CHAPTER 14 Adrenalectomy
Step 1. Surgical anatomy
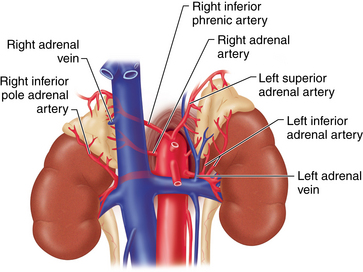
♦ The adrenal glands are located at the superior-medial aspect of each kidney and are composed of a cortex and medulla with distinct endocrine functions. The steroid hormones (cortisol, aldosterone, and the adrenal androgens) are synthesized and secreted in the adrenal cortex, and the adrenal medulla synthesizes the catecholamines, norepinephrine and epinephrine. Catecholamines may also be synthesized in extra-adrenal chromaffin tissue in the paraganglia.
♦ Each adrenal gland is embedded in Gerota’s fascia and is surrounded by retroperitoneal fat. The adrenal gland has a golden yellow appearance because of the high lipid content of the cortex.
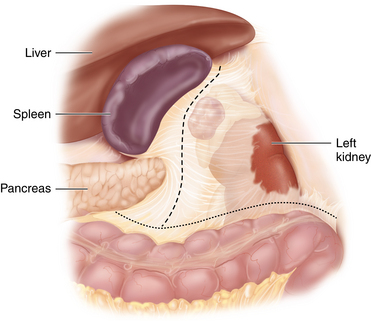
♦ The right adrenal gland is pyramidal in shape and lies superior to the right kidney, whereas the left adrenal is more flattened and is in intimate contact with the medial aspect of the superior pole of the left kidney.
♦ Bordering structures for the right adrenal are the inferior vena cava medially, the liver anteriorly, and the kidney inferiorly. A portion of the anteromedial border of the gland usually extends posterior to the vena cava. The right triangular ligament of the liver crosses the anterior surface of the adrenal gland superiorly, which means that the upper portion of the gland has no peritoneum covering its surface. Structures that border the posterior aspect of the right adrenal are the diaphragm superiorly and the anteromedial portion of the superior pole of the right kidney inferiorly.
♦ Structures neighboring the left adrenal gland are the spleen and fundus of the stomach superiorly, the splenic flexure of the colon, the tail of pancreas, and splenic vessels inferiorly, and the left crus of the diaphragm posteromedially and the medial aspect of the left kidney posterolaterally. The renal vessels lie just below the inferior border of the adrenal, and in the setting of a large tumor, they may overlie the renal artery and vein.
♦ The adrenal blood supply is derived from numerous branches of the inferior phrenic, aortic, and renal arteries. A single central vein drains each adrenal.
 The right adrenal vein is short (0.5 to 1 cm in length) and runs from the medial aspect of the gland directly into the posterolateral aspect of the inferior vena cava. A second right adrenal vein may occasionally enter either the vena cava or right hepatic vein more superiorly.
The right adrenal vein is short (0.5 to 1 cm in length) and runs from the medial aspect of the gland directly into the posterolateral aspect of the inferior vena cava. A second right adrenal vein may occasionally enter either the vena cava or right hepatic vein more superiorly. The left adrenal vein is longer than on the right (2 to 3 cm in length) and is found at the inferior-medial aspect of the gland, where it runs obliquely to empty into the left renal vein. The inferior phrenic vein typically joins the left adrenal vein proximal to its entry into the renal vein (Figure 14-1).
The left adrenal vein is longer than on the right (2 to 3 cm in length) and is found at the inferior-medial aspect of the gland, where it runs obliquely to empty into the left renal vein. The inferior phrenic vein typically joins the left adrenal vein proximal to its entry into the renal vein (Figure 14-1).Step 2. Preoperative considerations
♦ Most indications for adrenalectomy today are appropriate for a laparoscopic approach. The only absolute contraindication for laparoscopic adrenalectomy is an adrenal malignancy with evidence of local invasion or involved regional lymph nodes. However, surgeons should be cautious in approaching large tumors laparoscopically for a number of reasons: (1) large tumors are more difficult to remove, (2) the tumor is more likely to be malignant (especially adrenal cortical lesions >6 cm in size), and (3) the surgeon should be highly experienced in laparoscopic adrenalectomy.
