CHAPTER 73 Adult Scoliosis
Adult scoliosis encompasses a broad spectrum of deformity in the mature spine. It can result from scoliosis in childhood or arise de novo from degenerative changes within the spinal motion segments. Scoliosis in the adult differs significantly and importantly from scoliosis affecting the child or adolescent. Important differences include curve types and patterns, rate of deformity progression, rigidity of deformity, patient comorbidities, and clinical symptoms and presentation. The differences between the adult and child with scoliosis lead to significant differences in the goals of care and strategies for treatment.1 In the child with scoliosis, the primary goal of care is to avoid the consequences of deformity progression. Adults with scoliosis characteristically present with pain, functional limitations, neural symptoms, and symptomatic deformity resulting in a measurable impairment on health-related quality of life. Improvement of present pain and disability is an important and measurable goal of treatment for adults with scoliosis. The value of care for adults with scoliosis may be measured quantifiably by a change in patient-reported quality of life measures.
Impact of Adult Scoliosis
Adult scoliosis is a common disorder of the spine with a wide variation in reported prevalence. The prevalence of scoliosis in adults has been estimated by population-based studies, and radiographic studies including DEXA scans and radiographic studies on populations that are representative of age-adjusted norms. Reported rates of scoliosis range from 1.4% to 68%.2–5 The source of variability is related to differences in definitions of scoliosis, methods of defining cohorts, sample size, and screening tools. Healey and Lane6 identified curves over 10 degrees in more than 50% of elderly females with back pain and osteoporosis. Robin and colleagues7 identified some degree of scoliosis in 70% of adults in a cohort of 554 patients between ages 50 and 84, with 30% of those having curves greater than 30 degrees. Ten percent of patients with a straight spine at enrollment developed a new onset of scoliosis during the 7- to 13-year follow-up period. More recently, Schwab and colleagues8 identified scoliosis of greater than 10 degrees in 68% of healthy, adult volunteers older than age 60. The prevalence of scoliosis affecting the adult increases with age because of the significant rate of occurrence of de novo cases with aging of the spine.9 There is significant evidence that scoliosis is a common condition with a high prevalence on older populations.
The impact of scoliosis on health-related quality of life has also been reported with significant variability. The studies of Robin and colleagues and Schwab and colleagues reporting high prevalences of scoliosis in elderly adults both demonstrate little effect on self-reported health status including pain compared with adults without scoliosis. In contrast, other large studies comparing adults with scoliosis to unaffected controls demonstrate significant impairment in adults with scoliosis.10–14 In a long-term follow-up study of adults with late-onset adolescent scoliosis compared with unaffected controls, adults with scoliosis complained of chronic back pain more often than controls (61% vs. 35%).15 However, overall adults with late-onset adolescent scoliosis are equally productive and function at a relatively high level. Similarly, in a long-term follow-up of adults treated with bracing for adolescent idiopathic scoliosis, adults with scoliosis had measurably more back pain and functional limitations than unaffected controls.16 In a comparison of adults with scoliosis and unaffected controls matched for age, gender, and educational level, Berven and colleagues17 demonstrated measurable impairment of the adults with scoliosis in domains that include pain, function, mental health, and appearance. The development and validation of a disease-specific measure of health status for adults with scoliosis enables an accurate measure of clinical impact and change in health status for adults with scoliosis.18 Measurement of clinical impact and change in health status as a result of treatment is important in defining the value of care for adults with scoliosis.
The costs to the U.S. health care system involved in treating adult deformity are significant. In 2005 the overall cost of spine-related expenses was $86 billion.19 In 2004 $3.7 billion were spent on 134,000 hospital inpatient stays for patients older than 18 with a hospital discharge diagnosis of spinal deformity.20 In addition, there were 410,000 outpatient physician visits by adults with spinal deformity in 2004.21 The outpatient sector including emergency department visits and prescription medications is a significant and rapidly growing cost to our healthcare system.22 In a healthcare economy with limited resources, it is important to identify diseases and disorders that have a significant impact on patient-based assessment of quality of life and to identify treatments that may have a clinically significant impact on improving health-related quality of life. The management of adults with spinal deformity is an area with tremendous potential for improving health-related quality of life.
Classifying Adult Scoliosis
A classification of adult scoliosis is useful to accurately characterize a deformity pattern, to guide treatment and decision making, and to form a basis for the uniform reporting of results of care that may lead to an evidence-based approach to care.23 Adult scoliosis may be broadly divided into scoliosis that existed before skeletal maturity and scoliosis that developed after skeletal maturity, or de novo scoliosis. A nominal classification system for scoliosis was initially introduced by the Terminology Committee of the Scoliosis Research Society in 1969.24 The classification was etiologic and divided disorders of the spine into categories including idiopathic, congenital, neuromuscular, associated with neurofibromatosis, mesenchymal, traumatic, secondary to irritative phenomena, and other. A nominal classification is useful to lend insight into diagnosis and associated comorbidities. The importance of recognizing the etiology of spinal deformity is demonstrated by the disparity of previous publications on natural history and outcome in scoliosis treatment.25–27 The limitations of a nominal system are that it provides little insight into clinical symptoms and lacks guidance for care of specific curve types and locations. In adult scoliosis, global sagittal balance and symptomatic degenerative changes within the deformity are important determinants of the clinical impact of scoliosis on health status and strategies for care. Therefore specific radiographic features of adult deformity are a useful basis for a classification system in the adult.
King and colleagues introduced an ordinal classification system for thoracic idiopathic scoliosis that was intended to provide guidance for treatment of thoracic deformity in children and young adults.28 The authors demonstrated that the classification has significant value in determining the appropriate levels for fusion for thoracic deformities, and with the use of distraction instrumentation, the system led to a low rate of late decompensation and revision surgery. However, the classification has significant limitations including in applicability to current segmental instrumentation systems,29 applicability to patients with lumbar deformity,30 and recognition of alignment and deformity in the sagittal plane.31–33
The Lenke Classification of adolescent idiopathic scoliosis was developed by members of the Harms Study Group with the intent to be comprehensive and encompass all curve types, to be based on objective criteria for each curve type, to emphasize sagittal plane alignment, and to be easily understood and applied.34 The Lenke classification provides a standardized and useful framework for determining the extent of spinal arthrodesis in deformity.35,36 However, there is significant variability in the observed choice of levels by surgeons because of specific structural characteristics within the deformity, and most importantly because of considerations that are apparent from the patient’s clinical presentation that “override” radiographic considerations.37
The adult with spinal deformity presents with clinical and radiographic characteristics that are distinct from the adolescent with spinal deformity. In the adult with scoliosis, specific radiographic parameters have a significant impact on health-related quality of life. Global sagittal alignment has the most significant impact on pain and function, compared with other radiographic parameters including curve location, curve magnitude, and coronal balance.38 Schwab and colleagues39 developed a classification of adult scoliosis that emphasized the clinical impact of specific radiographic parameters including lumbar curve apex, lumbar lordosis, and intervertebral subluxation within the deformity. Further development of this system will include other radiographic parameters including pelvic incidence, trunk inclination, and lumbopelvic relationships.40
The recognition of symptomatic degenerative changes within the deformity including stenosis, spondylolisthesis, and rotational subluxation is critical for an effective classification system in the adult. Similarly, global imbalance of the spine in the sagittal and coronal plane is rare in adolescent idiopathic scoliosis but has an important impact on health status and treatment options in the adult patient. In the Scoliosis Research Society (SRS) Classification of Adult Deformity, Lowe and colleagues41 incorporated radiographic parameters with clinical modifiers. The SRS Classification of Adult Deformity is presented in Table 73–1. The SRS Classification for Adult Deformity is intended to be used by physicians to group patients with similar radiographic presentations and to assist useful multicenter collaborations and comparisons of similar cases. Further work in identifying key factors that influence surgical decision making and outcomes of care will lead to developments of useful classifications for adult scoliosis.
TABLE 73–1 Scoliosis Research Society Classification of Adult Spinal Deformity
| Adult Spinal Deformity Modifiers | |
| Regional sagittal modifier (include only if outside normal range as listed) | |
| (PT) Proximal thoracic (T2-T5) | ≥+20° |
| (MT) Main thoracic (T5-T12) | ≥+50° |
| (TL) Thoracolumbar (T10-L2) | ≥+20° |
| (L) Lumbar (T12-S1) | ≥–40° |
| Lumbar degenerative modifier (include only if present)
• (DDD) ↓ disc height, facet arthropathy, spinal stenosis based on radiograph and/or magnetic resonance imaging
|
|
Clinical Presentation of Adult Scoliosis
The adult with scoliosis may present to a physician caring for disorders of the spine with symptoms that are directly related to the deformity or with pain or symptoms of spinal origin that are unrelated to the presence of scoliosis. Patients with symptomatic adult spinal deformity characteristically present with symptoms related to back pain, radicular symptoms, deformity, progression of the deformity, coronal or sagittal imbalance, or neural compromise. Smith and colleagues42 identified back pain and radicular pain as a complaint in 99% and 85% of patients with adult scoliosis presenting to a neurosurgical practice, and nearly 10% of patients had neural symptoms including weakness and myelopathy. Correlation of clinical symptoms with deformity patterns and degenerative changes within the spine is an important challenge for the physician caring for patients with adult scoliosis. Recognizing patterns of referred pain and radicular pain is useful in identifying a source of pain or spinal origin and in directing nonoperative and operative care.43,44 Careful attention to the patient’s clinical symptoms and goals of care is important in aligning the physician and patient toward a shared process of decision making and toward a satisfactory outcome of care.45
The adult with scoliosis characteristically presents with symptoms that include axial and neurogenic pain, as well as progressive truncal imbalance.46–49 Degenerative changes within the spinal column are an important component of the clinical presentation of adult scoliosis. Spinal stenosis, rotatory subluxation, and nerve compression occur frequently in adult scoliosis and are an important consideration in the patient’s decision to pursue care.50–52 Glassman and colleagues studied a matched cohort of patients with scoliosis who chose to pursue surgery, compared with patients who chose nonoperative care. The authors found that patients who chose surgery had more frequent leg pain, more frequent episodes of moderate to severe back pain, and a higher mean level of daily back pain. Patients who chose surgery also self-reported more impairment with social function and appearance. In a similar study comparing adult scoliosis patients who chose surgical versus nonoperative care, Pekmezci and colleagues demonstrated that functional measures including walking ability and vitality were important determinants of patient preference for surgery over nonoperative care. These studies clearly indicate the importance of identifying and recognizing the patient’s symptoms and goals for care in planning an approach to care.
