19 Aesthetic Principles and Consultation
Minimally invasive aesthetic procedures have become the treatments of choice for rejuvenation of aging skin and facial enhancement.1 Since approval of botulinum toxin, dermal fillers, and lasers by the Food and Drug Administration (FDA) for cosmetic use, there has been a shift away from more traditional invasive surgical procedures that may radically alter appearance toward procedures that can enhance appearance in more natural and subtle ways. According to statistics from the American Society for Aesthetic Plastic Surgery, over 10 million aesthetic procedures are performed in the United States and more than 80% are minimally invasive.2 The most commonly performed procedures include onabotulinumtoxinA (Botox; formerly known as botulinum toxin type A) and dermal filler injections for treatment of wrinkles; lasers and intense pulsed light technologies for hair reduction, skin resurfacing, and photorejuvenation; and chemical peels and microdermabrasion for exfoliation.
These aesthetic procedures are associated with high patient and provider satisfaction because they are efficacious, have low risks of side effects, involve minimal patient discomfort with short recovery times, and can be safely performed in the office setting.3,4 As the popularity and demand for minimally invasive aesthetic procedures continues to grow, more health care providers are choosing to incorporate these types of treatments into their practice. This introduction to the aesthetic section of the book presents basic aesthetic principles for providers who wish to get started with aesthetic medicine. The succeeding chapters demonstrate the most commonly performed aesthetic procedures that can be readily incorporated into office practice.
Facial Aging
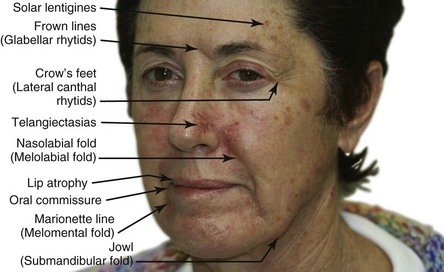
Facial aging is associated with a gradual thinning of the skin and loss of elasticity over time accompanied by the diminishment of dermal collagen, hyaluronic acid, and elastin. Ultraviolet (UV) radiation from sun exposure accelerates this process at a higher rate than does chronologic aging. This UV aging process is termed photoaging. To appreciate the contribution of photoaging to the appearance of aged skin, one needs only compare photoprotected skin, such as skin on the inside of the upper forearm or under the chin, to the appearance and texture of skin on face and back of the hands. Photoaged skin typically exhibits the following changes (Figure 19-1 for a computer-enhanced image demonstrating these signs)5:
In a study by New York plastic surgeon Dr. D. Antell on aging in identical twins, extrinsic factors, such as prolonged sun exposure, resulted in advanced aging changes (Figure 19-2A) relative to the intrinsic aging seen in non–sun-exposed twins (Figure 19-2B).6 Habitual facial expressions also contribute to formation of visible lines and wrinkles, particularly in the upper one-third of the face, because repetitive muscle contractions etch in frown lines between eyebrows and crow’s feet radiating from the corner of the eyes. In addition to skin laxity, volume loss, and dynamic musculature, facial aging also results from biometric facial changes such as descent of malar fat pads, which contributes to deepened nasolabial folds, and resorption of maxillary and mandibular bone, which contributes to radial lip lines and mental crease formation.7,8
Skin Anatomy
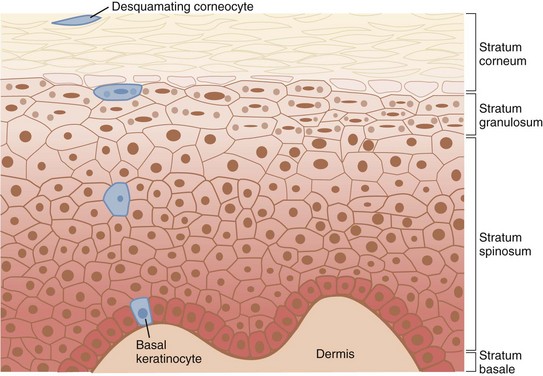
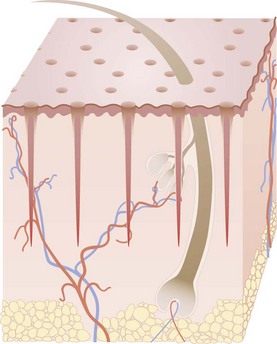
The skin is divided into three layers: the epidermis, dermis, and hypodermis or subcutaneous layer (Figure 19-3). The epidermis is the top layer of the skin and is composed of four cell types: keratinocytes, melanocytes, Langerhans cells, and Merkel cells. The epidermis is further divided into the outermost nonliving layer, the stratum corneum, and the living cellular layers of the stratum granulosum, stratum spinosum, and stratum basale.
