stage of the disorder.130
There is wide agreement now on a seven-stage scale to describe the progression of Alzheimer’s (see www.alz.org/alzheimers_disease_stages_of_alzheimers.asp). This scale is probably the most accurate staging system for AD and correlates more closely with the progression of different sets of symptoms through the course of the disease.
The barthel index
The Barthel Index (Table 27-1) is a profile scale that rates 10 self-care, continence, and mobility criteria.136 The specific rating guidelines used in scoring are presented in Appendix 27-A. The advantage of the Barthel Index is its simplicity and usefulness in evaluating patients before, during, and after treatment. It is functionally oriented and may be best used when accompanied by a clinical evaluation.87 The scale allows documentation of functional changes over time. It is useful when discussing with families the need for help for the patient who cannot manage self-care (ADLs and/or IADLs). Work continues to develop more effective and reliable scales for assessing function and status in people with AD.137
TABLE 27-1 
| WITH HELP | INDEPENDENT | |
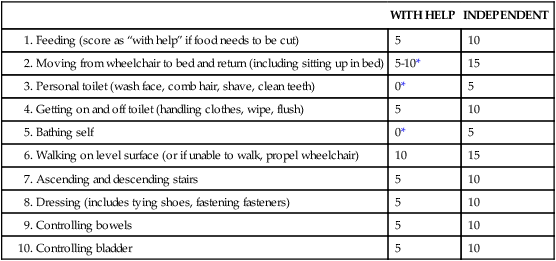
*A score of 0 is given in the activity when the patient cannot meet the criteria as defined (see Appendix 27-A).
Modified from Mahoney FI, Barthel DW: Functional evaluation: the Barthel index, Md State Med J 14:61, 1965.
Strategies for treatment and care
Once the diagnosis is established, treatment planning for long-term care at home or in an institution must be carefully made. No matter where the patient will be living, involvement of the caregivers and significant others is essential to maximizing functional outcomes. The emotional, physical, and financial resources of the patient and family or significant others who will be the caretakers must be ascertained. A review of the caretakers’ willingness to perform basic tasks or make visits, their willingness to learn and teach the necessary skills, and the realistic need for respites must be determined.138 Family training and orientation manuals that deal with all the details of caring for a person with dementia are available (see www.alz.org/living_with_alzheimers.asp).99 The same detailed orientation is needed for institutional staff who care for elderly patients with dementia. The structure and process of care can help patients be maximally active in their self-care and prevent unnecessary anxiety and catastrophic reactions.
Supporting families and caregivers with their own sense of loss, frustration, and helplessness
Family, significant others, and caregivers go through their own coping and adaptive process as the patient experiences gradual or sudden cognitive disturbances.139 These people have a history with the patient and have expectations about what the relationship and communication should be. As cognitive disturbance occurs, they experience a series of losses because the patient is no longer able to respond and interact as he or she has in the past. With progressive cognitive decline, family and friends experience ongoing losses because the patient is continually changing and less able to relate. For many patients with cognitive disturbances, at the final stage all communication disappears and the family is left with only nonverbal communication or no communication at all. Staff who work with a patient over a period of time also face their own personal reactions of loss, unfulfilled expectations, and a continual need to reassess how to relate effectively to the patient. The responsibility for creating a positive relationship falls on the people who are interacting with the patient. The family and caregivers themselves need training and ongoing support in learning how to nurture and maintain an ongoing relationship with the patient. This requires that caregivers and family members be aware that they are in a healing process as they relate to the loss of the relationship that previously existed.
Epstein: stages of healing for caregivers
Epstein140 provides a workable description of the stages of healing that occur when major trauma or loss occurs. Epstein defines healing as “putting right our wrong relation to our body, to other people and . . . to our own complicated minds, with their emotions and instincts at war with one another and not properly understood and accepted by what we call ‘I’ or ‘me.’ The process is one of reorganization, reintegration of things which have come apart.”140 When a patient experiences cognitive changes, the first stage of response by those who care for or love this person is suffering. Chaos exists during this traumatic time. For example, the patient suddenly cannot understand simple directions on how to operate the new electric cart and insists on getting the old one back. The family is upset and arguments ensue. The family and patient together eventually get a medical workup and they are told that “Mom has some type of degenerative cognitive problem.” They all experience a profound sense that “something is wrong.” The response to helplessness for most human beings is to resist. The lesson of this stage is acceptance. When acceptance is present, then detachment from the emotions is possible. With acceptance present, adaptation and compensation for losses are possible. In the example noted, this would mean that the family would return the new electric cart and have the old (familiar) model refurbished. The family would get training from the therapist in exactly what skills of interaction Mom does not have so that they can work to avoid creating situations in which she feels “stupid and helpless.” When a cognitive loss is truly present, training in skills only creates frustration in the patient that may lead to anger and rage. The staff and family need to be trained to understand the exact nature of the losses and provide appropriate compensations in their oral communication and how they relate to the patient.
