Aerosol and Humidity Therapy
I Stability: Stability is the tendency of aerosol particles to remain in suspension. The following factors affect the stability of an aerosol.
A Size: The smaller the aerosol particle, the greater the tendency toward stability. The larger the particle, the greater its tendency to rain out of suspension.
B Concentration: The greater the concentration of particles, the greater the tendency for individual particles to coalesce into larger particles and rain out of suspension.
C Humidity: The greater the relative humidity of the gas carrying the aerosol, the greater the stability of the aerosol.
II Penetration and Deposition of an Aerosol in the Respiratory Tract
A Penetration refers to the depth within the respiratory tract that an aerosol reaches.
B Deposition is the rain-out of aerosol particles within the respiratory tract.
C Depth of penetration and volume of deposition depend on
1. Gravity: Gravity decreases penetration and increases premature deposition but has minimal effect on aerosol particles in the therapeutic range of 1 to 5 μm (Table 35-1).
TABLE 35-1
Penetration and Deposition Versus Particle Size
| Particle Size (μ m) | Deposition in Respiratory Tract |
| >100 | Do not enter respiratory tract |
| 100-10 | Trapped in mouth |
| 100-5 | Trapped in nose |
| 5-2 | Deposited proximal to alveoli |
| 2-1 | Can enter alveoli, 95-100% of particles 1 mu;m in size settling |
| <1-0.25 | Stable, with minimal settling |
2. Kinetic energy: The greater the kinetic energy of the gas carrying the particles, the greater the tendency for premature deposition. This is because coalescence and impaction are increased.
3. Inertial impaction: Deposition of particles is increased at any point of directional change or increased airway resistance. Thus the smaller the airway diameter, the greater the tendency for deposition.
III Ventilatory Pattern for Optimal Penetration and Deposition
A The patient’s ventilatory pattern is the most important variable that can be controlled to ensure maximum penetration and deposition of aerosol particles during aerosol treatments.
1. Large, slowly inspired tidal volume (Vt) over 3 to 4 seconds except with dry powder aerosols. Dry powder aerosols require a fast inspiratory flow rate.
2. After inhalation a 3- to 4-second breath-holding period is advisable to ensure maximum deposition.
3. With large-volume aerosols (ultrasonic nebulizers) a face mask should be used.
4. Exhalation should be relaxed and normal.
5. Coughing should be encouraged if secretion mobilization occurs and at the completion of treatment.
C Attempts should be made to have all patients receiving aerosol therapy assume the described ventilatory pattern.
Inhaled particles are removed from the respiratory tract by three mechanisms.
A Primary mechanism: Mucociliary escalator, which moves approximately 100 ml of secretions to the oropharynx per day.
V Indications for Aerosol Therapy
A Bland aerosol administration is the delivery of aerosolized sterile water and isotonic or hypertonic saline.
1. Indications (Modified from AARC Clinical Practice Guideline: Bland aerosol administration, 2003)
a. Presence of upper airway edema
e. Postoperative management of the upper airway
b. Bronchoconstriction when artificial airway is used
(1) May be a problem primarily with neonates and infants
(2) Associated more frequently with the use of ultrasonic nebulizers than with the use of jet nebulizers
g. Edema is associated with decreased compliance and gas exchange and with increased airway resistance
B Indications for medicated aerosol administration are the need to deliver bronchodilators, antibiotics, or other pharmacologic agents in aerosol form to the lung parenchyma.
