Chapter 7 Adult congenital heart disease
Introduction
Congenital heart disease has an incidence of approximately 1% (Figure 7.1). Advances in medical and surgical management have resulted in a growing population of young adults who require continued care due to the predominantly palliative rather than curative nature of their interventions. CMR provides safe serial assessment of patients with adult congenital heart disease (ACHD).
CMR images and measurements complement those obtained using echocardiography, especially in postoperative patients. Accurate anatomical and functional information of complex cardiac pathology can be obtained in any plane. These factors make pre- and post-intervention CMR evaluation in ACHD invaluable.
CMR protocol
Other reporting requirements are highlighted following discussion of specific conditions.
Cardiac morphology and function
Subsequent cines are acquired in planes determined by the underlying diagnosis and provide higher resolution anatomical and functional information on parameters including biventricular size, function and mass. Assessment of the RV and pulmonary vasculature is of particular importance in ACHD along with extensive flow velocity mapping for measurement of peak velocities, regurgitant fractions and shunt performance (Figure 7.2). The Venc is set to account for low velocities in venous systems and higher velocities within shunts. Information from both the cines and velocity mapping is crucial for interpretation of the patterns of blood flow. Cine images also direct optimal positioning of velocity mapping sequences.
CMR in specific ACHD
Congenital heart disease is usually recognized in childhood and the most frequent use of CMR is in the assessment of patients with an established diagnosis.
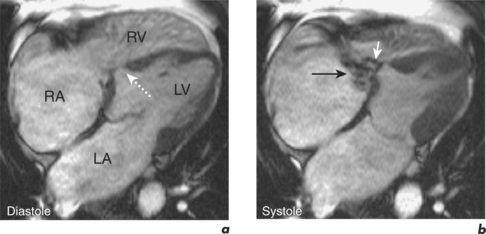
Ventricular septal defect
VSDs are the most common congenital heart defects. They range from small haemodynamically insignificant and isolated lesions to large defects associated with multiple cardiac anomalies such as in TOF. CMR is complementary to echocardiography in the assessment of simple and complex VSDs. It allows multiplanar visualization of the spatial relationship of the defect to surrounding structures, can diagnose concurrent cardiac pathology and their functional sequelae, and quantify shunt size and effect on the RV and PAs. SE imaging en-face and parallel to the VSD provides anatomical information. SSFP cines show signal loss in the RV due to blood flow through the VSD and are useful in assessing the shape and dimensions of the defect (Figure 7.3). Shunt ratio can be calculated in two ways: firstly, comparison of pulmonary to systemic flow (Qp:Qs) obtained by velocity mapping CMR, and secondly, from the difference in ventricular SV obtained from the ventricular short-axis stack of cines (Figure 7.4).
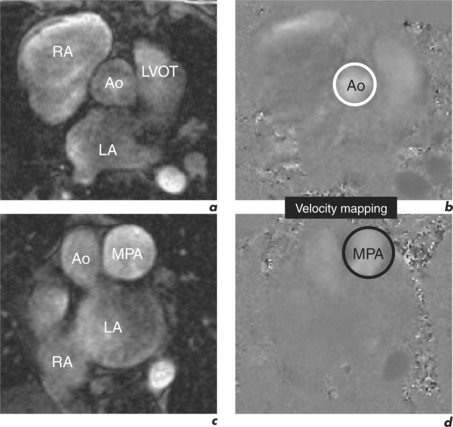
Figure 7.4 Calculation of Qp:Qs for the VSD case presented in Figure 7.3 using velocity mapping CMR.
Specific reporting features in the CMR assessment of VSD are therefore:
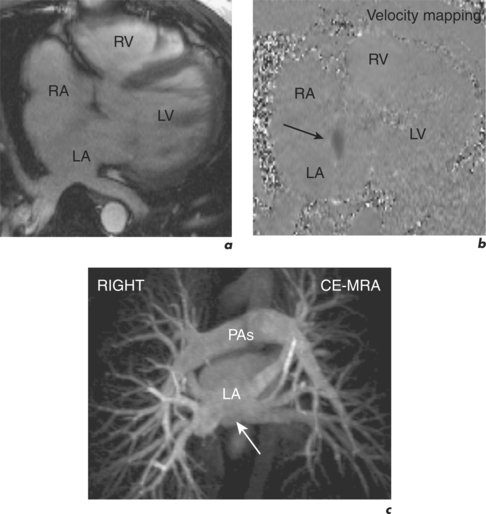
Atrial septal defect
There are three types of ASDs, all of which can present initially in adulthood. The commonest defect is the ostium secundum defect (75%) in the area of the foramen ovale. Echocardiography is first line for the diagnosis of ASD. CMR is used where echocardiography is suboptimal, identifying the defect through visualization of low signal on the right side of the atrial septum on SSFP cines. CMR quantifies shunt size, determines the anatomical and functional effects of the shunt, and accurately identifies anomalous pulmonary venous drainage (APVD; Figure 7.5).