Stage 10 is the time to connect with the creative force of the universe. The spiritual process is brought to the issue at hand. A sense of great wisdom and oneness with all creation is felt. When working from this state of being, the caregiver has the unique capacity to speak or act to bring out the best in others. In health care, some caregivers have the special gift of allowing themselves to step into the mental world of the other person and thereby create communication that will be heard and that can be acted on even by those with limited mental capacities. The most interesting thing is that the patients can often tell if a caregiver is in this unique state because they will come and sit next to the caregiver or want to hold hands. This state of ease and connection can be learned. A possible resource for exploring these skills is an organization called Landmark Education ([415] 981-8850; www.landmarkeducation.com), which provides programs and courses that examine how people listen, what bias they bring to the communication process, and specific speech strategies to bring out the best in others.
In-service training can offer a basic introduction to strategies for lifelong learning, healing, and self-awareness. “What works for me?” “What is the easiest way to learn new skills?” “What strategies enhance adaptability?” This type of learning is nonlinear and is the model a scientist uses to conduct an inquiry. Recently more attention has been paid to managing stress and the role of spirituality in processing grief and loss among caregivers and family.141–143
Role of the physical therapist: development of interventions and caregiver training
As a part of the rehabilitation program, caregiver training for this group of patients needs to emphasize reassurance, hands-on interventions, and communication to allow treatment to proceed at a pace perceived as reasonable by the patient.67 In the early and middle stages of all dementias, physical therapy intervention usually can prolong the ability to move with ease in ADLs and IADLs and maintain the ability to participate in some social activities. This is extremely important for caregivers because deficits in the patient’s ability to perform ADLs and IADLs often relate to the inability to physically perform these activities under supervision.47 The ability to walk is lost late in most dementias, but gait and coordination disturbances are common and can benefit from physical therapy.144–146 Therapeutic intervention to assist the patient and train the caregivers involves facilitation of ease of movement and motor planning and developing or refining environmental and cognitive cues to assist in carrying out complex tasks. Ultimately, caregivers require training in how to move, lift, and otherwise assist the patient.
Although not able to reverse the progressive cognitive decline, the exercise intervention that the physical therapist can develop may improve the level of function, confidence, vitality, and safety of the patient and ease the burden of care for the caregivers. Research is beginning to establish an important role for exercise in maintaining physical activity147,148; contributing to general health and slowing of cognitive decline149–152; as well as maintaining strength and aerobic conditioning.153 Guidelines for exercise prescription include aerobic, strength, balance, coordination, and flexibility activities determined by direct assessment, and suggestions for motivational and problem-solving strategies. The Seattle Protocols are an important contribution in this area.154,155 Research shows that exercise not only increases strength, coordination, and aerobic capacity but also creates beneficial changes in brain plasticity.156–158 Further studies need to be done to work out more clearly what types of exercise are beneficial in what ways for what populations.159
The accurate assessment of IADLs and ADLs is more reliable than medical diagnosis for predicting the amount of assistance and interaction a person will need in a nursing home (see Table 27-1 and Appendix 27-A).136 The first goal of rehabilitation for patients with dementia is to create a supportive emotional and physical environment. In other words, the environment must actively work to compensate for the patient’s cognitive and functional losses as they occur. The ultimate goal is to help patients feel they are capable so that they will continue to try to do those things for themselves that they can do safely, whether they remain in their home or live in an institution. Orientation and training of significant others is also important so they feel comfortable allowing the patient to participate safely in activities and basic self-care tasks modified to their cognitive level.
