CHAPTER 30 Agee Endoscopic Carpal Tunnel Release
Introduction
In 1989, Chow et al. described a two-portal endoscopic carpal tunnel release (ECTR) technique.1 This method has undergone a number of modifications since that time and is described in a separate chapter. Agee et al. published a prospective randomized clinical trial on his uniportal technique in 1992.2 Other investigators have published their preferred technique of using a one- or two-portal approach. The decision as to which technique to use is largely based on personal preference and comfort with the procedure. This chapter discusses the uniportal technique using the Agee endoscope.
Contraindications
Absolute contraindications include any distortion of the carpal canal due to tumor, previous surgery, carpal fracture/dislocation, or mal-union of the radius. A loss of wrist extension of 20 to 30 degrees either from bony fusion or wrist contracture would hamper this procedure by impeding the correct placement of the endosocope. Unfamiliarity with the regional anatomy is another contraindication. Due to the high learning curve, it is recommended that anyone contemplating this procedure should take a cadaver training course prior to attempting it clinically—unless training has been provided in a teaching environment.3
Relative contraindications abound and are not universally agreed upon. Flexor tendon thickening due to synovial hyperplasia or adhesions from previous flexor tendon repairs will complicate the procedure. Recurrent or persistent carpal tunnel syndrome following a previous release often includes a component of traction neuropathy due to scar, which may thwart attempts at ECTR. However, successful cases have been reported.4 Any suspicion of separate entrapment of the recurrent motor branch mandates an open procedure.
Relevant Anatomy
The flexor retinaculum (FR) consists of three distinct and continuous segments that extend from the distal radius to the base of the long finger metacarpal.5 The proximal segment is continuous with the deep forearm fascia and is inseparable from the thickened antebrachial fascia. The transverse carpal ligament (TCL) makes up the second part of the FR. The TCL arises from the scaphoid tuberosity and trapezial beak radially, and from the pisiform and hook of the hamate ulnarly. The distal segment of the FR consists of the aponeurosis between the thenar and hypothenar muscles. The median nerve becomes superficial in the forearm approximately 5 cm proximal to the wrist. It lies between the tendons of the flexor digitorum superficialis (FDS) and the flexor carpi radialis (FCR), and is dorsal or dorsoradial to the palmaris longus (PL).
Surgical Considerations
The position of the ulnar nerve and artery are of particular significance for endoscopic carpal tunnel release. Most endoscopic devices are designed to divide the flexor retinaculum just to the radial aspect of the hamate hook. In an anatomical study of the boundaries of Guyon’s canal, however, Cobb et al. showed that the confines of this space do not extend from the pisiform to the hook of the hamate (as previously accepted).6 The fascial roof extends radial to the hook of the hamate, which allows the ulnar neurovascular bundle to course radial to the hamate hook. Utilizing cross-sectional analysis of nine cadaver specimens, they found the ulnar artery to course radial to the hamate hook in five and palmar to it in four. Therefore, the ulnar artery may be at greater risk of injury during endoscopic procedures than previously recognized.
The safest path for release of the TCL has been studied extensively. Rotman and Manske investigated the anatomical relationships of an endoscopic carpal tunnel device to surrounding soft-tissue structures along the ring finger and the long-ring interspace axis.7 The average distance from the center of the device to the median nerve in the carpal tunnel averaged 3.3 mm in the ring finger axis and 2.5 mm in the long-ring interspace axis. The average distance from the distal edge of the transverse carpal ligament to the superficial palmar arch was 4.8 mm in the ring finger axis and 5.5 mm in the long-ring interspace axis. These and other more subtle anatomical observations indicate the greater safety of using the ring finger axis for endoscopic carpal tunnel release.