♦ All patients undergoing adrenalectomy should have completed a biochemical evaluation to assess for a functioning tumor. The minimal workup should consist of the following:
 Plasma fractionated metanephrines or 24-hour urine catecholamines and metanephrines to exclude a pheochromocytoma
Plasma fractionated metanephrines or 24-hour urine catecholamines and metanephrines to exclude a pheochromocytomaPreoperative preparation for adrenalectomy should entail the following:
♦ Control of hypertension and correction of any electrolyte abnormalities.
♦ Pharmacologic preparation of patients with pheochromocytomas with alpha-adrenergic blockade for 7 to 10 days preoperatively to mitigate against hypertensive exacerbations intraoperatively. Most commonly, phenoxybenzamine is used starting at 10 mg twice daily, with the dose increasing until hypertension and tachycardia are controlled and the patient is mildly orthostatic.
Equipment and instrumentation
Anesthesia
♦ Our usual protocol includes a single dose of first-generation cephalosporin prior to skin incision.
♦ A nasogastric tube is usually unnecessary.
♦ A Foley catheter is only used in patients in whom a longer procedure is expected (i.e., for pheos and large tumors over 5 cm).
♦ Stress-dose steroids are administered for patients with Cushing syndrome or those undergoing bilateral adrenalectomy. Steroids are tapered to maintenance doses early postoperatively and are continued until recovery of the pituitary-adrenal axis.
Room setup and patient positioning
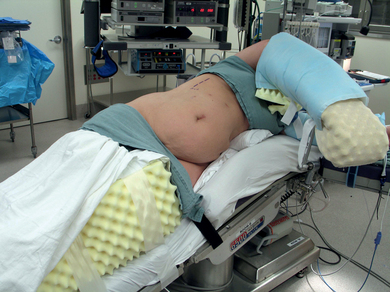
♦ The transabdominal lateral flank approach is the most commonly utilized laparoscopic approach. Some centers favor a direct retroperitoneal endoscopic approach with the patient in a prone position.
♦ Sequential steps in the transabdominal lateral approach are as follows:
Step 3. Operative steps
Access and port placement
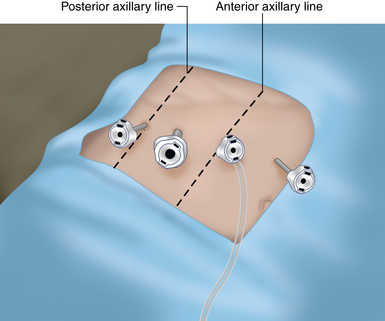
♦ Initial access is obtained by closed Veress needle insertion and insufflation in the subcostal region just medial to the anterior axillary line. An optical 5-mm trocar is used for initial access, and the other ports are placed under direct laparoscopic visualization. Alternatively, an open insertion technique can be used (Figure 14-3).
♦ The ports should be at least 5 cm apart to allow external freedom of movement. One of the ports is 10 to 12 mm in size (usually the midaxillary port) for insertion of the clip applier and specimen extraction, and the others are 5 mm in diameter.
Right adrenalectomy
Dissection of medial border of the adrenal
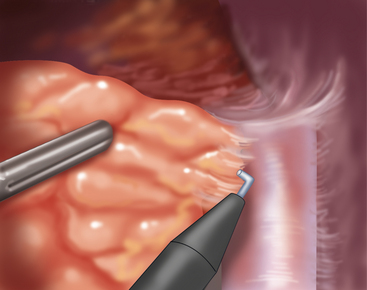
The peritoneum between the liver and the right adrenal is incised and the plane is developed between the adrenal and the inferior vena cava. The adrenal is gently retracted medially and small arterial branches to the middle and upper adrenal are hooked and cauterized. The adrenal vein should come into view early in the dissection (Figure 14-4).
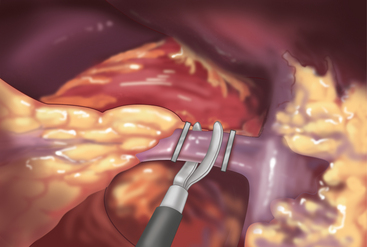
Division of right adrenal vein
The adrenal vein is isolated, clipped, and divided. A right-angle dissector is used to get around the vein. The vein is short and care must be taken to not exert much traction on it as it may tear at its junction with the vena cava (Figure 14-5).