Present pain and disability are common in the adult presenting with adult scoliosis. These symptoms are not as prevalent in adolescent idiopathic deformity.53–55 The differences in curve patterns and in clinical presentation between the adult with scoliosis and the adolescent with idiopathic scoliosis underlie the fundamental differences in the goals of treatment and surgical strategies for these populations. In the adolescent with idiopathic scoliosis, the goal of care is to prevent progression of deformity and consequences of deformity progression including pain, functional limitations, and truncal imbalance. In the adult with degenerative scoliosis, the goal of care is to improve present pain and disability. The presence of measurable compromise in health-related quality of life in the adult with degenerative scoliosis offers a measurable variable of the success of management and a quantifiable approach for developing an evidence-based approach to care based on patient self-assessment of changes in health status.
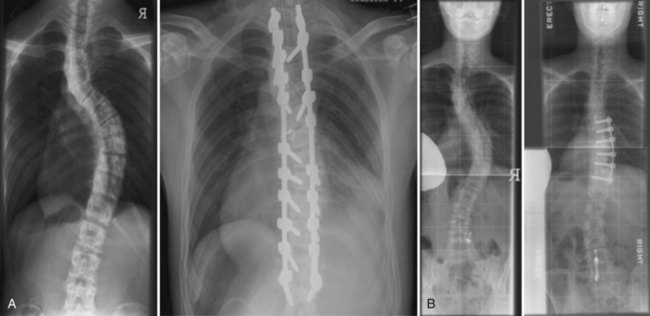
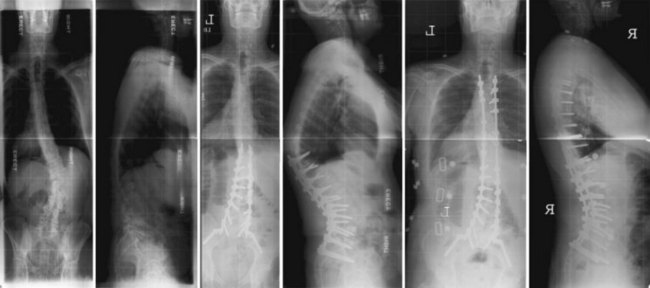
Deformity and concern about progression of deformity are also important considerations in the clinical presentation of the patient with adult scoliosis. Deformity in adult scoliosis may involve malalignment in the coronal, axial, and sagittal planes. Patients with coronal plane deformity often complain of waist asymmetry and ribs abutting the pelvis. The ribs on the concavity of the fractional curve or convexity of the thoracolumbar major curve may approximate the iliac crest and pelvic brim, and patients may complain of painful impingement most commonly in the transition from sitting to standing. Patients with sagittal plane deformity may complain of fatigue and pain on trying to stand erect. Patients may compensate for sagittal plane deformities in the spine with hyperextension of the hips and flexion of the knees. An assessment of pelvic tilt on clinical examination and on standing radiographs is useful in assessing the overall sagittal balance of the spine. Patients with rotation of the spine may complain of rib prominence and apical pain with sitting. Patients with prominent rib deformity may also complain of dissatisfaction with appearance and fit of clothing. Correction of deformity is one of the most reliable goals of surgical intervention for deformity. However, many patients with significant deformity may have limited complaints referable to the deformity. Therefore careful communication with the patient is critical to recognize the role of deformity in the patient’s clinical presentation. Figure 73–1 demonstrates a patient with significant coronal deformity with little pain or functional limitation. A correction of deformity in this patient would be unlikely to improve health-related quality of life in the absence of significant preoperative compromise or deficits.
Progression of deformity in the adult is common and is a reason for which ongoing follow-up of adults with scoliosis is an important role of the physician caring for disorders of the spine. Weinstein and colleagues56 followed a cohort of 194 adult idiopathic scoliosis patients for more than 40 years and noted that 68% had progression of their deformity after skeletal maturity. Thoracic curves greater than 50 degrees had the greatest progression followed by thoracolumbar and lumbar curves. With aging, other important changes in spinal curves include progression of curve size, a loss of lumbar lordosis, and reduced flexibility within the deformity.57,58 Deviren and colleagues59 demonstrated a correlation between age and lateral subluxation within the deformity and the presence of radicular pain. Age-related changes in the spine are an important cause of progressive deformity and progressive symptoms in the adult with scoliosis.
Clinical Evaluation
Activity and walking tolerance are important measures of function. The increasing requirement of walking aids such as a cane or walker may be due to loss of coronal and sagittal balance or to progressive neural dysfunction. Evaluation of gait is an important component of the physical examination. Gait disturbance may be caused by neurogenic etiology, pain, or functional or true leg length inequality. An antalgic gait may be due to axial pain or to radicular pain. Recognition of pathologic gait patterns including ataxic and spastic gaits is important in identifying upper motor neuron pathology including cervical stenosis, myelopathy, and neurodegenerative conditions.60–62 Pelvic obliquity and functional leg-length discrepancy may lead to gait disturbance with characteristic tilting toward the functionally short side for stride clearance. Patients may require support while standing due to fixed coronal imbalance.
An assessment of deformity is an important component of the clinical evaluation. The patient’s self-perception of the deformity may be different than the assessment of a family member or physician.63,64 Donaldson and colleagues65 demonstrated that significant variability in surgeon assessment of deformity may lead to inconsistencies in recommendations regarding operative care. Communication between the physician and patient regarding deformity is important to clarify the patient’s goals of care. Impairment of appearance and self-image is also an important clinical consideration in patients with adult scoliosis and an important goal of deformity correction.66
Careful physical examination is important in the assessment of deformity, localization of pain, and detection of neural deficits. On examination of the patient from the posterior aspect, note the waist asymmetry, trunk shift, and relative heights of the iliac crests. Measurement of leg lengths is important in determining whether pelvic obliquity may be related to a deformity between the pelvis and spine or due to leg-length discrepancy. A plumb line dropped from the spinous process of C7 will demonstrate clinical displacement relative to the midsacral point. The deviation of this line from the gluteal cleft measures the coronal imbalance. The flexibility of the deformity may be determined by testing the patient’s lateral bending or by lifting the patient under the axilla to assess passive correction. Clavicle asymmetry, or elevation of the clavicle contralateral to the major structural curve, will alert the surgeon to the importance of including the upper thoracic curve in the instrumented construct to prevent exacerbation of shoulder asymmetry.67 Figure 73–2A and B demonstrate the importance of extending fixation to include the upper thoracic curve in patients with preoperative elevation of the shoulder ipsilateral to the convexity of a major curve.
Physical examination must also include consideration of the sagittal profile. Inspecting from the side view demonstrates the patient’s lumbar lordosis, sagittal profile, and hip or knee flexion. Patients may compensate for a fixed sagittal malalignment with bending at the knees and extension at the hips. Asking patients to stand with knees fully extended, and noting pelvic tilt on physical examination will yield a more accurate assessment of fixed sagittal plane deformity. Resolution of deformity in the sitting posture may implicate flexion at the pelvic-femoral junction in the cause of sagittal malalignment. The Thomas test performed with the patient supine and pelvis level will demonstrate whether there is a contracture at the pelvic-femoral junction. Recognizing deformity in the sagittal plane is important for surgical planning and for effective improvement of sagittal plane malalignment.68
Radiographic Evaluation of Coronal Imbalance
Radiographic assessment of the adult with scoliosis requires standing 36-inch posteroanterior (PA) and lateral views. To obtain a true representation of coronal and sagittal balance, the patient’s knees and hips should be fully extended and leg-length discrepancy should be balanced with standing blocks. The film should also include the center of the femoral heads and the C7 vertebrae in order to measure pelvic incidence, pelvic tilt, and global spinal balance (Fig. 73–3). The Cobb angles should be measured on the PA and side-bending radiographs. The stable, neutral, and apical vertebrae should also be identified on the PA and side-bending films to aid with preoperative planning. The central sacral line (CSL) is the vertical line extended from the spinous process of S1, perpendicular to the pelvis on the PA radiograph. The stable vertebra is the vertebra that is most closely bisected by the CSL. The neutral vertebra is the nonrotated vertebra at the caudal end of the curve. The apical vertebra is the farthest from the CSL. In adult scoliosis, there is often lateral subluxation of the vertebral bodies and spondylolisthesis within the deformity. Degenerative changes including lateral subluxation and spondylolisthesis are associated with spinal stenosis and neurogenic symptoms. Inadequate plain film evaluation may lead to an incomplete assessment of the causes and extent of deformity.69
Radiographic assessment of flexibility of the spine is useful for the preoperative surgical planning. Supine side-bending films are commonly used and give the surgeon an indication of the flexibility of the major and fractional curves. In patients with more severe deformity, other techniques to assess flexibility of deformity include traction radiographs,70 the push prone technique,71 and fulcrum-bending technique.72 In short radii and larger curves, traction radiographs may give a better indication of flexibility than bending due to constraints between the rib cage and pelvis. The lateral flexion and extension film is useful to measure sagittal plane flexibility and to identify fixed kyphotic deformities. Sagittal plane mobility is an important consideration in surgical planning including the use of osteotomies and the choice of end vertebra. Dynamic instability on flexion and extension films may influence the extent of surgical instrumentation and fusion.
Neural deficits and radicular symptoms are an important clinical presentation of adult scoliosis. Advanced imaging with magnetic resonance imaging (MRI) or computed tomography (CT) scan is important to assess the role of decompression of the neural elements. Spinal canal stenosis and foraminal narrowing are common findings that may need to be addressed if they correlate with findings on history and physical examination. Intrinsic intervertebral disc degeneration is best measured with MRI, and facet arthropathy is most apparent with CT scan. Consideration of advanced and symptomatic degeneration of the caudal motion segments is important in selection of fusion levels. In the osteoporotic patient with compression fractures, MRI is also helpful in detecting recent fractures that may be amenable to nonoperative or less invasive surgical options (vertebral augmentation). In patients with previous fusions or attempted fusions, CT and bone scans are useful to assess bony union or the presence of a pseudarthrosis.73,74
Treatment of Adult Scoliosis
Guidance on when to do more, less, or nothing at all can be useful for the surgeon who is considering a spectrum of options and strategies for care. There is tremendous variability in the management of adult spinal deformity among physicians who care for patients with spinal deformity. Although some of this is driven by the range of pathology and complex expression of the aging spine with deformity, the presence of variability in treatment is also related to the absence of an evidence-based approach to adult deformity. The roles of nonoperative care, decompression alone, limited stabilization, or long fusions have been incompletely defined, and indications for each approach remain in evolution. Shared decision making regarding care for the adult with scoliosis requires clear and extensive communication between the physician and the patient in order to empower the formation of an informed choice. An informed choice regarding healthcare alternatives is based on considerations of the magnitude of the intervention, the expected change in health status, and durability of the change in health status over time. The evidence for each alternative remains incomplete and requires ongoing prospective investigation.75
Nonoperative Care in Adult Scoliosis
Nonoperative approaches to the management of adult scoliosis are directed toward improvement of pain and function, not toward correction of deformity or affecting the pattern of curve progression. There is limited evidence to support the efficacy of nonoperative care for the adult with symptomatic scoliosis.76 Van Dam reported that nonoperative care in adults with scoliosis is most useful in patients with limited pain and symptoms and that patients with significant symptoms received limited benefit from analgesics, orthoses, physical therapy, and activity modification.77 Dickson and colleagues reported on a cohort of patients who were operative candidates and choose nonoperative care. Compared with patients who choose surgery, the group treated nonoperatively had significantly more pain and functional limitations. Smith and colleagues78 reviewed the change in health status of 170 adults with scoliosis treated nonoperatively. The authors found no improvement in pain, disability, or SRS-22 score at 2-year follow-up.78 Each of these studies may be criticized for the absence of a specified protocol for nonoperative care.