Surgical Technique
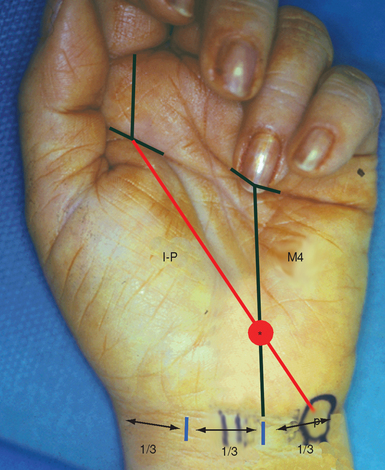
The landmarks to localize the hook of the hamate are as follows.8,9 First, the pisiform is palpated and marked. A second mark is placed on the proximal palmar skin crease, in line with the mid portion of the index finger. These two points are then connected, forming the index-pisiform line. A second line is drawn from the midpoint of the base of the ring finger, proximally to the wrist crease at the junction of its middle and ulnar third—forming the fourth metacarpal line. The intersection of the index-pisiform line and the fourth metacarpal line directly overlies the hook of the hamate (Figure 30.1). The palmar longus tendon (if present) is traced. The dissection should stay medial to the PL, which protects the median nerve.
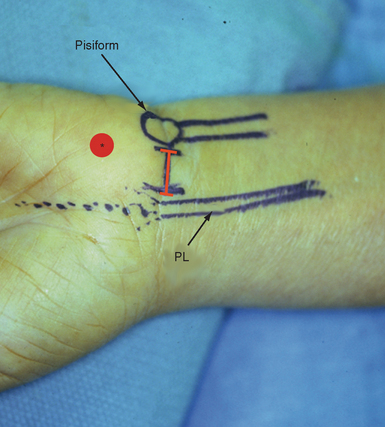
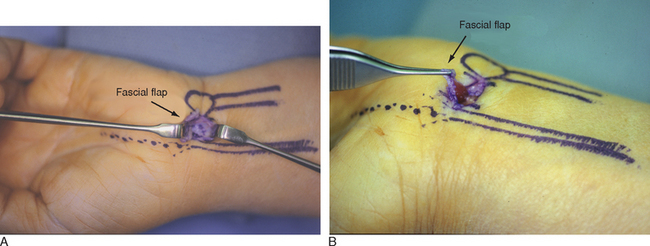
A 2-cm transverse incision is placed in the proximal wrist crease between the PL and pisiform. As the surgeon’s comfort level increases, this incision can be placed in the distal wrist crease—although there is more subcutaneous fat to contend with (Figure 30.2). The plane between the subcutaneous fat and the deep forearm fascia or flexor retinaculum is identified and developed. A distally based U-shaped flap of the flexor retinaculum is elevated by making two parallel incisions approximately 1 cm apart and 1 to 2 cm long through the deep fascia between the FCU and PL/median nerve (Figure 30.3A). The incisions are then connected by a proximal transverse cut. Care is taken to avoid penetration of the underlying flexor synovium to lessen inadvertent tendon laceration. The distally based flap is elevated (Figure 30.3b) while developing the plane between the FDS tendons and the undersurface of the TCL. Establishing this plane is integral to proper scope placement.
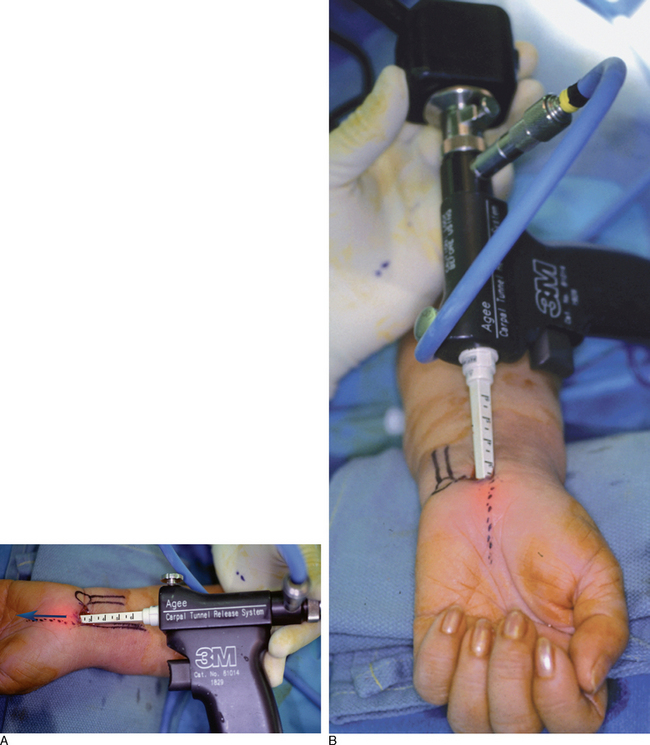
The wrist is then hyperextended over two folded towels. A small dilator is gently inserted, superficial to the plane of the flexor tendons but underneath the TCL—keeping it aligned with the ring metacarpal line and radial to the hamate hook. With proper placement, the dilator will abut against the hook of the hamate when sweeping it in an ulnar direction. If there is an obstruction to ulnar passage of the dilator, it should be removed and reinserted. Otherwise, there is a risk of grievous injury to the ulnar nerve and artery.