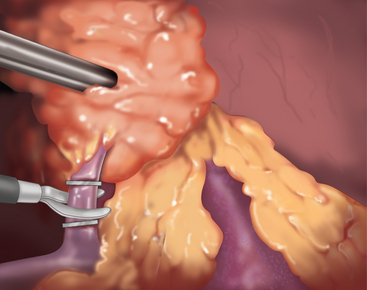
Inferior adrenal dissection
The medial border of the adrenal is freed up down to the underlying back muscle, and the dissection is extended inferiorly. The inferior portion of the adrenal sits on top of the kidney and extends toward the renal vessels. The dissection is carried inferiorly and then laterally out over the superior pole of the kidney, dividing the perinephric fat. Either a hook cautery or an ultrasonic device may be used for this portion of the dissection, and clips are applied to any larger vessels. The dissection should stay close to the inferior adrenal pole because of the proximity of the renal hilum and superior pole arterial branches (Figure 14-6).
Left adrenalectomy
Take down of splenic flexure of colon
The first step in left adrenalectomy is mobilization of the splenic flexure of the colon. This should be released from the lateral abdominal reflection all the way to the inferior pole of the spleen (Figure 14-7).
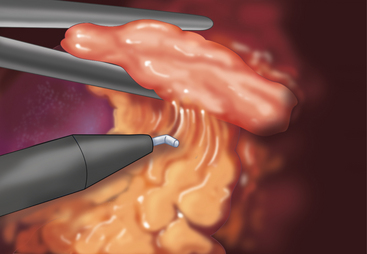
Isolation and division of left adrenal vein
The adrenal vein exits the adrenal obliquely at the inferior-medial border of the gland. The surrounding small vessels and connective tissue are dissected with the hook cautery and the vein is isolated with a right angle dissector. It is clipped and then divided (Figure 14-8).
Step 4. Postoperative care
♦ Day of surgery: Patients are admitted to a regular nursing unit and are started on a liquid diet once they are awake and alert. Exceptions are patients with vasoactive pheochromocytomas who may require a period of postoperative pressor support with arterial line monitoring, in which case they should be monitored in an intensive care unit setting.
♦ Postoperative day 1: Serum electrolytes and creatinine are obtained and the diet is advanced. Patients may be discharged once blood pressure is stable and they are tolerating a regular diet. Some patients may require longer in-hospital monitoring for blood pressure management or adjustments in hormone replacement.
♦ Patients with Cushing syndrome should receive perioperative stress steroids tapered rapidly to maintenance levels. For bilateral adrenalectomy, patients should receive both prednisone and mineralocorticoid replacement with fludrocortisone (0.1 mg/dL).
♦ Patients with aldosteronomas should have the spironolactone stopped, and other antihypertensive medications should be continued and subsequently adjusted or discontinued as clinically indicated.
Step 5. Pearls and pitfalls
♦ Surgeons who undertake adrenalectomy should be well versed in the biochemical evaluation of adrenal tumors and in options for adrenal imaging.
♦ A thorough knowledge of adrenal anatomy and relationships of surrounding structures is essential to successful adrenalectomy.
♦ A gentle, meticulous dissection technique should be used to minimize operative bleeding, to maintain clear dissection planes, and to avoid fracturing the adrenal capsule or tumor.
♦ Difficult cases (pheochromocytoma, obese patients, those with large tumors) should be avoided early in one’s experience with adrenalectomy.
♦ Large, malignant adrenal cortical cancers should be removed in an open fashion.
Brunt LM. Minimal access adrenal surgery. Surg Endosc. 2006;20(3):351-361.
Brunt LM, Moley JF. Adrenal incidentaloma. In: Cameron JL, editor. Current Surgical Therapy. ed 9. St. Louis: Mosby; 2008:597-602.
Duh Q-Y, Inabnet WB, Brunt LM. SAGES Grand Rounds Master Series Episode VII: Adrenal Tumors. Woodbury, CT: SAGES—Cine-Med. 2008.
Tessier D, Brunt LM. Laparoscopic adrenalectomy. In: Soper NJ, Swanstrom LL, Eubanks WS, editors. Mastery of Endoscopic and Laparoscopic Surgery. 3rd ed. Philadelphia, Lippincott: Williams & Wilkins; 2009:410-420.