Specific treatments for the nonoperative management of adult scoliosis include analgesics, orthotics, physical therapy, manual manipulation, activity modification, behavioral therapy, and injections.79–81 Glassman and colleagues82 reviewed the nonoperative resources used by 123 adults with scoliosis. Sixty-eight patients (55%) reported the use of one or more nonoperative modality including medications, physical therapy, exercise, injections/blocks, chiropractic care, pain management, bracing, and bed rest at a mean treatment cost over the 2-year period of $10,815. Patients treated nonoperatively reported no improvement in pain or disability over a 2-year follow-up. This study brings into question the value of nonoperative treatment commonly used for adult scoliosis patients. Cooper reported on the effect of transforaminal lumbar epidural injections on adults with scoliotic stenosis.83 The author defined a successful outcome as patient satisfaction and at least a two-point improvement on pain and function scores. The authors found good early results, with 60% of patients reporting success at 1 week after injection. However, the results declined significantly with only 27% of patients reporting success at 2-year follow-up. Injections including selective nerve blocks and facet blocks may be useful in identifying symptomatic neural compression and localizing pain generators.84–86 The value of discography in decision making regarding extension of arthrodesis to the lower lumbar spine and pelvis is limited.87,88
Operative Care in Adult Scoliosis
Aging population demographics and advances in surgical technique and anesthesia, combined with changing patient attitudes toward pain and limitations, have contributed to increased surgical rates for adult spinal deformity.89 Compared with the adolescent population, surgery for adult deformity is often more complex and technically difficult. Patients are older and may have significant medical comorbidities. These factors contribute to a high reported rate of complications that can result in the need for reoperation and questioning the value of limited improvement in health-related quality of life compared with the risk of surgery.90
The surgical goals in treating the patient with degenerative scoliosis include neural decompression, improvement of back pain, and restoration of spinal alignment.91,92 Indications for surgery in adult scoliosis include the following:
As discussed in the section on clinical presentation, patients who choose operative care over nonoperative care are more likely to have radicular pain or more severe pain and measurable functional limitations. The decision to pursue operative care over nonoperative care requires an assessment of the expected benefits of surgery compared with the cost of intervention including the risk of perioperative complications. In a debate on operative versus nonoperative care of adult scoliosis, Akbarnia and colleagues reviewed literature that included significant risks to scoliosis in the adult including reported complications of 56% to 75%, unplanned reoperations in 18% to 58%, and unproven benefits regarding improvement in health-related quality of life.93 However, since their review, several studies comparing operative and nonoperative management of adult scoliosis have consistently demonstrated better outcomes with operative care.94–96 Smith and colleagues97 reported on the risk of perioperative complications compared with improvement of health status measure by Oswestry Disability Index. The authors identified more perioperative complications in older adults but a parallel improvement in health status and disability. They concluded that the benefits of operative management of scoliosis in the adult appear to exceed the significant risks for all age groups.
Preoperative Planning and Medical Considerations
Comorbidities are an important determinant of health status and perioperative complications.98 Improvements in surgical techniques and perioperative care have expanded our ability to care for adults with significant comorbidities including pulmonary and cardiac disease, osteoporosis, and nutritional deficiency. With proper planning and patient preparation, medical conditions affecting adult patients can be optimized to decrease, although not eliminate, the perioperative risk.99 Additional potential benefits include decreasing hospital length of stay and recovery for the patient, as well as decreasing overall costs, and therefore use of resources is of benefit to society as a whole. With increasing review of quality of care, it is doubly important that we be vigilant in identifying and optimizing patient baselines preoperatively whenever possible.
Preoperative cardiac and pulmonary assessment is of special importance in the adult patient, especially in a surgical era when age is not a contraindication to major deformity correction. Preoperative pulmonary function testing is useful in patients with a history of frequent pneumonias, associated neuropathic (cerebral palsy, poliomyelitis) or myopathic (muscular dystrophy, primary myopathies) weakness, or subjective dyspnea. Irreversible preoperative vital capacity compromise is a predictor of postoperative respiratory complications.100,101 Other areas of physical health to assess include bone quality, nutritional status, obesity, and tobacco use. Each of these areas may be optimized before considering elective surgical correction. In addition to physical health, the surgeon may consider social, financial, and psychologic well-being of the patient because spinal deformity surgery and subsequent recovery will surely affect all of these areas. Patients who are in optimal physical shape, irrespective of their age, and who are participating in some aerobic activity, have ceased smoking for at least 2 to 3 months, and who are nutritionally sound are more likely to respond to the nonoperative approach and will be better prepared for recovery after surgery.102
Specific Operative Strategies and Considerations
There exists tremendous variability in the operative management of adult scoliosis, with little consensus on surgical strategy regarding approach and levels.103–105 The presence of variability is clear evidence of the absence of an evidence-based approach. Specific areas of controversy in the surgical management of degenerative scoliosis include the role of decompression and/or limited arthrodesis, the role of combined anterior and posterior surgery compared with posterior-only approaches, and the choice of fusion levels at the thoracolumbar and the lumbosacral junction.
Decompression Alone
Radicular pain and neural symptoms are important clinical presentations of adult scoliosis. Limited decompression of stenotic levels may offer significant improvement of clinical symptoms while limiting surgical risks associated with a larger reconstructive operation.106 However, decompression in the setting of deformity may lead to high rates of curve progression and poor outcomes.107 Frazier and colleagues108 demonstrated that preoperative scoliosis is associated with unfavorable outcome in decompressive surgeries for symptomatic spinal stenosis.
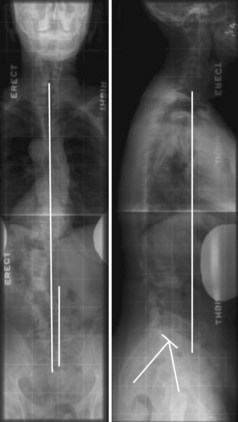
Deformity progression after surgical decompression is an important reason for revision surgery. Figure 73–4 demonstrates a case of deformity progression after multilevel lumbar decompression, requiring combined anterior and posterior reconstruction. Patients who may be the most appropriate candidates for decompression without fusion include the following:
Decompression with a Limited Fusion
Patients with adult scoliosis and pain that is limited to specific spinal segments may be appropriate for a decompression of the neural elements with a limited arthrodesis of the spine. The lumbosacral or fractional curve in adults with scoliosis may be a localized source of symptomatic neural compression and pain, even in the presence of more generalized deformity. Berven and colleagues reported that 3 of 18 patients with adult scoliosis who underwent decompression with a fusion that did not encompass the entire spine required revision surgery at 5-year follow-up. Figure 73–5 demonstrates an example of a decompression with limited fusion in a 62-year-old female with discrete radicular pain and axial pain that localized to the lumbosacral junction of the spine.
An important indication for a decompression with limited fusion is the presence of good global alignment of the spine in the sagittal and coronal planes. Patients with global malalignment of the spine in the sagittal or coronal plane are not appropriate candidates for a limited decompression and fusion. Unplanned revision rates in adult scoliosis surgery of 18% to 54% indicate that limited fusion should be performed with careful assessment of risks of deformity progression at adjacent segments, especially the thoracolumbar and lumbosacral junctions. Figure 73–6 demonstrates an example of an attempted limited decompression and fusion in a 74-year-old female with multiple comorbidities. She remained with significant deformity in the sagittal and coronal planes and required a three-column osteotomy for reconstruction and improvement of pain and function.
The thoracolumbar and lumbosacral junctions offer significant biomechanical challenges that may contribute to relatively high rates of implant failure, nonunion, and adjacent segment progressive deformity. The challenges of thoracolumbar and lumbosacral junctions are well-recognized by surgeons who care for patients with adult deformity.109–116 There is significant variability in the choice of cephalad and caudad levels in patients with adult lumbar spine deformity. Junctional complications are common and significant in fusions to the lumbosacral and thoracolumbar regions of the spine. Segmental instrumentation is an effective technique for selective of thoracic and lumbar deformity, and the technique generates a significant gradient in mobility of the spine between instrumented and noninstrumented levels. Long fusions with a cephalad level at the thoracolumbar junction may be compromised by progression of kyphosis above the fusion related to implant failure or adjacent segment kyphosis. Kuklo reviewed the biomechanical considerations in adult deformity that may optimize outcome in adult deformity reconstructions and concluded that coronal and sagittal alignment are important to avoid adjacent segment decompensation.117
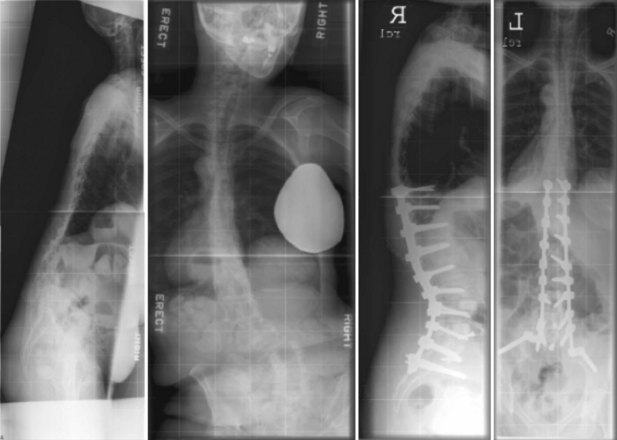
Adjacent segment kyphosis at the thoracolumbar junction is a frequent complication of adult deformity surgery. Swank and colleagues118 reported that fusions from L1 or L2 to the sacrum had an unacceptable rate of mechanical failure, with 7 of 20 cases developing junctional progression of deformity. Similarly, Simmons reported adjacent segment kyphosis, or “topping off,” in 60% of long fusions with a cephalad level at L1 or L2.119 More recently, Glattes and colleagues120 reported a 26% incidence of proximal junctional kyphosis in long adult deformity surgeries. In this series, the rate was highest at T3. At the thoracolumbar junction, Suk121 reported that stopping instrumentation at or distal to T11 increases the risk of adjacent segment kyphosis, with a rate of 50% in patients with long fusions ending at T12 or L1. Sethi and colleagues122 reviewed 218 patients with long fusions from the thoracolumbar junction to L5 or S1. The authors identified a 34% incidence of kyphosis greater than 10 degrees at the segment above the highest instrumented vertebra, and 12% of patients required revision surgery. Deformity constructs to T10 or T11 had a trend toward a lower need for revision than constructs to T12 or L1. Choosing a level for the highest instrumented vertebra in adult scoliosis is important for limiting complications. Indications for a more proximal extension of instrumentation and fusion include a thoracic curve extending above the planned top instrumented vertebra or segmental kyphosis greater than 5 degrees above the planned top instrumented vertebra. Figure 73–7 demonstrates a case of a patient with preoperative thoracolumbar kyphosis who developed progressive kyphosis above his fusion to T10 and required proximal extension of his fusion to the upper thoracic spine.