A larger dilator is next inserted to enlarge the gliding path for the scope. The distal tip of the dilators can be easily palpated in the midpalm by levering the tip anteriorly. Multiple passes of the dilators increases the risk of a median neuropraxia, especially in small wrists, and should be avoided. The soft-tissue elevator is then inserted and used to gently scrape any synovium from the undersurface of the TCL. While keeping the wrist hyperextended, the tip of the Agee endoscope is then gently inserted into the canal. The surface line marking the axis of the ring finger is used as a guide (Figure 30.4 and b).
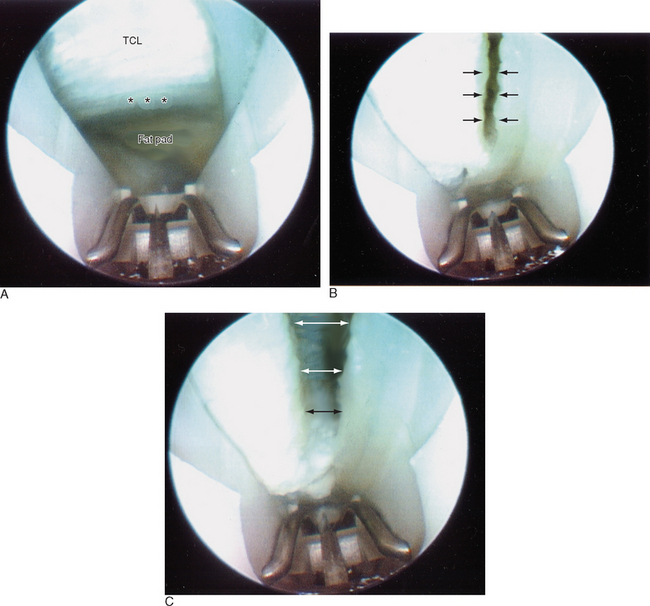
At this point, the shiny transverse fibers of the undersurface of the TCL should be visualized. Often, fogging of the scope, fluid from fatty tissue, or synovial remnants will block the view. In this event, the scope should be removed and defogged and the synovial elevator used once more. Because the scope is often colder than the carpal canal, keeping the scope in warm water until just before use may minimize the fogging. The distal edge of the TCL must be completely visualized (Figure 30.5a). This can be identified by a change of the transverse fibers to an ill-defined fat pad, which contains the superficial palmar arch and the common digital branch to the third web space.
Ballottement of the fat pad can aid in the demarcation zone. The hook blade should not be engaged until the distal edge is well seen. It is prudent to start the blade 2 to 3 mm from the distal edge on the first pass (Figure 30.5b). The hook blade is then maintained upright while the scope is slowly withdrawn proximally, keeping the blade in sight at all times. The scope is then reinserted to visualize the cut. The TCL is under tension and will usually split apart, allowing identification of the muscle fibers of the overlying palmar brevis or the longitudinally oriented fibers of the palmar aponeurosis. A second pass may be made at this point to release the distal-most fibers of the TCL (Figure 30.5c). The scope is then removed.