Partial anomalous pulmonary venous drainage and major aortopulmonary collateral arteries
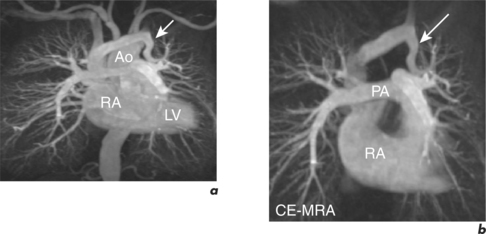
CMR has a useful role in the detection and serial evaluation of extracardiac venous and arterial vascular anomalies in ACHD, such as partial anomalous pulmonary venous drainage (PAPVD) and major aortopulmonary collateral arteries (MAPCAs). CMR imaging protocols in PAPVD and MAPCAs incorporate MRA for optimal detection of vessels and this often provides additional information to findings at cardiac catheterization as well as confirming the diagnosis (Figure 7.6). Velocity mapping quantifies shunt sizes, and SE techniques can surmount image artefact from endovascular coils.
Pulmonary stenosis, right ventricular outflow tract and conduit obstruction
In contrast to the assessment of ASD and VSD, the RVOT and conduits from the RV to the PA are often poorly visualized by echocardiography. CMR provides detailed imaging of the level and anatomy of RVOT obstruction with SE and SSFP cine imaging in orthogonal planes. Serial, contiguous cines in the transaxial plane are useful for functional assessment of extracardiac ventriculopulmonary shunts, such as the Rastelli shunt. Velocity mapping quantifies severity of stenosis or regurgitation and may be used at valve level, within the MPA, or separately within the right and left PAs (Figure 7.7). CE-MRA is an excellent noninvasive method of assessing branch pulmonary stenoses and identification of MAPCAs.
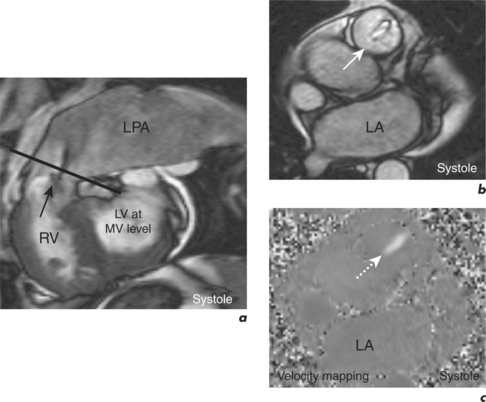
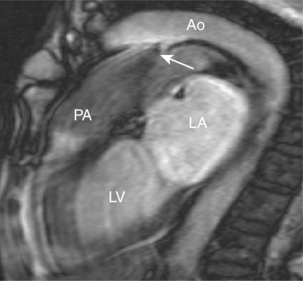
Patent ductus arteriosus and aortopulmonary window
PDA describes persistent arterial communication between the proximal LPA and descending thoracic aorta distal to the origin of the left subclavian artery. It is usually an isolated lesion in adults. Flow through a PDA is detectable on cines, which show turbulence in the anterior portion of the PA proximal to its bifurcation (Figure 7.8). CMR can quantify shunt size and evaluate signs of pulmonary hypertension prior to decisions regarding device closure.
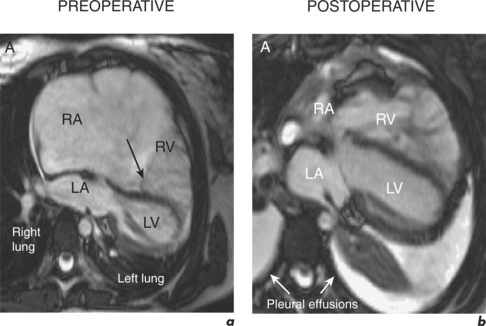
Ebstein anomaly
The diagnosis of Ebstein’s anomaly is usually made on echocardiography but CMR has a role in defining anatomy and identifying those requiring and suitable for surgical correction (Figure 7.9). Apical displacement of the septal and mural leaflets of the tricuspid valve (TV) is identified on long-axis cines. Serial short-axis cines assess enlargement of the anterior leaflet and degree of TV dysplasia, and are later analysed to provide volumetric and functional data on the RA and RV. Velocity mapping CMR is usually performed in order to quantify the degree of TR, but is occasionally also used to quantify the severity of TS. Both SSFP cines and velocity mapping are used to evaluate the presence of abnormal atrial communication.