The lumbosacral junction of the spine offers similar challenges in decision making. The choice to end a fusion at L5 or S1 has important consequences, and there remains significant controversy regarding long constructs to the lumbosacral junction that compromises the ability of surgeons and patients to make informed choices.123–125 Terminating a fusion at L5 reduces the magnitude of the procedure and may limit perioperative complications.126,127 However, this benefit may come at the cost of a loss of deformity correction over time and a need for future surgery with extension of arthrodesis to the sacrum.128,129 Specifically, Edwards and colleagues published two separate papers on a cohort of patients whose fusions stopped at L5. In a retrospective case series, they found the incidence of radiographic subsequent degeneration at L5-S1 to be 61% over a mean follow-up of 5.6 years. Subsequent advance degeneration (SAD) at L5-S1 led to a progressive loss of sagittal plane balance, and 4/19 patients with degeneration at L5-S1 required revision surgery at L5-S1.129 Edwards and colleagues131 subsequently matched this cohort to a series of patients who underwent long fusions to the sacrum in the presence of a healthy L5-S1 disc, once again noting a high incidence of subsequent degenerative changes at L5-S1 at a mean of 5.2 years follow-up. Importantly, the SRS-24 outcome scores were no different between groups. In contrast, a higher rate of surgical complications including pseudarthroses and reoperations was seen in the sacrum cohort after the index surgery. Eck and colleagues132 identified 59 patients fused to L4, L5, or S1. The patients fused short of the sacrum did not have a reliable maintenance of global sagittal balance, with 7 of 44 patients demonstrating subsequent degeneration. Those patients with subsequent degeneration below L4 or L5 had worse clinical outcomes including postoperative pain and function.132 Swamy and colleagues133 reported on the need for revision surgery in patients fused to L5 and found a 10-year survival of 70%, with most revisions needed in the first 2 years after surgery. Therefore a subset of patients can have reliable and stable results with long fusions ending at L4 or L5. Clear indications to extend instrumentation and fusion to the level of the sacrum include the following:
In the absence of clear indications to extend arthrodesis to the sacrum, stopping long fusions at L5 may be a reasonable surgical choice. Figure 73–8 demonstrates a successful long fusion to L5 is a 63-year-old female who had her original surgery 24 years before developing lumbosacral pain and L5 radicular pain, leading to a late revision.
Surgical Approaches in Adult Deformity Surgery
Anterior Only, Anterior and Posterior, and Posterior Only
The choice of a surgical approach to the spine in adult deformity has an important effect on the morbidity of surgery and on the efficacy of deformity correction and clinical outcomes. In some deformity patterns, there may be clinical equipoise between an anterior-only and a posterior-only approach to surgical correction. Specifically, in thoracolumbar deformity, or Lenke type 5C curves, or in single overhang thoracic curves, an anterior or a posterior approach may result in similar correction and clinical outcomes.134–137 In contrast, a balanced double thoracic or balanced double major deformity may be decompensated with an anterior-only approach or with an asymmetric correction of one curve compared with the other. Surgical approaches to the correction of adult deformity have evolved significantly with the development of posterior segmental instrumentation systems and the development of surgical techniques for three-column osteotomies through a posterior approach.
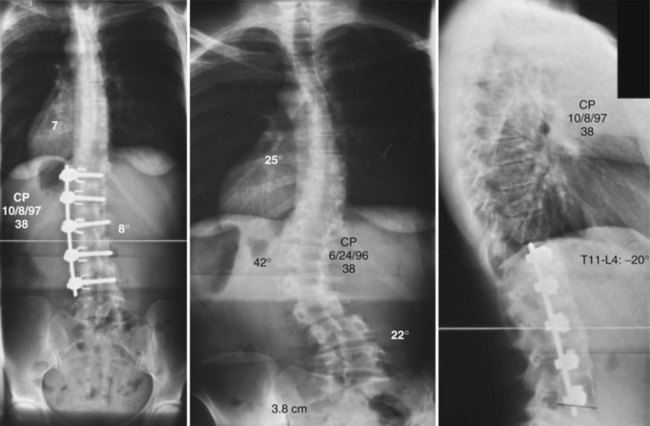
Anterior surgery for the treatment of thoracolumbar scoliosis in the adult was introduced by Dwyer in 1969.138 With semirigid instrumentation introduced by Zielke, several authors demonstrated that anterior correction of thoracolumbar deformity had significant advantages over posterior nonsegmental surgery including sparing motion segments, saving posterior muscle integrity, and more effective deformity correction in the coronal and axial planes.139–142 Smith and colleagues143 reported excellent clinical outcomes with limited complications in a series of 15 consecutive adult patients treated with rigid single-rod anterior surgery for thoracolumbar scoliosis. The authors reported no kyphotic decompensation or nonunion with rigid instrumentation and structural interbody grafts and demonstrated fewer levels fused compared with posterior surgery. Deviren and colleagues144 reported similar outcomes in adults with thoracolumbar scoliosis compared with adolescents. Figure 73–9 demonstrated an anterior-only approach with a single rigid rod instrumentation for a 38-year-old male with a thoracolumbar deformity.
In a comparison of anterior surgery with Zielke semirigid fixation with Cotrel-Dubousset posterior segmental instrumentation, Suk demonstrated better correction in the frontal plane and in rotation with the ventral derotation system of Zielke. However, sagittal plane alignment and postoperative maintenance of correction was better in the posterior group.145 With the introduction of pedicle screws and the ability to gain segmental fixation of the spine with a powerful capacity for rotation and rigid fixation, posterior approached to thoracolumbar deformity gained a comparable ability to correct deformity including rotational and preserve levels.146,147 In a recent comparison of anterior and posterior approaches to Lenke 5C thoracolumbar curves, Geck and colleagues148 demonstrated that posterior-only correction of deformity resulted in significantly better curve correction, less loss of correction over time, and shorter hospital stays.
Anterior approaches to adult scoliosis may be useful in the release of a rigid deformity, improvement of sagittal alignment, and gaining effective arthrodesis of the spine. Bradford and colleagues149 demonstrated that a combined anterior and posterior approach to Scheuermann kyphosis resulted in significantly better deformity correction and better fusion rates and maintenance of correction over the instrumented segments than posterior-only surgery with nonsegmental instrumentation. Similarly, in adult scoliosis, a combined anterior and posterior approach has been advocated for improvement of lumbar lordosis and improvement of fusion rates, especially at the lumbosacral junction.150–152
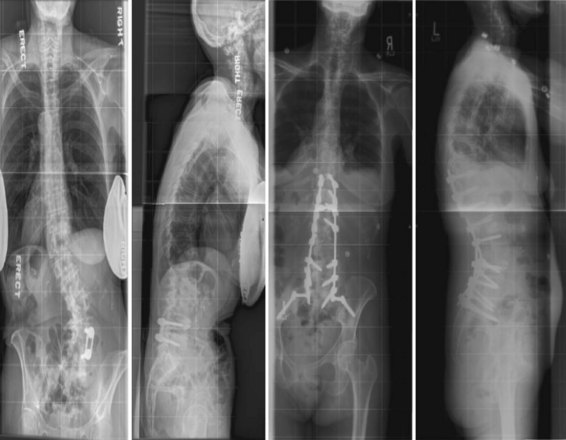
Combined anterior and posterior surgery in adult deformity has resulted in good clinical outcomes and radiographic corrections but has been associated with significant perioperative complications. Berven and colleagues153 reported the clinical and radiographic outcomes of combined anterior and posterior surgery in 25 adults with scoliosis and significant sagittal plane deformity. The authors demonstrated effective deformity correction in the coronal and sagittal planes, with high rates of patient satisfaction. Patients with preoperative lumbar hypolordosis (>−30 degrees) had the most reliable improvement of health status. However, 40% of patients had perioperative or late complications including wound infection, dural tear, pneumonia, and pseudarthrosis. Other authors have confirmed a high rate of surgical complications in combined anterior and posterior approaches to adult scoliosis.154–159 The role of minimally invasive approaches to the anterior column including direct lateral approaches may expand the indications and use of anterior surgery for adult scoliosis, but long-term outcome of the direct lateral approach in deformity is not available at this time.160 Relative indications for a combined anterior and posterior approach to adult deformity may include correction of a fixed lumbosacral obliquity, lumbar hypolordosis, posterior-element deficiency, pseudarthrosis, and bone stock insufficiency, especially at the lumbosacral junction of the spine. Figure 73–10 demonstrates a combined anterior and posterior approach for a 57-year-old male with adult scoliosis and a rigid, hypolordotic lumbar deformity with severe multilevel stenosis.