It is possible for the mesoneural tissue surrounding the median nerve to become interposed between the scope and the undersurface of the TCL. It will not have the appearance of nerve tissue and can be drawn in by the hook blade, which may lead to a partial or complete median nerve laceration. If there is any doubt, the scope should be removed and the field cleared. If the view cannot be improved, conversion to an open procedure is necessary. The wound is infiltrated with Marcaine and closed with an absorbable subcuticular suture and Steri-Strips.
Complications
There have been significant and devastating complications reported, which are often related to poor scope placement or inadequate visualization of the TCL. This includes partial and complete median nerve lacerations, common digital nerve lacerations, and injuries to the superficial palmar arch.10 The author has noted a neurapraxia of the third common digital nerve branch in small women patients with small carpal canals that has lasted up to six months. Flexor tendon lacerations have also been reported. If there is anything less than complete visualization, the procedure should be converted to an open CTR. Placing the scope in Guyon’s canal due to inadequate identification of the hook of the hamate has resulted in ulnar nerve and artery lacerations.11 Incomplete release of the TCL is commonly reported and is a major criticism of this technique.12,13
Results
Controversy continues to dog any method of ECTR. Advocates proclaim less postoperative pain, quicker recovery of grip strength, and a faster return to work.14–16 Critics cite the higher occurrence of incomplete release of the transverse carpal ligament, disturbing reports of neurovascular injury, and a similar incidence of pillar pain.10,17–22 Agee et al. carried out a 10-center randomized prospective multicenter study of endoscopic release using his technique. There were 122 patients in the study. Twenty-five had carpal tunnel surgery on both hands and 97 had surgery on one hand. Of the surgical procedures, 65 were in the control group and 82 were in the device group.
For patients in the device group with one affected hand, the median time for return to work was 21.5 days less than that for the control group. Another large multicenter prospective study of 192 cases demonstrated at least in the short term that the patients treated with the endoscopic method had significantly greater grip strength, pinch strength, and hand dexterity. The open technique resulted in greater scar tenderness during the first three months after surgery, as well as a longer time until the patients could return to work.23
Everyone is not in agreement on this point, though. In a small study of 25 patients with bilateral carpal tunnel syndrome who underwent an endoscopic release by the Agee technique on one hand and open release on the other, the investigators found no significant advantages in terms of return of grip strength, manual dexterity, or sensation.22 Foucher et al. examined his initial experience with this technique in 95 hands at 4.5 years.24 Seventy-two percent of hands were free of symptoms and 94% were described by the patients as functionally normal. Seventeen hands (out of 27) with residual or recurrent symptoms were examined. Nine hands (nine patients) were only partially improved (mean 6.7 on a 10-point scale) and in eight hands (seven patients) some symptoms had recurred after a mean delay of 3.8 years.
One utility of the endoscopic method is the ability to perform simultaneous bilateral CTR without significantly increasing patient morbidity.25 This, however, has been replicated with simultaneous bilateral open release as well.26,27
1 Chow JC. Endoscopic release of the carpal ligament: A new technique for carpal tunnel syndrome. Arthroscopy. 1989;5:19-24.
2 Agee JM, McCarroll HRJr., Tortosa RD, et al. Endoscopic release of the carpal tunnel: A randomized prospective multicenter study. J Hand Surg [Am]. 1992;17:987-995.
3 Wheatley MJ, Hall JW, Pratt D, Faringer PD. Is training in endoscopic carpal tunnel release appropriate for residents? Ann Plast Surg. 1996;37:254-257.
4 Teoh LC, Tan PL. Endoscopic carpal tunnel release for recurrent carpal tunnel syndrome after previous open release. Hand Surg. 2004;9:235-239.
5 Cobb TK, Dalley BK, Posteraro RH, Lewis RC. Anatomy of the flexor retinaculum. J Hand Surg [Am]. 1993;18:91-99.
6 Cobb TK, Carmichael SW, Cooney WP. The ulnar neurovascular bundle at the wrist: A technical note on endoscopic carpal tunnel release. J Hand Surg [Br]. 1994;19:24-26.
7 Rotman MB, Manske PR. Anatomic relationships of an endoscopic carpal tunnel device to surrounding structures. J Hand Surg [Am]. 1993;18:442-450.