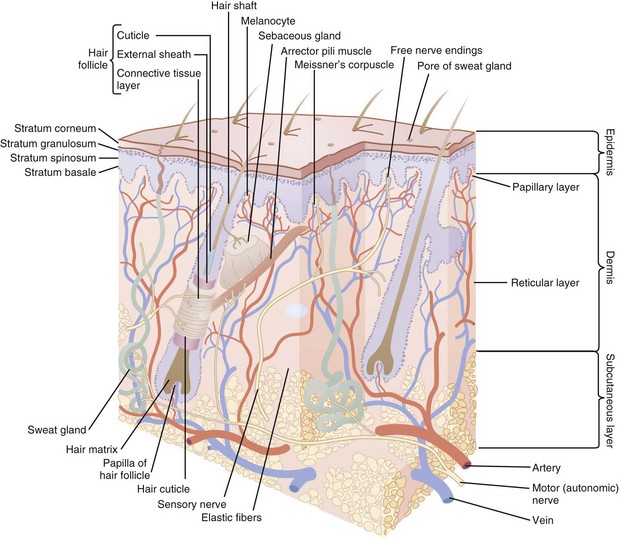
FIGURE 19-3 Skin anatomy.
(Modified from White CR, Bigby M, Sangueza OP. What is normal skin? In: Arndt KA, LeBoit PE, Robinson JK, Wintroub BU, eds., Cutaneous Medicine and Surgery. Philadelphia: Saunders; 1996:3–41.)
The stratum corneum is composed of corneocytes and lipids, which serves as a barrier against microbial pathogens and environmental irritants and also keeps the skin hydrated and protected from injury. Constant renewal is necessary for the epidermis to maintain its integrity and function effectively. In healthy young skin, it takes approximately 1 month for keratinocytes to migrate from the living basal layer of the epidermis to the stratum corneum surface and desquamate, during the process of epidermal renewal. Figure 19-4 shows the structure of the epidermis with the keratinocyte maturation highlighted. Photoaged skin demonstrates slower keratinocyte maturation and abnormal retention of cells in the epidermis. This results in a rough and thickened stratum corneum with impaired barrier function, reduced hydration capabilities, and increased pigmentation from retention of melanin-laden keratinocytes in the epidermis.
The distribution of melanin within the epidermis determines skin coloration. While the number of melanocytes is similar for both light and dark skin types, melanin is concentrated in small aggregated melanosomes in light skin and is more disbursed in darker skin.9
Aesthetic Consultation
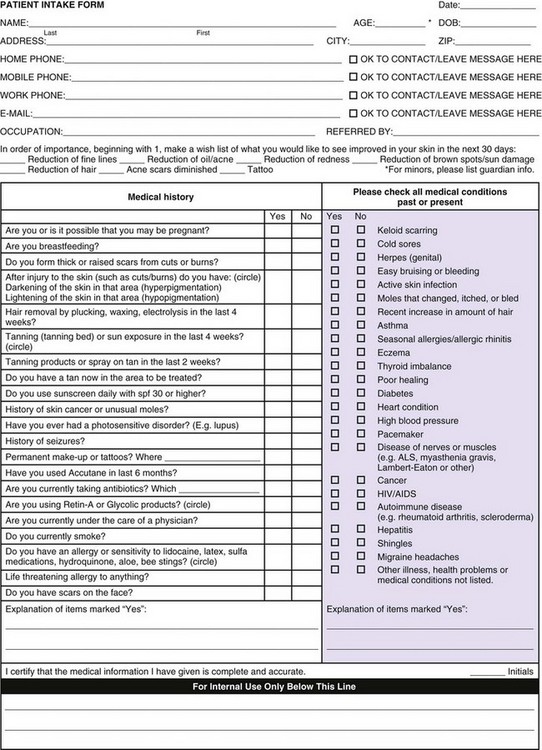
Aesthetic consultation is an important part of successfully performing aesthetic treatments. The patient’s medical history is reviewed, including past medical history, medications, allergies, and past cosmetic history (including results from previous treatments and side effects if any, surgeries, and satisfaction with outcomes). Figure 19-5 is an example of an aesthetic intake form that clinicians may use. Repeated dissatisfaction with past aesthetic treatments can be associated with unrealistic expectations or body dysmorphic disorder and is a contraindication to treatment.