Posterior Approaches
Posterior-only approaches to adult scoliosis may offer significant advantages over combined anterior and posterior approaches. These advantages include effective management of double major curves through a single incision, posterior decompression of the neural elements, better pulmonary tolerance, and single-stage surgery. Over the past decade, there has been a significant paradigm shift from anterior-only and combined anterior and posterior surgery to posterior-only approaches to deformity. Factors that have contributed to this change include the development of transpedicular segmental instrumentation, which transfers powerful forces for deformity correction to the spine, and the evolution of surgical techniques. The use of posterior-based techniques for interbody fixation permits effective circumferential arthrodesis of the spine from a posterior-only approach.161 Crandall and Revella162 demonstrated similar clinical and radiographic outcomes in adults with degenerative scoliosis treated with a thoracolumbar interbody fusion or a separate anterior lumbar interbody fusion at the lumbosacral junction. The development of three-column osteotomies for correction of more rigid spinal deformity permits effective correction of even large deformities without an anterior release. Posterior-based three-column osteotomies including transpedicular wedge resection and vertebral column resections may be useful for the correction of severe sagittal and coronal plane deformity. The use of osteobiologics may improve fusion rates in adult scoliosis surgery and preclude the need for circumferential fusion at the lumbosacral junction.163
Lee and colleagues164 demonstrated that a posterior-only approach to Scheuermann kyphosis with thoracic pedicle screws and apical osteotomies is more effective than a combined anterior and posterior approach. In a matched comparison, patients treated with posterior surgery had less blood loss and operating time, better correction and maintenance of correction, and fewer complications. Similarly, in adult scoliosis, posterior-only surgery has been associated with fewer complications and similar clinical outcomes compared with anterior and posterior approaches.165 Suk166 demonstrated that the posterior approach with transpedicular fixation results in deformity correction that is comparable with anterior and posterior approaches and avoids the complications of a separate anterior approach. Kim and colleagues167 then addressed whether an anterior apical release of the lumbar curve in adult deformity is necessary for effective deformity correction. The authors compared patients undergoing an anterior release and fusion, followed by posterior fusion with a matched cohort treated with posterior correction and fusion, followed by anterior fusion. They concluded that both techniques resulted in similar deformity correction. However, there were more complications in the anterior and posterior group, and clinical outcome was significantly better in the patients who underwent a posterior-based deformity correction followed by an anterior surgery for the lumbosacral junction. Pateder and colleagues168 compared outcomes and complications in adults with thoracolumbar scoliosis measuring 40 to 70 degrees. The authors demonstrated similar radiographic correction of deformity for each group. However, patients with staged anterior and posterior surgery had significantly more perioperative complications. Posterior-only approaches may be effective even in severe deformities. In a comparison of patients with curves greater than 90 degrees treated with combined anterior and posterior surgery versus posterior-only surgery, Dobbs and colleagues169 demonstrated similar deformity correction and complications, but significantly less impairment of pulmonary function in patients treated with posterior-only surgery. Figure 73–11 demonstrates a posterior-only approach to deformity in a 68-year-old female with multiple prior anterior surgeries including colostomy.
For severe spinal deformity, vertebral column resection is a useful technique to permit spinal column shortening and trunk translation. Bradford introduced the vertebral column resection with a combined anterior and posterior approach.170 Suk and colleagues171 developed a posterior-only approach to vertebral column resection for severe spinal deformities. Lenke and colleagues172 have demonstrated effective deformity correction in adult and pediatric scoliosis with a posterior-based vertebral column resection, although the authors have identified a significant risk to the neural elements with the procedure. A posterior-only vertebral column resection may be effective for spinal deformity that is focal and in which the apex of coronal and sagittal deformity is matched. The combined anterior and posterior approach may be more effective in treating the patient with a deformity that extends across multiple segments, deformity that involves multiple apices including different apices in the coronal and sagittal planes, and in the spine with hypokyphosis or lordosis across the thoracic spine. Figure 73–12 demonstrates a severe postoperative deformity treated with a single-stage, posterior-based vertebral column resection.
Complications of Adult Scoliosis Surgery
Neural injury may include injury to the spinal cord or injury to the optic nerve or peripheral nerves during surgery. Neural injury in spinal deformity surgery may result from direct trauma or compression of the neural elements by instrumentation or by bone and soft tissue displaced during deformity correction. Neural injury may also be caused indirectly, as a result of vascular compromise or elongation of the spinal cord. MacEwen and colleagues reported an incidence of neural injury of 0.72% on the basis of voluntary reporting by members of the Scoliosis Research Society.173 The results of the survey revealed 74 complications involving the spinal cord with 41 involving complete paralysis and 33 incomplete lesions. The authors identified risk factors for neural injury including congenital scoliosis, nonidiopathic scoliosis, severe kyphosis distraction instrumentation without preoperative traction, and failure of the surgeon to identify insufficiency of the posterior elements. With the advent of segmental instrumentation systems, multiple sublaminar and intrapedicular fixation sites, and the improvement of capacity to correct deformity, one might expect the risk of neural injury in deformity surgery to increase significantly. However, in subsequent surveys of the Scoliosis Research Society, no overall increase in the prevalence of spinal cord injury has been observed.174 The report of neural complications from the experience of individual surgeons and surgical centers may represent a more consecutive series and complete assessment, and such reports have demonstrated complete or partial cord deficits in up to 16% of patients undergoing correction with a combination of sublaminar wiring and distraction instrumentation.175–177 In a comprehensive review of more than 11 years of experience using posterior and/or anterior spinal segmental instrumentation, Bridwell and colleagues178 reported four cases of major neural injury out of 1090 surgeries. All four cases involved a combined anterior and posterior approach to the spine, with harvesting of the convex segmental vessels. Risk factors for neural injury were identified as hyperkyphosis and combined anterior and posterior surgery.
Intraoperative assessment of neural function is useful for the early detection of neural injury and for the reversal of traction or compression that may be etiologic. An intraoperative assessment of neural function may be made directly by awakening the patient after instrumentation and deformity correction and demonstrating intact corticospinal tracts by having the patient move the lower extremities voluntarily. The Stagnara wake-up test provides a functional assessment of spinal cord integrity and remains a useful tool, especially in the event of a change in monitored evoked potentials.179,180 Continuous intraoperative neurologic monitoring is available with the use of evoked potentials. Direct monitoring of the corticospinal tract is accomplished by motor evoked potentials. The combination of motor and somatosensory evoked potential monitoring improves the sensitivity and predictive value of intraoperative changes in amplitude and latency.181
Vascular injury may result from direct injury to a major vessel or from thromboembolic disease. The choice of surgical approach may minimize the risk of vascular injury and affect the ability to repair bleeding vessels. In separate publications within 1 year, McAfee reported on complications of the open anterior approach to the thoracolumbar spine and the endoscopic approach for thoracolumbar spinal reconstruction.182,183 Vascular complication occurred only in one laparoscopic case, and this was repaired with an open approach. Other series have reported a rate of up to 18% significant vascular injury resulting from the anterior approach to the spine.184–189 Vascular injury from the posterior approach to the spine is less common but can have devastating complications.190 Papadoulas and colleagues191 identified a prevalence of injury to the major vessels anteriorly in 1 to 5 cases/10,000 in posterior lumbar disc excision. Presentations included acute hemorrhage and shock, as well as late presentations of pseudoaneurysm and arteriovenous fistula. Vascular injury may also result from thromboembolism to the aorta, iliac, or femoral arteries as a result of manipulation.192 Kulkarni and colleagues reported eight cases of vascular insufficiency to the lower extremity after an anterior approach to the L4-5 level.193 Five cases involved thrombosis to the common iliac or femoral arteries, two cases involved functional vasospasm, and one involved an intimal tear. The authors recommend intraoperative monitoring with pulse oximetry to the toes as a method to assist with early detection in patients at risk.
Reported rates of deep venous thrombosis vary from 0.3% to 31% depending on patient populations and methods of surveillance.194 Thrombotic risk is greater with anterior surgery and with injury to the vein.195 The use of perioperative prophylaxis to prevent deep venous thrombosis remains controversial.196 The utility and safety of chemical prophylaxis remains undefined, and the benefit of reducing the occurrence of thromboembolic events may be limited compared with the risk of epidural hematoma or wound complications. Therefore decision making on thromboprophylaxis in the spine must be made on a case-by-case basis, with consideration of patient risk factors and surgical approach.
Reoperation after spinal surgery may be considered a failure of the initial surgery by both the patient and the surgeon and represents the need for multiple procedures on a group that is at significant risk for complications. Frequently cited reasons for reoperation for adult spinal deformity are deep wound infection (2% to 11%),197,198 pseudarthrosis (4% to 24%),199,200 and adjacent segment decompensation (1% to 3%).201,202 Additional reasons include neurologic complications, loss of correction, implant failure or pullout, and prominent or painful implants. From a patient standpoint, the risk of reoperation may be an important factor in the initial decision to proceed with surgery. Knowledge of the rate, reason, and time of reoperation may assist the surgeon and the patient during preoperative discussions and may increase awareness of problems that commonly occur postoperatively. Identifying specific risk factors for complications and revision may also be useful in the early recognition or avoidance of specific complications.
Future Directions
Optimal treatment of adult scoliosis remains controversial and without specific guidance. Identifying specific surgical strategies that may lead to the best clinical outcomes with the least risk is an important goal for future research. Schwab and colleagues203 have used multivariate regression models to identify patient-specific factors that are predictive of good outcomes and complications. Patients who are most likely to reach a clinically significant improvement after surgery include older patients with greater preoperative disability and more significant deformity. Patients who are most likely to have perioperative complications include those with significant sagittal deformity and those requiring fusion to the pelvis. Further development of predictive models may lead to a reliable strategy for the management of specific cases.
1 Bess S, Boachie-Adjei O, Burton D, et al. International Spine Study Group: Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine. 2009;34:2186-2190. 15
2 Carter OD, Haynes SG. Prevalence rates for scoliosis in US adults: results from the first National Health and Nutrition Examination Survey. Int J Epidemiol. 1987;16:537-544.
3 Pappou IP, Girardi FP, Sandhu HS, et al. Discordantly high spinal bone mineral density values in patients with adult lumbar scoliosis. Spine. 2006;31:1614-1620.
4 Perennou D, Marcelli C, Herisson C, et al. Adult lumbar scoliosis. Epidemiologic aspects in a low-back pain population. Spine. 1994;19:123-128.
5 Urrutia J, Ledezma CD, Espinosa J, et al: Lumbar scoliosis in postmenopausal women: Prevalence and relationship with boned density, age and body mass index. Spine. In press.
6 Healey JH, Lane JM. Structural scoliosis in osteoporotic women. Clin Orthop Relat Res. 1985;195:216-223.
7 Robin GC, Span Y, Steinberg R, et al. Scoliosis in the elderly: A follow-up study. Spine. 1982;7:355-359.
8 Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30:1082-1085.
9 Kobayashi T, Atsuta Y, Takemitsu M, et al. A prospective study of de novo scoliosis in a community based cohort. Spine. 2006;31:178-182. 15
10 Cordover AM, Betz RR, Clements DH, et al. Natural history of adolescent thoracolumbar and lumbar idiopathic scoliosis into adulthood. J Spinal Disord. 1997;10:193-196.
11 Jackson RP, Simmons EH, Stripinis D. Incidence and severity of back pain in adult idiopathic scoliosis. Spine. 1983;8:749-756.
12 Kostuik JP, Bentivoglio J. The incidence of ow back pain in adult scoliosis. Acta Orthop Belg. 1981;47:548-559.
13 Pérennou D, Marcelli C, Hérisson C, et al. Adult lumbar scoliosis. Epidemiologic aspects in a low-back pain population. Spine. 1994;19:123-128.
14 Witt I, Vestergaard A, Rosenklint A. A comparative analysis of x-ray findings of the lumbar spine in patients with and without lumbar pain. Spine. 1984;9(3):298-300.
15 Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289:559-567.
16 Danielsson AJ, Nachemson AL. Back pain and function 22 years after brace treatment for adolescent idiopathic scoliosis: a case-control study-part I. Spine. 2003;28:2078-2085. discussion 2086 15
17 Berven S, Deviren V, Demir-Deviren S, et al. Studies in the modified Scoliosis Research Society Outcomes Instrument in adults: validation, reliability, and discriminatory capacity. Spine. 2003;28:2164-2169. discussion 2169
18 Bridwell KH, Berven S, Glassman S, et al. Is the SRS-22 instrument responsive to change in adult scoliosis patients having primary spinal deformity surgery? Spine. 2007;2007(32):2220-2225.
19 Martin BI, Turner JA, Mirza SK, et al. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997-2006. Spine. 2009;34:2077-2084.
20 Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Inpatient Sample, 2004.
21 National Center for Health Statistics, National Ambulatory Medical Care Survey, 2004
22 Luo X, Pietrobon R, Sun SX, et al. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976). 2004;29(1):79-86.
23 Garbuz DS, Masri BS, Esdaile J, et al. Classification systems in orthopaedics. J Am Acad Orthop Surg. 2002;10:290-297.
24 Goldstein LA, Waugh TR. Classification and terminology of scoliosis. Clin Orthop. 1973;93:10-22.
25 Bjure J, Nachemson A. Non-treated scoliosis. Clin Orthop Relat Res. 1973;93:44-52.
26 Nilsonne U, Lundgren KD. Long-term prognosis in idiopathic scoliosis. Acta Orthop Scand. 1968;39:456-458.
27 Collis D, Ponseti I. Long-term follow-up of patients with idiopathic scoliosis not treated surgically. J Bone Joint Surg. 1969;51A:425-431.
28 King H, Moe J, Bradford DS, et al. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:1302-1313.
29 Roye DP, Farcy JP, Ricjert JB, et al. Results of spinal instrumentation of adolescent idiopathic scoliosis by King type. Spine. 1992;7:S270-S273.
30 Lenke LG, Betz RR, Clements D, et al. Curve prevalence of a new classification of operative adolescent idiopathic scoliosis. Spine. 2002;27:604-611.
31 Halm H, Castro WH, Jerosch J, et al. Sagittal plane correction in “King-classified” idiopathic scoliosis patients treated with Cotrel-Dubousset instrumentation. Acta Orthop Belg. 1989;61:294-301.
32 Cruickshank JL, Koike M, Dickson RA. Curve patterns in idiopathic scoliosis. A clinical and radiographic study. J Bone Joint Surg. 1989;71-B:259-263.
33 Coonrad R, Murrell G, Motley G, et al. A logical coronal pattern classification of 2,000 consecutive idiopathic scoliosis cases based on the Scoliosis Research Society-defined apical vertebra. Spine. 1998;23:1380-1391.
34 Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J Bone Joint Surg. 2001;83A:1169-1181.
35 Lenke LG. Lenke classification system of adolescent idiopathic scoliosis: Treatment recommendations. AAOS Instructional Course Lectures. 2005;54:537-542.
36 Lenke LG, Edwards CC, Bridwell KH. The Lenke classification of adolescent idiopathic scoliosis: How it organizes curve patterns as a template to perform selective fusions of the spine. Spine. 2003;28(20S):S199-S207.
37 Lenke LG, Betz RR, Haher TR, et al. Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis: Curve classification, operative approach, and fusion levels. Spine. 2001;26:2347-2353.
38 Glassman SD, Berven S, Bridwell KH, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682-688.
39 Schwab F, Farcy JP, Bridwell K, et al. A clinical impact classification of scoliosis in the adult. Spine. 2006;31:2109-2114. 15
40 Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine. 2009;34:E599-E606.
41 Lowe T, Berven SH, Schwab FJ, et al. The SRS classification for adult spinal deformity: Building on the King/Moe and Lenke classification systems. Spine. 2006;31(19 Suppl):S119-S125.
42 Smith JS, Fu KM, Urban P, et al. Neurological symptoms and deficits in adults with scoliosis who present to a surgical clinic: Incidence and association with the choice of operative versus nonoperative management. J Neurosurg Spine. 2008;9:326-331.
43 Milette PC. Radiculopathy, radicular pain, radiating pain, referred pain: What are we really talking about? Radiology. 1994;192:280-282.
44 Bogduk N. The innervation of the lumbar spine. Spine. 1983;8:286-293.
45 Lurie JD, Weinstein JN. Shared decision-making and the orthopaedic workforce. Clin Orthop Relat Res. 2001;385:68-75.
46 Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925-948.
47 Fraser JF, Huang RC, Girardi FP, et al. Pathogenesis, presentation, and treatment of lumbar spinal stenosis associated with coronal or sagittal spinal deformities. Neurosurg Focus. 2003;14:1-9.
48 Simmons EDJr, Kowalski JM, Simmons EH. The results of surgical treatment for adult scoliosis. Spine. 1993;18:718-724.
49 Bradford D. Adult scoliosis: Current concepts of treatment. Clin Orthop. 1988;229:70-87.
50 Epstein JA, Epstein BS, Jones MD. Symptomatic lumbar scoliosis with degenerative changes in the elderly. Spine. 1979;4:542-547.
51 Liu H, Ishihara H, Kanamori M, et al. Characteristics of nerve root compression caused by degenerative lumbar spinal stenosis with scoliosis. Spine J. 2003;3:524-529.
52 Ploumis A, Transfeldt E, Gilbert TJ, et al. Degenerative lumbar scoliosis: radiographic correlation of lateral rotatory olisthesis with neural canal dimensions. Spine. 2006;31:2353-2358.
53 King HA. Back pain in children. Pediatr Clin North Am. 1984;31:1083-1095.
54 Ramirez N, Johnston CE, Browne RH. The prevalence of back pain in children who have idiopathic scoliosis. J Bone Joint Surg Am. 1997;79:364-368.
55 D’Andrea LP, Betz RR, Lenke LG, et al. Do radiographic parameters correlate with clinical outcomes in adolescent idiopathic scoliosis? Spine (Phila Pa 1976). 2000;15(25):1795-1802.
56 Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289:559-567.
57 Murata Y, Takahashi K, Hanaoka E, et al. Changes in scoliotic curvature and lordotic angle during the early phase of degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2002;27:2268-2273.
58 Pritchett JW, Bortel DT. Degenerative symptomatic lumbar scoliosis. Spine. 1993;18:700-703.
59 Deviren V, Berven S, Kleinstueck F, et al. Predictors of flexibility and pain patterns in thoracolumbar and lumbar idiopathic scoliosis. Spine. 2002;27:2346-2349.
60 Lee MJ, Garcia R, Cassinelli EH, et al. Tandem stenosis: A cadaveric study in osseous morphology. Spine J. 2008;8:1003-1006.
61 Lim MR, Huang RC, Wu A, et al. Evaluation of the elderly patient with an abnormal gait. J Am Acad Orthop Surg. 2007;15:107-117.
62 Baik JS, Kim JY, Park JH, et al. Scoliosis in patients with Parkinson’s disease. J Clin Neurol. 2009;5:91-94.
63 Smith PL, Donaldson S, Hedden D, et al. Parents’ and patients’ perceptions of postoperative appearance in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2006;31:2367-2374.
64 Sanders JO, Harrast JJ, Kuklo TR, et al. Spinal Deformity Study Group: The Spinal Appearance Questionnaire: Results of reliability, validity, and responsiveness testing in patients with idiopathic scoliosis. Spine. 2007;32:2719-2722.
65 Donaldson S, Hedden D, Stephens D, et al. Surgeon reliability in rating physical deformity in adolescent idiopathic scoliosis. Spine. 2007;32:363-367.
66 Kostuik JP, Israel J, Hall JE. Scoliosis surgery in adults. Clin Orthop Relat Res. 1973;93:225-234.
67 Kuklo TR, Lenke LG, Graham EJ, et al. Correlation of radiographic, clinical, and patient assessment of shoulder balance following fusion versus nonfusion of the proximal thoracic curve in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2002;27:2013-2020.
68 Berven SH, Deviren V, Smith JA, et al. Management of fixed sagittal plane deformity: Results of the transpedicular wedge resection osteotomy. Spine (Phila Pa 1976). 2001;26:2036-2043.
69 Horton WC, Brown CW, Bridwell KH, et al. Is there an optimal patient stance for obtaining a lateral 36” radiograph? A critical comparison of three techniques. Spine. 2005;30:427-433.
70 Polly DWJr, Sturm PF. Traction versus supine side bending. Which technique best determines curve flexibility? Spine. 1998;23:804-808.
71 Vedantam R, Lenke LG, Bridwell KH, et al. Comparison of push-prone and lateral-bending radiographs for predicting postoperative coronal alignment in thoracolumbar and lumbar scoliotic curves. Spine (Phila Pa 1976). 2000;25:76-81.
72 Cheung KM, Luk KD. Prediction of correction of scoliosis with use of the fulcrum bending radiograph. J Bone Joint Surg Am. 1997;79:1144-1150.
73 Deckey JE, Court C, Bradford DS. Loss of sagittal plane correction after removal of spinal implants. Spine. 2000;25:2453-2460.
74 Berven S, Kao H, Deviren V, et al. Treatment of thoracic pseudarthrosis in the adult: Is combined surgery necessary? Clin Orthop Relat Res. 2003;411:25-31.
75 Bridwell KH, Berven S, Edwards C2nd, et al. The problems and limitations of applying evidence-based medicine to primary surgical treatment of adult spinal deformity. Spine. 2007;32(19 Suppl):S135-S139.
76 Bridwell KH, Glassman S, Horton W, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: A prospective multicenter evidence-based medicine study. Spine. 2009;34:2171-2178.
77 van Dam BE. Nonoperative treatment of adult scoliosis. Orthop Clin North Am. 1988;19:347-351.