8 Cobb TK, Cooney WP, An KN. Clinical location of hook of hamate: A technical note for endoscopic carpal tunnel release. J Hand Surg [Am]. 1994;19:516-518.
9 Cobb TK, Knudson GA, Cooney WP. The use of topographical landmarks to improve the outcome of Agee endoscopic carpal tunnel release. Arthroscopy. 1995;11:165-172.
10 Murphy RXJr., Jennings JF, Wukich DK. Major neurovascular complications of endoscopic carpal tunnel release. J Hand Surg [Am]. 1994;19:114-118.
11 Luallin SR, Toby EB. Incidental Guyon’s canal release during attempted endoscopic carpal tunnel release: An anatomical study and report of two cases. Arthroscopy. 1993;9:382-386. discussion 81
12 Varitimidis SE, Herndon JH, Sotereanos DG. Failed endoscopic carpal tunnel release: Operative findings and results of open revision surgery. J Hand Surg [Br]. 1999;24:465-467.
13 Hulsizer DL, Staebler MP, Weiss AP, Akelman E. The results of revision carpal tunnel release following previous open versus endoscopic surgery. J Hand Surg [Am]. 1998;23:865-869.
14 Atroshi I, Larsson GU, Ornstein E, et al. Outcomes of endoscopic surgery compared with open surgery for carpal tunnel syndrome among employed patients: Randomised controlled trial. BMJ. 2006;332(7556):1473.
15 Futami T. Surgery for bilateral carpal tunnel syndrome: Endoscopic and open release compared in 10 patients. Acta Orthop Scand. 1995;66:153-155.
16 Jimenez DF, Gibbs SR, Clapper AT. Endoscopic treatment of carpal tunnel syndrome: A critical review. J Neurosurg. 1998;88:817-826.
17 Ecker HAJr. Persistent or recurrent carpal tunnel surgery following prior endoscopic carpal tunnel release. J Hand Surg [Am]. 1999;24:647-648.
18 Forman DL, Watson HK, Caulfield KA, et al. Persistent or recurrent carpal tunnel syndrome following prior endoscopic carpal tunnel release. J Hand Surg [Am]. 1998;23:1010-1014.
19 Ludlow KS, Merla JL, Cox JA, Hurst LN. Pillar pain as a postoperative complication of carpal tunnel release: A review of the literature. J Hand Ther. 1997;10:277-282.
20 Nath RK, Mackinnon SE, Weeks PM. Ulnar nerve transection as a complication of two-portal endoscopic carpal tunnel release: A case report. J Hand Surg [Am]. 1993;18:896-898.
21 Wheatley MJ, Kaul MP. Recurrent carpal tunnel syndrome following endoscopic carpal tunnel release: A preliminary report. Ann Plast Surg. 1997;39:469-471.
22 Schonauer F, Varma S, Belcher HJ. Endoscopic carpal tunnel release: Practice in evolution. Scand J Plast Reconstr Surg Hand Surg. 2003;37:360-364.
23 Trumble TE, Diao E, Abrams RA, Gilbert-Anderson MM. Single-portal endoscopic carpal tunnel release compared with open release: A prospective, randomized trial. J Bone Joint Surg Am. 2002;84-A:1107-1115.
24 Erhard L, Ozalp T, Citron N, Foucher G. Carpal tunnel release by the Agee endoscopic technique: Results at 4 year follow-up. J Hand Surg [Br]. 1999;24:583-585.
25 Fehringer EV, Tiedeman JJ, Dobler K, McCarthy JA. Bilateral endoscopic carpal tunnel releases: Simultaneous versus staged operative intervention. Arthroscopy. 2002;18:316-321.
26 Wang AA, Hutchinson DT, Vanderhooft JE. Bilateral simultaneous open carpal tunnel release: A prospective study of postoperative activities of daily living and patient satisfaction. J Hand Surg [Am]. 2003;28:845-848.
27 Weber RA, Boyer KM. Consecutive versus simultaneous bilateral carpal tunnel release. Ann Plast Surg. 2005;54:15-19.