VI General Goals of Aerosol Therapy
1. Improve efficiency of cough mechanism
2. Restore and maintain normal function of mucociliary escalator
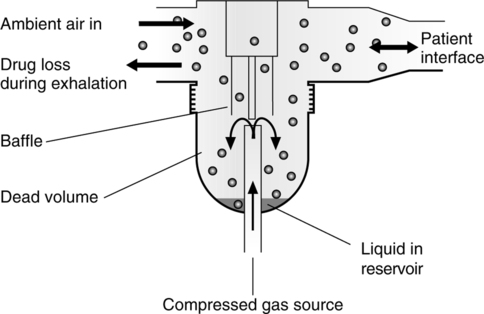
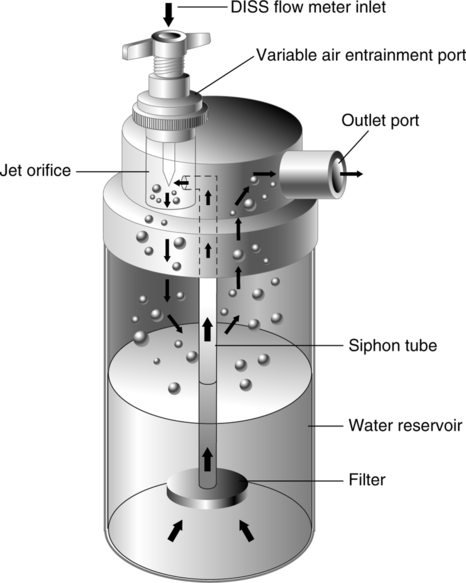
B Humidify gases delivered to patients with artificial airways (large volume nebulizer; Figure 35-1). Aerosol delivered to patients with artificial airways should be heated.
C Deliver medications by small volume nebulizer (SVN), metered dose inhaler (MDI), or dry powder inhaler (DPI)
VII Jet Aerosol Generators (Gas Powered)
A These generators use jet mixing to produce an aerosol and entrain a second gas.
B A system of baffles is used to impact large particles out of suspension.
C These generators are commonly used for delivery of medications (SVNs) and for humidification of inspired gases (large volume nebulizers).
VIII Aerosol Generators to Deliver Medications
A Small volume (jet) nebulizer (Figure 35-2)
1. Does not require patient coordination
2. A mouthpiece or face mask may be used.
3. Able to deliver high doses of medication
4. The amount of drug nebulized increases as the fill volume increases. A fill volume of 4 ml is recommended.
5. Generally the higher the flow to the nebulizer, the smaller the particle size generated; 6 to 8 L/min is recommended.
6. May be powered by oxygen or compressed air
7. SVNs are inconvenient to use outside the hospital environment and not portable.
8. Bacterial contamination of the SVN is common.
9. SVNs are usually used to administer aerosolized medications to infants and young children or to administer medications not available in MDIs.
10. SVNs may be used to deliver aerosolized medications during mechanical ventilation.
a. Proper technique for aerosol delivery by SVN during mechanical ventilation
(1) Fill the nebulizer with the drug and diluent to the optimal fill volume, 4 to 6 ml.
(2) Place the nebulizer in the inspiratory limb of the circuit at least 30 cm from the patient’s Y piece.
(3) Attach the nebulizer tubing to the nebulizer outlet on the ventilator or to an external source of gas flow.
(4) Ensure that the flow through the nebulizer is 6 to 8 L/min.
(5) Ensure that the Vt is sufficient (≥500 ml in adults).
(6) If necessary adjust the delivered minute volume, trigger sensitivity, flow, and alarms to compensate for the additional flow through the nebulizer. In pediatric ventilators the additional flow may cause an increase in airway pressure or positive end-expiratory pressure and/or expiratory retard.
(7) Turn off the continuous flow on the ventilator, and remove or bypass the heat and moisture exchanger (HME) if present.
(8) Check the nebulizer for adequate aerosol generation.
(9) Disconnect the nebulizer when no more aerosol is produced.
(10) Reconnect the ventilator circuit, and reset to the original ventilator and alarm settings.
(11) Rinse the nebulizer with sterile water, let air dry, and store aseptically. To minimize bacterial contamination it is recommended that SVNs be changed at least every 24 hours.
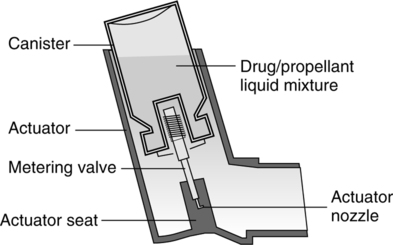
B Metered dose inhaler (Figure 35-3)
1. The MDI is the most common method used to deliver medication aerosols because it is convenient, portable, and less expensive.
2. The MDI is used to administer bronchodilators, anticholinergics, antiinflammatory agents, and steroids.
3. Proper use requires patient coordination.
4. It consists of a canister containing the drug, propellants, and an actuator.
5. Chlorofluorocarbon propellants have been used. More recently hydrofluoroalkene propellants are used because they are less harmful to the environment.