78 Smith JS, Shaffrey CI, Berven S, et al. Spinal Deformity Study Group: Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery. 2009;65:86-93. discussion 93-94
79 Winter RB, Lonstein JE. Adult scoliosis. Instr Course Lect. 1983;32:170-191.
80 Fast A. Low back disorders: Conservative management. Arch Phys Med Rehabil. 1988;69:880-891.
81 Cummins J, Lurie JD, Tosteson TD, et al. Descriptive epidemiology and prior healthcare utilization of patients in the Spine Patient Outcomes Research Trial’s (SPORT) three observational cohorts: Disc herniation, spinal stenosis, and degenerative spondylolisthesis. Spine. 2006;31:806-814.
82 Glassman SD, Carreon LY, Shaffrey CI, et al. The costs and benefits of nonoperative management for adult scoliosis. Spine. 2010;35:578-582.
83 Cooper G, Lutz GE, Boachie-Adjei O, et al. Effectiveness of transforaminal epidural steroid injections in patients with degenerative lumbar scoliotic stenosis and radiculopathy. Pain Physician. 2004;7:311-317.
84 Schwarzer AC, Derby R, Aprill CN, et al. The value of the provocation response in lumbar zygapophyseal joint injections. Clin J Pain. 1994;10:309-313.
85 Sehgal N, Dunbar EE, Shah RV, et al. Systematic review of diagnostic utility of facet (zygapophysial) joint injections in chronic spinal pain: an update. Pain Physician. 2007;10:213-228.
86 Young IA, Hyman GS, Packia-Raj LN, et al. The use of lumbar epidural/transforaminal steroids for managing spinal disease. J Am Acad Orthop Surg. 2007;15:228-238.
87 Kostuik JP. Decision making in adult scoliosis. Spine. 1979;4:521-525.
88 Carragee EJ, Lincoln T, Parmar VS, et al. A gold standard evaluation of the “discogenic pain” diagnosis as determined by provocative discography. Spine (Phila Pa 1976). 2006;31:2115-2123.
89 Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259-1265.
90 Albert TJ, Purtill J, Mesa J, et al. Health outcome assessment before and after adult deformity surgery. A prospective study. Spine. 1995;20:2002-2004.
91 Oskouian RJ, Shaffrey CI. Degenerative lumbar scoliosis. Neurosurgery Clin N Am. 2006;17:299-315.
92 Bradford DS, Tay BK, Hu SS. Adult scoliosis: Surgical indications, operative management, complications, and outcomes. Spine. 1999;24:2617-2629.
93 Akbarnia BA, Ogilvie JW, Hammerberg KW. Debate: Degenerative scoliosis: to operate or not to operate. Spine. 2006;31(19 Suppl):S195-S201.
94 Smith JS, Shaffrey CI, Berven S, et al. Spinal Deformity Study Group: Operative versus nonoperative treatment of leg pain in adults with scoliosis: A retrospective review of a prospective multicenter database with two-year follow-up. Spine. 2009;34:1693-1698.
95 Bridwell KH, Glassman S, Horton W, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: A prospective multicenter evidence-based medicine study. Spine. 2009;34:2171-2178.
96 Li G, Passias P, Kozanek M, et al. Adult scoliosis in patients over sixty-five years of age: Outcomes of operative versus nonoperative treatment at a minimum two-year follow-up. Spine. 2009;34:2165-2170.
97 Smith JS, Shaffrey CI, Berven S, et al. Spinal Deformity Study Group: Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery. 2009;65:86-93.
98 Slover J, Abdu WA, Hanscom B, et al. The impact of comorbidities on the change in short-form 36 and Oswestry scores following lumbar spine surgery. Spine. 2006;31:1974-1980.
99 Hu SS, Berven SH. Preparing the adult deformity patient for spinal surgery. Spine. 2006;31(19 Suppl):S126-S131.
100 Bowen RM. Respiratory management in scoliosis. In: Lonstein JE, Bradford DS, Winter RB, et al, editors. Moe’s Textbook of Scoliosis and Other Spinal Deformities. Philadelphia: WB Saunders; 1995:572-580.
101 Padman R, McNamara R. Postoperative pulmonary complications in children with neuromuscular scoliosis who underwent posterior spine fusion. Del Med J. 1990;62:999.
102 Hu SS, Berven SH. Preparing the adult deformity patient for spinal surgery. Spine. 2006;31(19 Suppl):S126-S131.
103 Lenke LG, Betz RR, Haher TR, et al. Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis: curve classification, operative approach, and fusion levels. Spine. 2001;26:2347-2353.
104 Berven SH, Deviren V, Mitchell B, et al. Operative management of degenerative scoliosis: an evidence-based approach to surgical strategies based on clinical and radiographic outcomes. Neurosurg Clin N Am. 2007;18:261-272.
105 Akbarnia BA, Ogilvie JW, Hammerberg KW. Debate: Degenerative Scoliosis: To operate or not to operate. Spine (Phila Pa 1976). 2005;31(19 Suppl):S195-S201.
106 Weinstein, sport study on stenosis
108 Frazier DD, et al: Spine 1997
109 Polly DWJr, Hamill CL, Bridwell KH. Debate: to fuse or not to fuse to the sacrum, the fate of the L5-S1 disc. Spine. 2006;31(19 Suppl):S179-S184.
110 Shufflebarger H, Suk SI, Mardjetko S. Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: Stopping at T10 versus L1. Spine (Phila Pa 1976). 2006;31(19 Suppl):S185-S194.
111 Wigh RE. The thoracolumbar and lumbosacral transitional junctions. Spine. 1980;5:215-222.
112 Kwon BK, Elgafy H, Keynan O, et al. Progressive junctional kyphosis at the caudal end of lumbar instrumented fusion: Etiology, predictors, and treatment. Spine. 2006 Aug;31:1943-1951.
113 Lowe TG, Lenke L, Betz R, et al. Distal junctional kyphosis of adolescent idiopathic thoracic curves following anterior or posterior instrumented fusion: Incidence, risk factors, and prevention. Spine. 2006 Feb 1;31:299-302.
114 Frez R, Cheng JC, Wong EM. Longitudinal changes in truncal balance after selective fusion of King II curves in adolescent idiopathic scoliosis. Spine. 2000 Jun 1;25:1352-1359.
115 Swamy G, Berven SH, Bradford DS. The selection of L5 versus S1 in long fusions for adult idiopathic scoliosis. Neurosurg Clin N Am. 2007 Apr;18:281-288.
116 Balderston RA, Winter RB, Moe JH, et al. Fusion to the sacrum for nonparalytic scoliosis in the adult. Spine. 1986 Oct;11(8):824-829.
117 Kuklo TR. Principles for selecting fusion levels in adult spinal deformity with particular attention to lumbar curves and double major curves. Spine. 2006;31(19 Suppl):S132-S138.
118 Swank S, Lonstein JE, Moe JH, Winter RB, Bradford DS. Surgical treatment of adult scoliosis. A review of two hundred and twenty-two cases. J Bone Joint Surg Am. 1981;63:268-287.
119 Simmons ED, et al: SRS 2005
120 Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: Incidence, outcomes, and risk factor analysis. Spine. 2005;30:1643-1649.
121 Shufflebarger H, Suk SI, Mardjetko S. Debate: Determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine. 2006;31(19 Suppl):S185-S194.
123 Horton WC, Holt RT, Muldowny DS. Controversy. Fusion of L5-S1 in adult scoliosis. Spine. 1996;21(21):2520-2522.
124 Polly DW: Debate: To fuse or not to fuse to the sacrum, the fate of the L5-S1 Disc. Spine 31(19S):s179–s184
125 Bridwell KH, Edwards CC, Lenke LG. The pros and cons to saving the L5-S1 motion segment in a long scoliosis fusion construct. Spine. 2003;28:S234-S242.
126 Eck KR, Bridwell KH, Ungacta FF, et al. Complications and results of long adult deformity fusions down to l4, l5, and the sacrum. Spine. 2001;26:E182-E192.
127 Edwards CC2nd, Bridwell KH, Patel A, et al. Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine. 2004;29:1996-2005.
128 Swamy G, Berven S, Bradford DS. The selection of L5 versus S1 in long fusions for adult idiopathic scoliosis. Neurosurg Clin N Am. 2007;18:281-288.
129 Edwards CC2nd, Bridwell KH, Patel A, et al. Thoracolumbar deformity arthrodesis to L5 in adults: the fate of the L5-S1 disc. Spine. 2003;28:2122-2131.
130 Reference deleted in proofs.
131 Edwards CC2nd, Bridwell KH, Patel A, et al. Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine. 2004;29:1996-2005.
132 Eck KR, Bridwell KH, Ungacta FF, et al. Complications and results of long adult deformity fusions down to l4, l5, and the sacrum. Spine. 2001;26:E182-E192.
133 Swamy G, Berven S, Bradford DS. The selection of L5 versus S1 in long fusions for adult idiopathic scoliosis. Neurosurg Clin N Am. 2007;18:281-288.
134 Betz RR, Shufflebarger H. Anterior versus posterior instrumentation for the correction of thoracic idiopathic scoliosis. Spine. 2001;26:1095-1100.
135 Lowe TG, Betz R, Lenke L, et al. Anterior single-rod instrumentation of the thoracic and lumbar spine: saving levels. Spine. 2003;28:S208-S216.
136 Good CR, Lenke LG, Bridwell KH, et al. Can posterior-only surgery provide similar radiographic and clinical results as combined anterior (thoracotomy/thoracoabdominal)/posterior approaches for adult scoliosis? Spine. 2010;35:210-218.
137 Burton DC, Asher MA, Lai SM. Patient-based outcomes analysis of patients with single torsion thoracolumbar-lumbar scoliosis treated with anterior or posterior instrumentation: an average 5- to 9-year follow-up study. Spine (Phila Pa 1976). 2002;27:2363-2367.
138 Dwyer AF, Newton NC, Sherwood AA. An anterior approach to scoliosis. A preliminary report. Clin Orthop Relat Res. 1969;62:192-202.
139 Moe JH, Purcell GA, Bradford DS. Zielke instrumentation (VDS) for the correction of spinal curvature. Analysis of results in 66 patients. Clin Orthop Relat Res. 1983;180:133-153.
140 Hammerberg KW, Rodts MF, DeWald RL. Zielke instrumentation. Orthopedics. 1988;11:1365-1371.
141 Kostuik JP, Carl A, Ferron S. Anterior Zielke instrumentation for spinal deformity in adults. J Bone Joint Surg Am. 1989;71:898-912.
142 Engsberg JR, Lenke LG, Uhrich ML, et al. Prospective comparison of gait and trunk range of motion in adolescents with idiopathic thoracic scoliosis undergoing anterior or posterior spinal fusion. Spine. 2003;28:1993-2000.
143 Smith JA, Deviren V, Berven S, Bradford DS. Does instrumented anterior scoliosis surgery lead to kyphosis, pseudarthrosis, or inadequate correction in adults? Spine. 2002;27:529-534.