The Alzheimer’s Association ([800] 272-3900; www.alz.org) is a resource for professionals and caregivers of people with dementia. The goals of the association are the following:
 To support research related to the diagnosis, therapy, cause, and cure of AD and related disorders
To support research related to the diagnosis, therapy, cause, and cure of AD and related disorders
 To aid in organizing family support groups; to educate and assist affected families
To aid in organizing family support groups; to educate and assist affected families
 To sponsor educational programs for professionals and laypersons on the topic of AD
To sponsor educational programs for professionals and laypersons on the topic of AD
 To advise government agencies of the needs of the affected families and to promote federal, state, and private support of research
To advise government agencies of the needs of the affected families and to promote federal, state, and private support of research
 To offer help in any manner to patients and their caregivers to promote the well-being of all involved
To offer help in any manner to patients and their caregivers to promote the well-being of all involved
The Alzheimer’s Association promotes the provision of humane care to the patient with dementia or related disorders throughout the course of the illness. Other support groups have been tried in communities in which spouses have worked to develop ongoing respite care.160
As a member of the rehabilitation team, the physical or occupational therapist can conduct an inventory of services as a part of the annual review of the quality of care that is provided for a patient with dementia. Surveys of persons caring for patients with dementia listed the following services in their perceived order of importance83,161:
1. A paid companion who can come to the home a few hours each week to give caregivers a rest (respite)
2. Assistance in locating people or organizations to provide patient care
3. Assistance in applying for government programs, such as Medicaid, disability insurance, and income support programs
4. A paid companion who can come to the home for overnight care so caregivers can go away for one or more days (respite)
5. Personal home care for the person with dementia to help with activities such as bathing, dressing, or feeding in the home
6. Support groups composed of others who are caring for persons with dementia and other cognitive deficits
7. Special nursing home care programs only for persons with dementia and other cognitive deficits while the caregiver is away
8. Adult day care providing supervision and activities away from the home
Not mentioned in this chapter was the need for psychological support for caregivers. The stress on caregivers is extreme, and symptoms of anxiety and depression are common. Because of the relative lack of counseling services for caregivers, however, the use of (and probable abuse of and dependence on) psychotropic medications by caregivers is high.60,162 Because these medications may impair the cognitive functioning of caregivers, the risk of harm to the patient with dementia is also high.
Dementia and delirium: new frontiers
Most current research in delirium and dementia is focused on AD. The Alzheimer’s Association is the largest private foundation funding research on dementia, supporting on average about 100 projects totaling almost $15 million annually. Research is underway to explore possible causes of dementia, including work that examines the roles of neurotransmitters, structural brain changes, nutrition, viruses, drugs, immunological deficits, and heredity in the etiology of AD. Studies to increase the diagnostic accuracy of different forms of dementia, including making a distinction between cortical and subcortical dementia161 or using Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) criteria163 or neuropsychological criteria, are also underway. Newer diagnostic models of dementia, including that caused by stage II or III human immunodeficiency virus infection, are also being studied.164,165 New research that may shed light on the mechanisms of the early stages of AD relates to other neurodegenerative diseases. Persons with dementia who also have parkinsonian symptoms, delusions, and hallucinations have been reported to experience faster decline that those who do not.166 This research team found a relation between the presence of Lewy bodies (abnormal structures in the brain that contain a protein called synuclein) and parkinsonian symptoms; affected individuals had lower survival rates than those with either symptom present by itself.
The most exciting area of research is pharmacology (see Chapter 36). The advent of tacrine, a drug that slows down the progression of AD in some patients, has produced an explosion of research on drugs aimed at stabilizing or reversing the symptoms of this disease. Although no cures are available, some drugs, such as physostigmine, ondansetron, and nerve growth factor, have shown some promise. These studies have spawned a search for new drugs to treat both AD and the symptoms of other dementias.167–169
Research is also being funded that is investigating the best ways to provide care and support in the home and at long-term residential settings.33
Summary
In working with an older person with dementia or delirium, the therapist can do much to make the quality of life better for the patient, family, and caregivers.99 A thorough listing of the details needed to develop an environment and process of care for elderly persons with cognitive deficits can be found in other texts (see www.alz.org/living_with_alzheimers.asp).99,131
Specific examples of modifications of physical and occupational therapy examination and treatment may include working in collaboration with the family, close friends, and other members of the rehabilitation team and developing a consultative relationship with key caregivers (professional and nonprofessional and all shifts of institutional staff) to encourage problem solving and patient participation in self-care. Another important modification includes the evaluation of each patient’s communication abilities before the therapy assessment to adapt the assessment in such a way as to promote patient participation. Case Study examples are presented later in this chapter (refer to Case Studies 27-1 and 27-2) to provide clinical scenarios and corresponding physical and occupational therapy examination and treatment strategies.