6. Effective use of the MDI depends on patient technique and coordination. Depending on technique, lung deposition in adults may vary between 10% and 25% of the nominal dose.
a. Proper technique for use of the MDI
(1) Warm the MDI canister to hand or body temperature.
(2) Insert canister into actuator, shake vigorously, and uncap the mouthpiece.
(3) When the MDI is new or has not been used recently, prime the metering chamber by actuating the MDI several times before use.
(4) Open mouth wide so tongue does not obstruct the mouthpiece.
(5) Hold the MDI vertically with the outlet aimed at the mouth.
(7) Place outlet either between the lips or approximately 4 cm (two fingers’ width) from the mouth.
(8) Breathe in slowly, and actuate the MDI just after the beginning of inspiration.
(9) Continue to inhale to total lung capacity (TLC).
(10) Hold breath for 4 to 10 seconds.
(11) Wait 30 seconds between actuations, and repeat until prescribed dose is administered.
7. An MDI may be used with a spacer or valved holding chamber to reduce oropharyngeal deposition of the drug, decrease the bad taste of some medications, and aid the patient with poor hand-breath coordination.
a. Spacers with masks may be used to administer aerosolized medications to small children.
b. Proper technique for use of an MDI with a spacer
(1) Warm the MDI canister to hand or body temperature.
(2) Shake vigorously, insert canister into actuator, and insert the actuator into the spacer.
(3) Place the spacer between lips and teeth, and close mouth around the mouthpiece of the spacer.
(5) One second later begin to inhale completely to TLC.
(6) Hold breath for 4 to 10 seconds.
(7) Repeat inhalation if Vt is small.
(8) Wait 30 seconds, and then repeat the process until prescribed dose is delivered.
c. A spacer should always be used with MDIs delivering steroids.
8. Bacterial contamination of the MDI is uncommon.
9. It is difficult to deliver high doses of medication with the MDI.
10. MDIs with an appropriate spacer can be used to administer aerosolized drugs into the inspiratory limb of a ventilator circuit.
a. Proper technique for use of an MDI during mechanical ventilation
(1) Decrease the inspiratory flow rate or extend the inspiratory time during administration.
(2) Ensure the ventilator breath is synchronous with the patient’s inspiration.
(3) Shake the MDI canister vigorously.
(4) Place the canister in the actuator of a cylindrical spacer placed in the inspiratory limb of the ventilator circuit.
(5) Actuate the MDI at the beginning of inspiration of a ventilator breath.
(6) Remove the canister, and shake between actuations.
(7) Wait 20 to 30 seconds between actuations, and repeat until prescribed dose is delivered.
(8) Remove canister from actuator in spacer, and close opening in spacer as indicated.
C Dry powder inhaler (Figure 35-4)
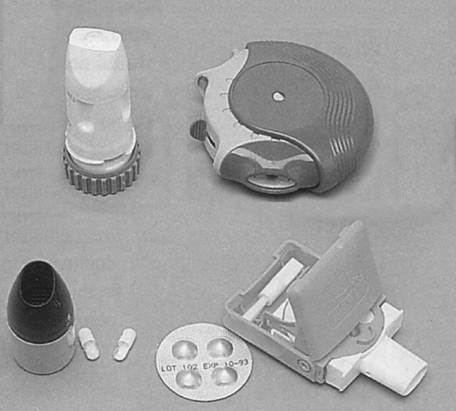
1. DPI is breath activated and requires some patient coordination.
2. DPI produces drug particles in the respirable range, 1 to 5 μm.
3. A fast inspiratory flow rate (>30 to 60 L/min) is required to deliver an effective dose.
4. There are four different types of DPIs: rotahaler, turbuhaler, diskus, and diskhaler.
5. DPIs should not be used for patients with acute bronchospasm or children aged <6 years.
D There are several types of special jet nebulizers commonly used for specific applications.
1. A vented breath-enhanced nebulizer is used to administer aerosolized antibiotics.
2. A valved nebulizer with an expiratory filter is used to administer pentamidine.
3. Nebulizers specifically made to provide continuous infusion of medications into the nebulizer are used for continuous aerosolized bronchodilator administration.
4. The small particle aerosol generator (SPAG) is only used to administer the drug ribavirin.
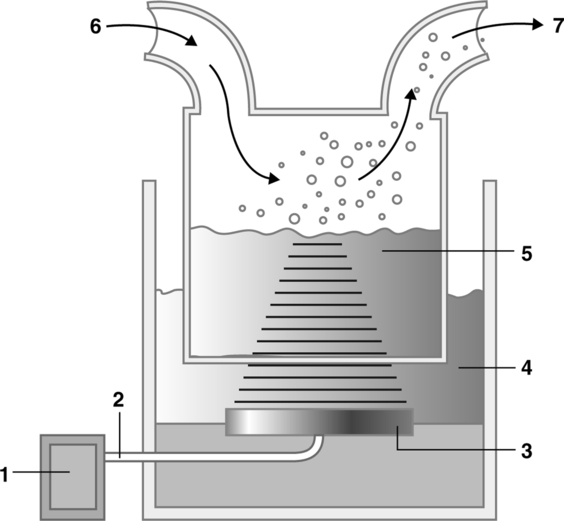
IX Ultrasonic Aerosol Generators (Electrically Powered)
A Ultrasonic nebulizers function by transforming standard household current into ultrasonic sound waves (Figure 35-5).
B The Federal Commerce Commission governs the frequency range (1 to 2 megacycles/sec) for ultrasonic sound waves of ultrasonic nebulizers. All ultrasonic nebulizers produced and sold in the United States have preset frequencies in this range.
C The ultrasonic sound waves are applied to a quartz crystal or ceramic disk, causing it to vibrate at the same frequency as the ultrasonic waves. This is referred to as the piezoelectric quality of the disk.
D The crystal or disk transfers its vibratory energy to the fluid to be nebulized, creating an aerosol.
E These nebulizers incorporate an amplitude control that varies the intensity of ultrasonic waves, allowing varying aerosol outputs.
F Ultrasonic nebulizers are used principally to deliver bland aerosols for sputum induction.
X Comparison of Nebulizer Output
XI Comparison of Nebulizer Particle Size
A Jet nebulizers: 55% of aerosol particles produced fall in the therapeutic range of 1 to 5 μm.
B Ultrasonic nebulizers: 97% of aerosol particles produced fall in the therapeutic range of 1 to 5 μm.
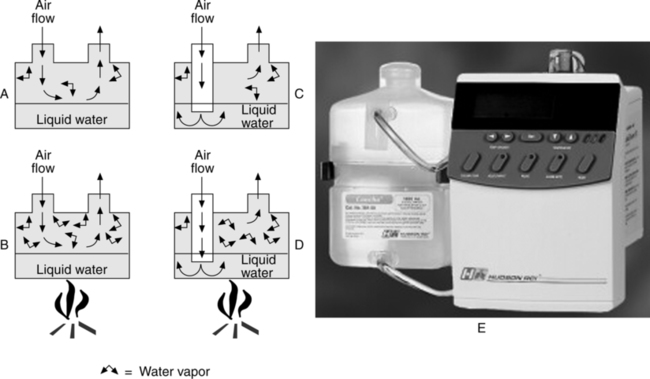
A A humidifier is designed to increase the water vapor content of a dry gas.
B There are two types of humidifiers.
C Generally three types of active humidifiers are used.
D Humidifiers also are either heated or unheated.
E Unheated bubble humidifiers may be used with simple oxygen therapy appliances.
1. These units are intended to bring dry gas to approximately 40% relative humidity at body temperature.
F Heated humidifiers are normally used during mechanical ventilation.
1. Bubble, passover, and wick humidifiers are available (Figure 35-6).
2. Systems are usually heated to achieve 34° C to 37° C and 100% relative humidity at the patient’s airway.
3. As a result of the temperature decrease as a gas moves from the humidifier to the patient, excess water vapor condenses in the tubing.