144 Deviren V, Patel VV, Metz LN, et al. Anterior arthrodesis with instrumentation for thoracolumbar scoliosis: comparison of efficacy in adults and adolescents. Spine. 2008;33:1219-1223.
145 Suk SI, Lee CK, Chung SS. Comparison of Zielke ventral derotation system and Cotrel-Dubousset instrumentation in the treatment of idiopathic lumbar and thoracolumbar scoliosis. Spine. 1994;19:419-429.
146 Halm H, Niemeyer T, Link T, Liljenqvist U. Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur Spine J. 2000;9:191-197.
147 Good CR, Lenke LG, Bridwell KH, et al. Can posterior-only surgery provide similar radiographic and clinical results as combined anterior (thoracotomy/thoracoabdominal)/posterior approaches for adult scoliosis? Spine. 2010;35:210-218.
148 Geck MJ, Rinella A, Hawthorne D, et al. Comparison of surgical treatment in Lenke 5C adolescent idiopathic scoliosis: anterior dual rod versus posterior pedicle fixation surgery: a comparison of two practices. Spine. 2009;34:1942-1951.
149 Bradford DS, Ahmed KB, Moe JH, et al. The surgical management of patients with Scheuermann’s disease: a review of twenty-four cases managed by combined anterior and posterior spine fusion. J Bone Joint Surg Am. 1980;62:705-712.
150 Kostuik JP. Treatment of scoliosis in the adult thoracolumbar spine with special reference to fusion to the sacrum. Orthop Clin North Am. 1988;19:371-381.
151 Johnson JR, Holt RT. Combined use of anterior and posterior surgery for adult scoliosis. Orthop Clin North Am. 1988;19:361-370.
152 Bridwell KH. Normalization of the coronal and sagittal profile in idiopathic scoliosis: options of treatment. J Orthop Sci. 1998;3:125-134.
153 Berven SH, Deviren V, Smith JA, et al. Management of fixed sagittal plane deformity: outcome of combined anterior and posterior surgery. Spine. 2003;28:1710-1715.
154 Floman Y, Micheli LJ, Penny JN, et al. Combined anterior and posterior fusion in seventy-three spinally deformed patients: indications, results and complications. Clin Orthop Relat Res. 1982;164:110-122.
155 McDonnell MF, Glassman SD, Dimar JR2nd, Puno RM, Johnson JR. Perioperative complications of anterior procedures on the spine. J Bone Joint Surg Am. 1996;78:839-847.
156 Weis JC, Betz RR, Clements DH3rd, Balsara RK. Prevalence of perioperative complications after anterior spinal fusion for patients with idiopathic scoliosis. J Spinal Disord. 1997;10:371-375.
157 Shapiro GS, Taira G, Boachie-Adjei O. Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: A study of long-term clinical radiographic outcomes. Spine. 2003;28:358-363.
158 Lapp MA, Bridwell KH, Lenke LG, et al. Long-term complications in adult spinal deformity patients having combined surgery a comparison of primary to revision patients. Spine. 2001;26:973-983.
159 Kim YB, Lenke LG, Kim YJ, et al. The morbidity of an anterior thoracolumbar approach: Adult spinal deformity patients with greater than five-year follow-up. Spine. 2009;34:822-826.
160 Anand N, Baron EM, et al. Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: A technique and feasibility study. J Spinal Disord Tech. 2008;21:459-467.
161 Lippman CR, Spence CA, Youssef AS, Cahill DW. Correction of adult scoliosis via a posterior-only approach. Neurosurg Focus. 2003;14:e5.
162 Crandall DG, Revella J. Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: Three year clinical and radiographic outcomes. Spine. 2009;34:2126-2133.
163 Maeda T, Buchowski JM, Kim YJ, et al. Long adult spinal deformity fusion to the sacrum using rhBMP-2 versus autogenous iliac crest bone graft. Spine. 2009;34:2205-2212.
164 Lee SS, Lenke LG, Kuklo TR, et al. Comparison of Scheuermann kyphosis correction by posterior-only thoracic pedicle screw fixation versus combined anterior/posterior fusion. Spine. 2006;31:2316-2321.
165 Burton DC, Sama AA, Asher MA, et al. The treatment of large (>70 degrees) thoracic idiopathic scoliosis curves with posterior instrumentation and arthrodesis: When is anterior release indicated? Spine. 2005;30:1979-1984.
166 Suk SI, Kim JH, Cho KJ, et al. Is anterior release necessary in severe scoliosis treated by posterior segmental pedicle screw fixation? Eur Spine J. 2007;16:1359-1365.
167 Kim YB, Lenke LG, Kim YJ, et al. Surgical treatment of adult scoliosis: Is anterior apical release and fusion necessary for the lumbar curve? Spine. 2008;33:1125-1132.
168 Pateder DB, Kebaish KM, Cascio BM, et al. Posterior only versus combined anterior and posterior approaches to lumbar scoliosis in adults: A radiographic analysis. Spine. 2007;32:1551-1554.
169 Dobbs MB, Lenke LG, Kim YJ, et al. Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90 degrees. Spine. 2006;31:2386-2391.
170 Boachie-Adjei O, Bradford DS. Vertebral column resection and arthrodesis for complex spinal deformities. J Spinal Disord. 1991;4:193-202.
171 Suk SI, Kim JH, Kim WJ, et al. Posterior vertebral column resection for severe spinal deformities. Spine. 2002;27:2374-2382.
172 Lenke LG, Sides BA, Koester LA, et al. Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res. 2010;468:687-699.
173 MacEwen GD, Bunnell WP, Sriram K. Acute neurological complications in the treatment of scoliosis. J Bone Joint Surg. 1975;57A:404-411.
174 Winter RB. Neurologic safety in spinal deformity surgery. Spine. 1997;22:1527-1533.
175 Thompson GH, Wilbur RG, Shaffer JW, et al. Segmental spinal instrumentation in idiopathic scoliosis: A preliminary report. Spine. 1985;10:623-630.
176 Wilburg G, Thompson GH, Shaffer JW, et al. Postoperative neurological deficits in segmental spinal instrumentation. J Bone Joint Surg [Am]. 1984;66:1178-1187.
177 Zielke K, Pellen B. The neurological risk of Harrington procedures. Arch Orthop Unfall Chir. 1975;83:311-322.
178 Bridwell KH, Lenke LG, Baldus C, Blanke K. Major intraoperative neurologic deficits in pediatric and adult spinal deformity patients. Spine. 1998;23:324-331.
179 Vauzelle C, Stagnara P, Jouviroux P. Functional monitoring of spinal activity during spinal surgery. Clin Orthop. 1973;93:173-178.
180 Brustowicz RM, Hall JE. In defense of the wake-up test. Anesth Analg. 1988;67:1019.
181 Pelosi L, Lamb J, Grevitt M, et al. Combined monitoring of motor and somatosensory evoked potentials in orthopaedic spinal surgery. Clin Neurophysiol. 2002;113:1082-1091.
182 McAfee PC. Complications of anterior approaches to the thoracolumbar spine. Emphasis on Kaneda Instrumentation. Clin Orthop. 1994;306:110-119.
183 McAfee PC, Regan JR, Zdeblick T, et al. The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery. A prospective multicenter study comprising the first 100 cases. Spine. 1995;20:1624-1632.
184 Baker JK, Reardon PR, Reardon MJ, Heggeness MH. Vascular injury in anterior lumbar surgery. Spine. 1993;18:2227-2230.
185 Rajaraman V, Vingan R, Roth P, et al. Visceral and vascular complications resulting from anterior lumbar interbody fusion. J Neurosurg. 1999;91(1 Suppl):60-64.
186 Bianchi C, Ballard JL, Abou-Zamzam AM, et al. Anterior retroperitoneal lumbosacral spine exposure: Operative technique and results. Ann Vasc Surg. 2003;17:137-142.
187 Oskouian RJJr, Johnson JP. Vascular complications in anterior thoracolumbar spinal reconstruction. J Neurosurg. 2002;96(1 Suppl):1-5.
188 Lieberman IH, Willsher PC, Litwin DE, et al. Transperitoneal laparoscopic exposure for lumbar interbody fusion. Spine. 2000;25:509-514. discussion, 515
189 Regan JJ, Aronoff RJ, Ohnmeiss DD, Sengupta DK. Laparoscopic approach to L4-L5 for interbody fusion using BAK cages: Experience in the first 58 cases. Spine. 1999;24:2171-2174.
190 Goodkin R, Laska LL. Vascular and visceral injuries associated with lumbar disc surgery: Medicolegal implications. Surg Neurol. 1998;49:358-370. discussion 370-372
191 Papadoulas S, Konstantinou D, Kourea HP, et al. Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg. 2002;24:189-195.
192 Raskas DS, Delamarter RB. Occlusion of the left iliac artery after retroperitoneal exposure of the spine. Clin Orthop. 1997;338:86-89.
193 Kulkarni SS, Lowery GL, Ross RE, et al. Intimal injury and thrombosis of the iliac vessels is a significant problem in older patients with arteriosclerotic disease. Eur Spine J. 2003;12:48-54.
194 Glotzbecker MP, Bono CM, Wood KB, Harris MB. Thromboembolic disease in spinal surgery: a systematic review. Spine. 2009;34:291-303.
195 Dearborn JT, Hu SS, Tribus CB, Bradford DS. Thromboembolic complications after major thoracolumbar spine surgery. Spine. 1999;24:1471-1476.
196 Bono CM, Watters WC3rd, Heggeness MH, et al. An evidence-based clinical guideline for the use of antithrombotic therapies in spine surgery. Spine J. 2009;9:1046-1051.
197 Lapp MA, Bridwell KH, Lenke LG, et al. Long-term complications in adult spinal deformity patients having combined surgery: A comparison of primary to revision patients. Spine. 2001;26:973-983.
198 Mok JM, Guillaume TJ, Talu U, et al. Clinical outcome of deep wound infection after instrumented posterior spinal fusion: A matched cohort analysis. Spine (Phila Pa 1976). 2009;34:578-583.
199 Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am. 2006;88:721-728.
200 Emami A, Deviren V, Berven S, et al. Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque-Galveston, combined iliac and sacral screws, and sacral fixation. Spine. 2002;27:776-786.
201 Rinella A, Bridwell K, Kim Y, et al. Late complications of adult idiopathic scoliosis primary fusions to L4 and above: The effect of age and distal fusion level. Spine. 2004;29:318-325.
202 Helgeson MD, Shah SA, Newton PO, et al. Harms Study Group: Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine. 2010;35:177-181.
203 Schwab FJ, Lafage V, Farcy JP, et al. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine. 2008;33:2243-2247.