Modifications of treatment include the use of gentle, nonverbal neurological rehabilitation techniques (e.g., the Feldenkrais Method). The key is to acknowledge the now well-established research finding that nondeclarative learning and memory (procedural) are available long after declarative learning and memory (ability to consciously learn and remember facts and events) are lost for a person with AD. Motor ability is one of the last areas to be affected by AD.170 Assisting a person with AD to edit procedural memory and increase walking safety is therefore possible. The functional outcomes of this learning can include a decrease in abnormal muscle tone, enhanced sensory awareness and organization for the position of the eyes and head in space, an increase in the ease of movement, an increase in the ease of breathing, enhanced endurance, minimized anxiety, minimized resting muscle rigidity in the chest, and increased patient coordination. The therapist needs to modify the process of neurological facilitation by decreasing patient effort and adding extra cuing and more frequent breaks for integration of learning. Tasks may need to be simplified so that the patient can perform them, and the caregiver is trained to perform only those tasks that the patient cannot perform.
“AD is the most common disorder causing cognitive decline in old age and exacts a substantial toll on society. Although the diagnosis of AD is often missed or delayed, it is primarily one of inclusion, not exclusion, and usually can be made using standardized clinical criteria. Most cases can be diagnosed and managed in primary care settings, yet some patients with atypical presentations, severe impairment, or complex co-morbidity benefit from specialist referral. AD is progressive and irreversible, but pharmacologic therapies for cognitive impairment and non-pharmacologic and pharmacologic treatments for behavioral problems associated with dementia can enhance quality of life. Psychotherapeutic intervention with family members is often indicated, as nearly half of all caregivers become depressed. Health care delivery to these patients is fragmented and inadequate.”36
1. I will ask my patient if he or she would like to pray or worship today, and I will make arrangements to meet those needs.
2. I will speak or communicate in a way that is functional and workable for the patient.
3. I will repeat what I hear and perceive back to the patient to ensure that I capture her or his perspective.
4. I will encourage natural participation by creating a pace that is pleasant for the patient.
5. I will close doors quietly.
6. I will not raise my voice and shout except in a real emergency.
7. I will talk to someone on staff when I get upset or take something personally so I can have peace with co-workers, creating a positive atmosphere for the patients to live in.
8. I will offer to warm up the patient’s tea or coffee and make sure it is not so hot that it could cause a burn.
9. I will create only one choice at a time so the patient can understand and then choose yes or no.
10. I will know what “my” patient has eaten on my shift.
11. I will know my patients’ timing for toileting so I can support their continence and dignity.
12. I will tell the patient I am going to touch him or her before I do so, to avoid surprises.
13. I will walk (rolling or ambulating) with every one of my patients outdoors as often as possible or at least every 3 days to encourage good sleep and mental and physical stimulation.
14. I will sit and visit with each of my patients for 10 minutes (every shift).
15. I promise to listen with an open heart to the patients’ perception of life at the moment.
16. I promise to close the blinds in every room at night (unless the patient requests otherwise) and open blinds every morning to reinforce day-night orientation.
17. I will discover and use the “personal” get ready for bed routine for all patients so they sleep well.
18. I promise to talk and walk at a pace that encourages a sense of safety for my patients.
19. I promise to be self-nurturing and come to work well rested and ready to share myself.
20. I promise to avoid confrontational actions and body language except in an emergency.
21. I promise to respect the unique ergonomics of each patient and adapt as needed.
22. I promise to offer to add support to explore ways to increase comfort.
23. I promise to notice how my patients relate so no one agitates or bothers another.
24. I promise to be kind to myself, other staff, and my patients.
25. I promise to be of service and adapt to meet my patients’ needs.
26. I promise to report problems (equipment, environment, relationships) to the person who can do something about them.
27. I promise not to gossip (talk about others so that it leaves a negative impression and no resolution of the problem).
28. I promise to leave my workspace clean and restocked after I have taken care of the patient (or at least to leave a note to alert the next shift about what has not been done).