The main areas of concern should be determined and prioritized by the patient at the time of consultation. It is recommended that the patient view these areas using a handheld mirror, so that the provider and patient may simultaneously examine the desired treatment areas. Asymmetries, such as uneven eyebrow height, are pointed out to the patient, noted in the chart, and photographed.10 Pigmented lesions in the treatment area are evaluated and lesions suspected of melanoma biopsied with results reviewed prior to proceeding with treatments.
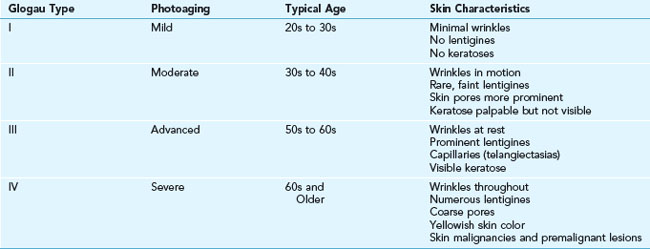
Glogau Classification of Photoaging
The Glogau classification system was developed to assess the severity of photoaging, especially with regard to wrinkles (see Table 19-1). It is used as a baseline measure at the time of aesthetic consultation and may be used as a gross guide to therapy. In general, Glogau types I, II, and III tend to show the most noticeable improvements with less aggressive minimally invasive aesthetic treatments such as botulinum toxin and dermal filler injections, nonablative lasers, superficial and fractional ablative lasers, and superficial skin resurfacing procedures such as light chemical peels and microdermabrasion. Glogau type IV patients often require deep ablative laser treatments and/or surgery for significant results.
Fitzpatrick Skin Types
The Fitzpatrick skin type classification was developed to categorize a skin color and response to sunlight exposure. Skin types I, II, and III are white or Caucasian; types IV and V have olive skin tones, as seen in persons of Mediterranean, Asian, and Latin descent; and type VI is black, often of African American descent (see Table 19-2).11 Fitzpatrick skin type may be used as a guide to the type and aggressiveness of aesthetic treatments, and may grossly predict skin response to treatments. For example, patients with Fitzpatrick skin types I, II, and III can generally tolerate aggressive treatments and have low risks of pigmentary changes. Patients with darker Fitzpatrick skin types (types IV through VI) have greater risks of pigmentary alterations, such as hyperpigmentation and hypopigmentation and require more conservative treatments to minimize the likelihood of these complications.
|
Fitzpatrick Skin Type |
Characteristics |
Response to Sun Exposure |
|---|---|---|
| I |
Photodocumentation
Photodocumentation, where photographs are used to demonstrate clinical findings, is an essential component of aesthetic treatments both for the patient’s reference and for medical-legal purposes.12 Photographs prior to treatment, midway through a series of treatments, and post-treatment are helpful and recommended. Consent for photographs is typically included in the procedure consent form and obtained prior to taking photographs. Recommended photographs include the full face and specific treatment areas which are photographed from the front, 45 and 90 degrees while the patient is positioned fully upright looking straight ahead. For injection treatments, photographs are taken with the face at rest and with active facial movement of the treatment areas. There are commercial photographic systems available that provide standardized angles and lighting to facilitate consistent photography.
Informed Consent
Patients seeking elective aesthetic treatments typically have high expectations of treatment outcomes and low tolerance for side effects. It is recommended that all aspects of the informed consent process be addressed13:
Laser Treatment Principles
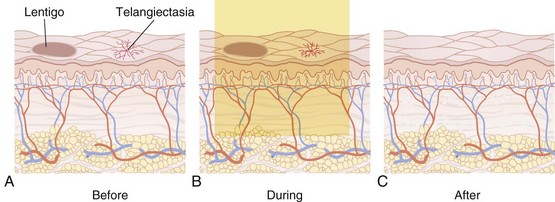
Laser* devices produce monochromatic light of a single wavelength that is highly focused in a collimated beam (defined as parallel rays of light that disperse minimally). Intense pulsed light (IPL) devices emit a spectrum of wavelengths and employ filters to refine the energy output. Treatments with lasers and IPL devices (collectively referred to as lasers in this book) are based on the principle of selective photothermolysis. According to this principle, light of a specific wavelength is selectively absorbed by the “undesired” target in the skin such as a solar lentigo; the target is heated, damaged, and eliminated, while the surrounding skin is left unaffected. Figure 19-6 illustrates the principle of selective photothermolysis with treatment of solar lentigines and telangiectasias.14
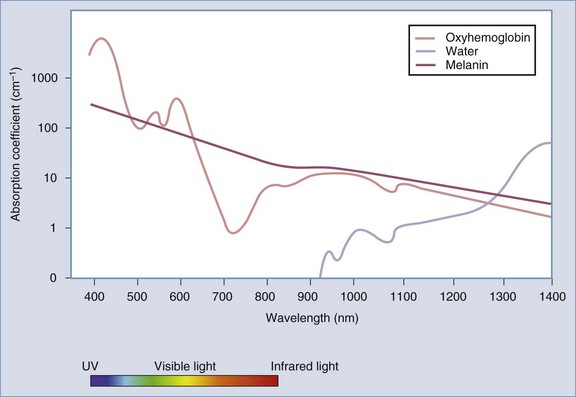
When laser energy impacts skin, the beam may be absorbed, reflected, transmitted, or scattered. All four interactions occur to some degree, but absorption is the most important clinically. The degree of absorption depends on the chromophores, or light-absorbing substances, in skin. The primary chromophores in skin are melanin, oxyhemoglobin, and water, and each has a unique wavelength absorption spectrum (Figure 19-7). Treatment wavelengths are selected such that they are absorbed better by the target chromophores than by chromophores in the surrounding skin. Target chromophores for laser treatments are shown in Table 19-3.