Tetralogy of Fallot
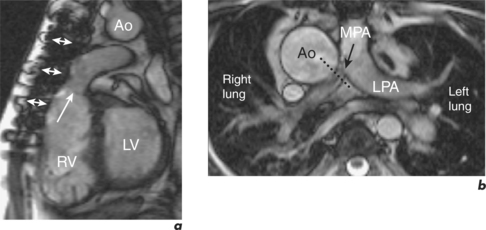
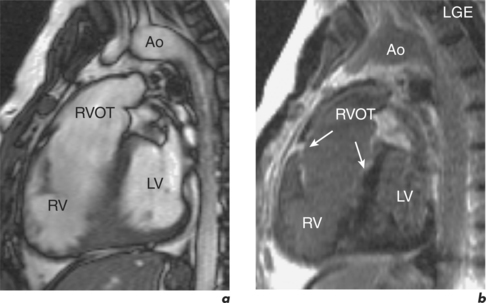
TOF comprises VSD, RVOT obstruction, RVH and an overriding aorta. Definitive repair includes VSD patch closure and resection of RVOT obstruction, with older patients often having prior palliative shunt procedures such as the Blalock–Taussig (subclavian to PA anastomosis) shunt. Reconstruction of the RVOT leads to important PR and serial assessments of regurgitation and the RV are crucial following repair. Other postoperative complications, such as aneurysm formation in the RVOT and dilatation of the aortic root, as well as co-existing congenital anomalies, including right-sided aortic arch and aberrant coronary anatomy, can often be identified at the initial orthogonal multislice FSE sequences and are then further characterized with higher resolution SSFP sequences.
LGE in the RV and LV is common following TOF repair and is related to adverse clinical markers including ventricular dysfunction. In particular, RV enhancement predicts arrhythmia which has potential prognostic implications (Figure 7.10).
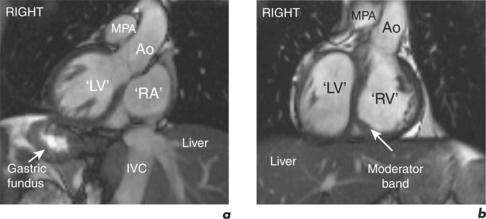
Corrected transposition of the great arteries
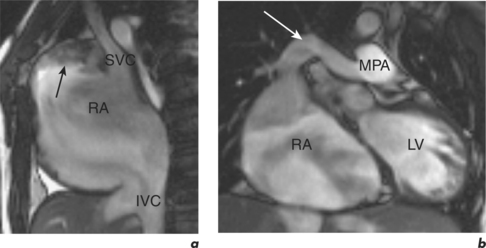
In transposition of the great arteries (TGA) the aorta arises from the RV and the PA arises from the LV. Almost all surviving adults with TGA have undergone operative correction in childhood, either removal of the atrial septum and insertion of a baffle (Mustard operation) or folding of the atrial wall (Senning operation), to redirect atrial flow but leaving the transposed ventriculoarterial connections. The primary aim in postoperative imaging is assessment of pulmonary and systemic venous flow pathways (Figure 7.11). CMR readily identifies stenoses and baffle leaks with subsequent multiplanar and multislice evaluation allowing anatomical clarification and accurate quantification. SSFP cines are acquired to visualize each pathway in order to identify narrowing or signal loss due to turbulence. Through-plane velocity mapping is then used to identify flow velocities above 1 m/s, indicative of flow obstruction at atrial level. Dilatation of the azygous and hemi-azygous veins is a useful pointer to significant systemic venous pathway obstruction.
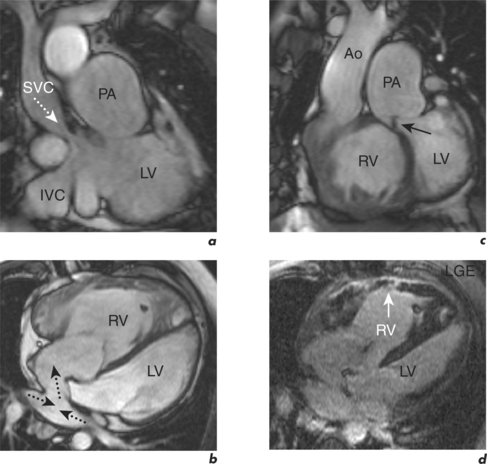
Figure 7.11 Part of the CMR evaluation in a 30-year-old man who had undergone a Mustard operation for TGA aged 2 months.
Patients who have undergone corrective arterial switch operations require assessment of supravalvular PS or AS and branch PA stenoses. Such patients are also at risk of ostial coronary artery stenoses at the site of coronary artery reimplantation, and these can also be evaluated by CMR.
Univentricular hearts and Fontan repair
In patients with one effective ventricle, the Fontan operation routes systemic venous return directly into the PAs leaving the ventricle to pump oxygenated blood to the systemic circulation. Pulmonary blood flow is dependent on elevated pressure within the systemic veins and any obstruction to flow, such as with thrombus, makes the circuit fail. Contemporary repair involves total cavopulmonary connection, usually by an atrial tunnel or extracardiac conduit. CMR is invaluable in the assessment of such shunts since echocardiography is often limited by the retrosternal position of the connection. Targeted SSFP cines of the connection identify obstruction as signal loss from turbulent blood flow. These acquisitions are also early indicators of RA thrombus formation, which should later be confirmed or refuted using EGE (Figure 7.12). Cine imaging is extended to the pulmonary veins to exclude post-operative compression, with through-plane flow velocities above 1 m/s coinciding with atrial systole being suggestive of obstruction. Serial, contiguous short-axis SSFP cines allow determination of univentricular function and since only one SV value is available, quantification of atrioventricular valve regurgitation requires velocity mapping at the aorta and MPA.
Specific CMR reporting comments for the Fontan circuit are on: