Chapter 422 Acyanotic Congenital Heart Disease
Regurgitant Lesions
422.1 Pulmonary Valvular Insufficiency and Congenital Absence of the Pulmonary Valve
Congenital absence of the pulmonary valve is usually associated with a ventricular septal defect, often in the context of tetralogy of Fallot (Chapter 424.1). In many of these neonates, the pulmonary arteries become widely dilated and compress the bronchi, with subsequent recurrent episodes of wheezing, pulmonary collapse, and pneumonitis. The presence and degree of cyanosis are variable. Florid pulmonary valvular incompetence may not be well tolerated, and death may occur from a combination of bronchial compression, hypoxemia, and heart failure. Correction involves plication of the massively dilated pulmonary arteries, closure of the ventricular septal defect, and placement of a homograft across the right ventricular outflow tract.
McDonnell BE, Raff GW, Gaynor JW, et al. Outcome after repair of tetralogy of Fallot with absent pulmonary valve. Ann Thorac Surg. 1999;67:1391-1395.
Pinsky WW. Absent pulmonary valve syndrome. In: Garson A, Bricker JT, Fisher DJ, et al, editors. The science and practice of pediatric cardiology. Baltimore: Williams & Wilkins; 1998:1413-1419.
422.2 Congenital Mitral Insufficiency
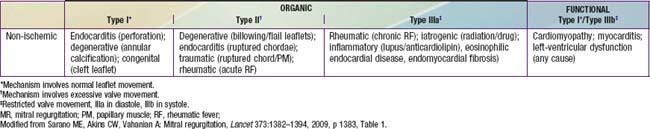
Congenital mitral insufficiency is rare as an isolated lesion and is more often associated with other anomalies. It is most commonly encountered in combination with an atrioventricular septal defect, either an ostium primum defect, or a complete AV septal defect (Chapter 420.5). Mitral insufficiency is also seen in patients with dilated cardiomyopathy (Chapter 433.1) as their left ventricular function deteriorates, secondary to dilatation of the valve ring. Mitral insufficiency may also be encountered in conjunction with coarctation of the aorta, ventricular septal defect, corrected transposition of the great vessels, anomalous origin of the left coronary artery from the pulmonary artery, or Marfan syndrome. In the absence of other congenital heart disease, endocarditis or rheumatic fever should be suspected in a patient with isolated severe mitral insufficiency (Table 422-1).
422.3 Mitral Valve Prolapse
This lesion is not progressive in childhood, and specific therapy is not indicated. Antibiotic prophylaxis is no longer recommended during surgery and dental procedures (Chapter 431).
American Academy of Pediatrics Committee on Sports Medicine and Fitness. Mitral valve prolapse and athletic competition of children and adolescents. Pediatrics. 1995;95:789.
Bouknight DP, O’Rourke RA. Current management of mitral valve prolapse. Am Fam Physician. 2000;61:3343-3350. 3353–3354
Briffa N. Surgery for degenerative mitral valve disease. BMJ. 2010;341:c5339.
Hepner ADS, Morrell H, Greaves S, et al. Prevalence of mitral valve prolapse in young athletes. Cardiol Young. 2008;18:402-404.
Jacobs W, Chamoun A, Stouffer GA. Mitral valve prolapse: a review of the literature. Am J Med Sci. 2001;321:401-410.
Maron BJ, Ackerman MJ, Nishimura RA, et al. Task Force 4: HCM and other cardiomyopathies, mitral valve prolapse, myocarditis, and Marfan syndrome. J Am Coll Cardiol. 2005;45:1340-1345.
Sarano ME, Akins CW, Vahanian A. Mitral regurgitation. Lancet. 2009;373:1382-1394.
422.4 Tricuspid Regurgitation
Isolated tricuspid regurgitation is generally associated with Ebstein anomaly of the tricuspid valve. Ebstein anomaly may occur either without cyanosis or with varying degrees of cyanosis, depending on the severity of the tricuspid regurgitation and the presence of an atrial-level communication (patent foramen ovale or atrial septal defect). Older children tend to have the acyanotic form, whereas if detected in the newborn period, Ebstein anomaly is usually associated with severe cyanosis (Chapter 424.7).
Ben Sivarajan V, Chrisant MR, Ittenbach RF, et al. Prevalence and risk factors for tricuspid valve regurgitation after pediatric heart transplantation. J Heart Lung Transplant. 2008;27:494-500.
Sachdeva R, Fiser RT, Morrow WR, et al. Ruptured tricuspid valve papillary muscle: a treatable cause of neonatal cyanosis. Ann Thorac Surg. 2007;83:680-682.