| Treatment | Chromophore |
| Hair reduction | Melanin |
| Photorejuvenation: | |
| Pigmented lesions Red vascular lesions |
Melanin Oxyhemoglobin |
| Tattoos | Tattoo ink |
| Wrinkle reduction | Water |
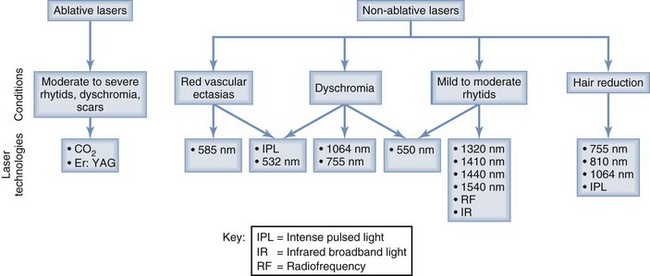
Figure 19-8 summarizes lasers commonly used for treatment of aesthetic conditions including: dyschromia, vascular ectasias, rhytids, and hair reduction.
Laser Parameters
To achieve efficacious treatments with maximal safety, the provider must have an understanding of basic laser parameters, as well as the properties of the targets being treated in the skin. Laser parameter definitions and key concepts are summarized below15:
A typical laser is shown in Figure 19-9 with its component parts, including a computerized touch screen commonly used to select laser parameters, a laser handpiece and distance guide.
Fractional Lasers
“Fractional” refers to a method of laser energy delivery, it does not refer to a particular wavelength. Fractional devices deliver laser energy in microscopic columns, called microthermal zones (Figure 19-10). The two main types of fractional laser devices are ablative (e.g., CO2 and Er:YAG) and nonablative (e.g., 1550 and 1410 nm). Most fractional devices are used for skin resurfacing to reduce wrinkles and improve dyschromia. Only a portion of the skin is treated with this fractional method of delivery, resulting in significantly shortened recovery times particularly for ablative lasers.
Laser Safety
When using lasers, a laser safety officer should be designated, the American National Standards Institute (ANSI) laser safety requirements met,16–18 and specific device manufacturer’s guidelines for safety and maintenance follow. Wavelength-specific eyewear must be worn to protect patients and providers from ocular injury. Mirrors and windows are covered, laser warning signs posted, and a laser safety checklist reviewed prior to performing each treatment.
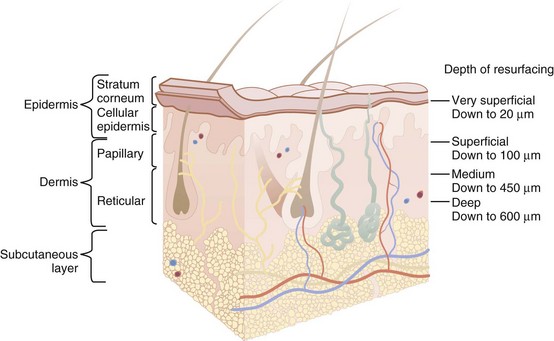
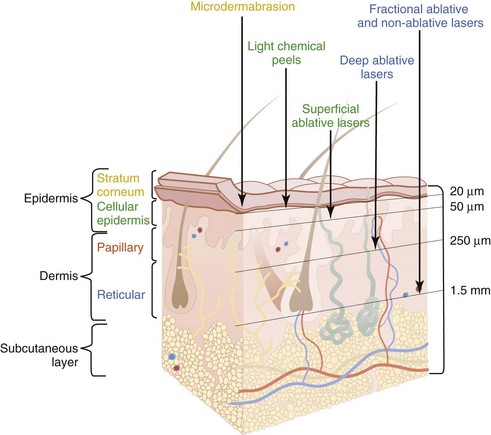
Skin Resurfacing
Skin resurfacing can be performed to varying degrees of aggressiveness based on the depth of skin penetration. Figure 19-11 shows standard definitions for very superficial (stratum corneum), superficial (typically to the base of the epidermis, but may include the upper papillary dermis), medium (upper reticular dermis), and deep (midreticular dermis) skin resurfacing. Figure 19-12 illustrates the typical depths achieved with different resurfacing procedures. In general, the greater the depth of wounding, the more dramatic the results achieved. However, greater wound depths are also associated with longer recovery time, more intensive postprocedure care, and greater risks of side effects and complications. Penetration into or below the papillary dermis, which is usually associated with bleeding, has a greater risk of scarring than more superficial resurfacing of the epidermis.