4. The use of heated ventilator circuits with some humidifier systems has greatly reduced condensate in circuits.
5. Hazards and complications of heated humidifiers (Modified from AARC Clinical Practice Guideline: Humidification During Mechanical Ventilation, 1992)
a. Potential for electrical shock
d. Thermal injury to the airway
e. Burns to the patient and tubing meltdown if heated-wire circuits are covered or circuits and humidifiers are incompatible
f. Underhydration and impaction of mucous secretions
g. Hypoventilation and/or alveolar gas trapping caused by mucous plugging of airways
h. Possible increased resistive work of breathing through the humidifier or because of mucous plugging of airways
i. Inadvertent overfilling resulting in unintentional tracheal lavage–heated reservoir humidifiers
j. When disconnected from the patient some ventilators generate a high flow through the patient circuit that may aerosolize contaminated condensate, putting the patient and clinician at risk for nosocomial infection.
k. Potential for burns to caregivers from hot metal
l. Inadvertent tracheal lavage from pooled condensate in patient circuit
m. Elevated airway pressures caused by pooled condensation
n. Patient-ventilator dyssynchrony and improper ventilator performance caused by pooled condensation in the circuit
G Humidifiers, either unheated or heated, may be used with noninvasive ventilators (bilevel positive airway pressure or continuous positive airway pressure) for patient comfort and to prevent drying of secretions.
XIII Heat and Moisture Exchangers (Artificial Noses)
A These devices sequester some or most of the water vapor exhaled by the patient. On the subsequent inspiration, the sequestered water is used to humidify the next inspiration.
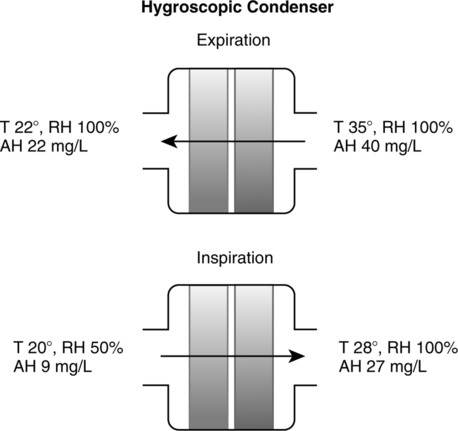
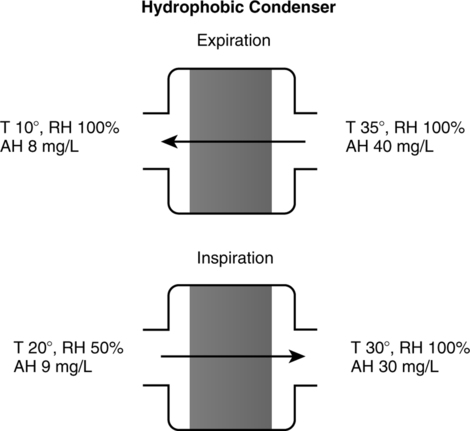
B Three types: Condenser humidifiers, hygroscopic condenser humidifiers (Figure 35-7), and hydrophobic condenser humidifiers.
C Condenser humidifiers usually are only 50% efficient.
D Hygroscopic condenser humidifiers are up to 70% efficient.
E Hydrophobic condenser humidifiers are approximately 70% efficient and are capable of filtering bacteria (Figure 35-8).
F HMEs are capable of maintaining adequate humidification for short-term (up to 72 hours) and periodic use (16 to 20 hr/day) in patients with chronic disease.
G Contraindications for HME use (Modified from AARC Clinical Practice Guideline: Humidification During Mechanical Ventilation, 1992)
1. Patients with thick, copious, or bloody secretions
2. Patients with an expired Vt <70% of the delivered Vt (e.g., those with large bronchopleurocutaneous fistulas or incompetent or absent endotracheal tube cuffs)
3. Patients with body temperature <32° C
4. Patients with high spontaneous minute volume (>10 L/min)
5. An HME must be removed from the patient circuit during aerosol treatments when the nebulizer is placed in the patient circuit.
H Hazards and complications of HME
1. Underhydration and impaction of mucous secretions
2. Hypoventilation and/or alveolar gas trapping caused by mucous plugging of airways
3. Possible increased resistive work of breathing through the HME or because of mucous plugging of airways
4. Possible hypoventilation caused by increased deadspace
5. Ineffective low pressure alarm during disconnection because of resistance through HME