Aesthetic Procedures: Getting Started
1. Small R. Aesthetic procedures in office practice. Am Fam Physician. 2009;80(11):1231-1237.
2. Cosmetic Surgery National Data Bank 2010 statistics. American Society for Aesthetic Plastic Surgery, 2010.
3. de Maio M. The minimal approach: an innovation in facial cosmetic procedures. Aesthetic Plast Surg. 2004;28:295-300.
4. Sommer B, Zschocke I, Bergfeld D, et al. Satisfaction of patients after treatment with botulinum toxin for dynamic facial lines. Derm Surg. 2003;29(5):456-460.
5. Lockman AR, Lockman DW. Skin changes in the maturing woman. Clin Fam Pract. 2002;4(1):113-134.
6. Antell D. How environment and lifestyle choices influence the aging process. Ann Plast Surg. 2009;43(6):585-588.
7. Zimbler MS, Kokoska MS, Thomas JR. Anatomy and pathophysiology of facial aging. Facial Plast Surg Clin North Am. 2001;9(2):179-187. vii
8. Werschler P. Combining advanced injection techniques: Integrating new therapies into clinical practice. Cosmetic Dermatol. 2008;21(2 S1):3-6.
9. Szabo G, Gerald AB, Pathak MA, et al. Racial differences in the fate of melanosomes in human epidermis. Nature. 1969;222(5198):1081-1082.
10. Small R. Aesthetic procedures introduction. In: Mayeaux E, editor. The Essential Guide to Primary Care Procedures. Philadelphia: Lippincott Williams & Wilkins; 2009:195-199.
11. Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1998;124(6):869-871.
12. Kuhnel T, Wolf S. Mirror system for photodocumentation in plastic and aesthetic surgery. Brit J Plast Surg. 2005;58(6):830-832.
13. Informed consent update, Claims Rx. Norcal Mutual Insurance Company. 2007.
14. Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524-527.
15. Levins P. Selective photothermolysis. In: Keller GS, Lacombe V, Lee P, Watson J, editors. Lasers in Aesthetic Surgery. New York: Thieme Medical Publishers; 2001:34-40.
16. American National Standards Institute. American National Standard for the Safe Use of Lasers. Z136.1–2007.
17. American National Standards Institute. American National Standard for the Safe Use of Lasers in Health Care Facilities. Z136.3–2005.
18. Recommended practices for laser safety in practice setting. In: Perioperative Standards and Recommended Practices. Denver, CO: Association of Perioperative Registered Nurses; 2008:447-452.
Alibhai H. Introduction to aesthetic medicine. In Pfenninger JL, Fowler GC, editors: Pfenninger and Fowler’s Procedures for Primary Care, 3rd ed, Philadelphia: Mosby/Elsevier, 2010.
Small R, Hoang D. Botulinum toxin introduction and foundation concepts. In: Small R, Hoang D, editors. A Practical Guide to Botulinum Toxin Procedures. Philadelphia: Lippincott Williams & Wilkins, 2011.
Small R, Hoang D. Dermal filler introduction and foundation concepts. In: Small R, Hoang D, editors. A Practical Guide to Dermal Filler Procedures. Philadelphia: Lippincott Williams & Wilkins, 2011.
Small R, Linder J. Skin care introduction and foundation concepts. In: Small R, Linder J, editors. A Practical Guide to Skin Care Procedures and Products. Philadelphia: Lippincott Williams & Wilkins, 2011.
Small R. Laser introduction and foundation concepts. In: Small R, editor. A Practical Guide to Cosmetic Lasers. Philadelphia: Lippincott Williams & Wilkins, 2012.