CHAPTER 27 Acute Scaphoid Fractures in Nonunions
The scaphoid is the most frequently fractured bone in the carpus and accounts for approximately 70% of all carpal fractures.1 This fracture typically occurs in young men between the ages of 15 and 30 years.2 A scaphoid fracture is a common athletic injury, occurring most often in contact sports, particularly in football and basketball players. It is estimated that 1 of 100 college football players will sustain a fracture of the scaphoid.3 Commonly, an injured athlete continues to compete and eventually presents to the treating physician after the season is over with a scaphoid nonunion.
Acute nondisplaced fractures of the scaphoid have traditionally been managed with cast immobilization.4,5 Nondisplaced scaphoid fractures usually heal in 8 to 12 weeks when immobilized in long arm or short arm spica casts.4–6 Although cast immobilization is successful in up to 85% to 90% of cases, it must be asked what the cost is to the patient, particularly the athlete, who may not be able to tolerate a lengthy course of immobilization during the season or while actively training.4–6 Prolonged immobilization may lead to muscle atrophy, disuse osteopenia, joint contracture, and financial hardship. Until the fracture unites, the athlete may be inactive for 6 months or longer.
The duration of cast immobilization varies dramatically according to the fracture site. A fracture of the scaphoid tubercle may be healed within a period of 6 weeks, whereas a fracture of the waist of the scaphoid may require immobilization for 3 months or longer. A fracture of the proximal third of the scaphoid may take 5 months or longer to heal with a cast because of the vascularity of the scaphoid.7 This may result in loss of an athletic scholarship or loss of employment.
Displaced scaphoids have a reported nonunion rate of up to 50%.2 Factors that decrease the prognosis for healing include the amount of displacement, associated carpal ligament instability, and delayed presentation (>4 to 6 weeks).1 Traditionally, acute displaced fractures of the scaphoid and scaphoid nonunions have been managed by open reduction and internal fixation.1,2,8–16 Complications associated with open reduction fixation include avascular necrosis, carpal instability, donor site pain, infection, screw protrusion, and reflex sympathetic dystrophy resulting from the significant soft tissue dissection that is required.4,17 The most commonly reported complication in one series was hypertrophic scarring.2 Although jigs have been designed to assist an open reduction, they frequently are difficult to apply and may necessitate further extensive surgical dissection.18
Wrist arthroscopy has revolutionized the practice of orthopedics by allowing the surgeon to examine and treat intra-articular abnormalities of the wrist joint under bright light and magnification.19 The scaphoid is well visualized from the radiocarpal and midcarpal spaces. Whipple is credited with being the first surgeon to attempt arthroscopic management of scaphoid fractures.19 His preliminary work set the stage for the current concepts and treatment by arthroscopy of these common fractures.
The indications and techniques of arthroscopic management of acute scaphoid fractures and selected nonunions are reviewed in this chapter. Arthroscopic stabilization provides direct visualization of the fracture reduction, screw insertion, and limited surgical dissection, which may allow for a greater range of motion and earlier return to competition or employment.
TREATMENT
Indications
Arthroscopic stabilization of selected scaphoid nonunions may be performed. Slade and Geissler published their radiographic classification of scaphoid nonunions (Table 27-1).20
 In type II injuries, a fibrous union is present. A minimal fracture line may be seen on plain radiographs. The lunate is not rotated, and there is no humpback deformity.
In type II injuries, a fibrous union is present. A minimal fracture line may be seen on plain radiographs. The lunate is not rotated, and there is no humpback deformity. In type III injuries, minimal sclerosis is seen at the fracture site. Sclerosis is less than 1 mm long, the lunate is not rotated, and no humpback deformity is seen.
In type III injuries, minimal sclerosis is seen at the fracture site. Sclerosis is less than 1 mm long, the lunate is not rotated, and no humpback deformity is seen. In type IV injuries, cystic formation is present. The cystic formation is between 1 and 5 mm in diameter. No humpback deformity or rotation of the lunate is seen on plain radiographs.
In type IV injuries, cystic formation is present. The cystic formation is between 1 and 5 mm in diameter. No humpback deformity or rotation of the lunate is seen on plain radiographs. In type V injuries, the cystic changes are larger than 5 mm in diameter, and rotation of the lunate has occurred, resulting in a humpback deformity as seen with plain radiography or CT. The lunate has rotated to a position of dorsal intercalated segment instability (DISI).
In type V injuries, the cystic changes are larger than 5 mm in diameter, and rotation of the lunate has occurred, resulting in a humpback deformity as seen with plain radiography or CT. The lunate has rotated to a position of dorsal intercalated segment instability (DISI). In type VI injuries, secondary degenerative changes are present, with spurring along the radial border of the scaphoid and peaking of the radial styloid (i.e., scaphoid nonunion advanced collapse [SNAC]).
In type VI injuries, secondary degenerative changes are present, with spurring along the radial border of the scaphoid and peaking of the radial styloid (i.e., scaphoid nonunion advanced collapse [SNAC]).TABLE 27-1 Slade-Geissler Classification of Scaphoid Nonunions
| Type | Description |
|---|---|
| I | Delayed presentation at 4-12 wk |
| II | Fibrous union, minimal fracture line |
| III | Minimal sclerosis < 1 mm |
| IV | Cystic formation, 1-5 mm |
| V | Humpback deformity with > 5-mm cystic change |
| VI | Wrist arthrosis |
Arthroscopic Techniques
Various arthroscopically assisted and percutaneous techniques for fractures of the scaphoid have been described in the literature.21–32 Haddad and Goddard24 popularized the volar approach, and the dorsal approach was popularized by Slade and colleagues.26 Geissler and Slade described a technique in which the starting point of the guidewire and the eventual screw insertion are determined arthroscopically, which limits guesswork concerning the insertion point.32
Volar Percutaneous Approach
In the volar percutaneous technique that was popularized by Haddad and Goddard, the patient is placed supine with the thumb suspended in a Chinese finger trap.24 Placing the thumb under suspension allows ulnar deviation of the wrist, which improves access to the distal pole of the scaphoid. Under fluoroscopic guidance, a longitudinal, 0.5-cm skin incision is made over the most distal radial aspect of the scaphoid. Blunt dissection is used to expose the distal pole of the scaphoid. The cutaneous nerves must be protected when using this technique.
A percutaneous guidewire is introduced into the scaphoid trapezial joint and advanced proximally and dorsally across the fracture site. The position of the guidewire is easily checked in the anteroposterior, oblique, and lateral planes by rotating the forearm under fluoroscopy. This provides an almost 360-degree view of the position of the guidewire within the scaphoid. The length of the guidewire within the scaphoid is determined by placing a second guidewire next to the initial one and measuring the difference between the two. A drill is inserted through the soft tissue protector, and the scaphoid is reamed. A headless cannulated screw is then placed over the guidewire. A second guidewire may be useful to prevent rotation of the fracture fragments while the screw is being inserted.
Haddad and Goddard reported their initial results in a pilot study of 15 patients with acute fractures of the scaphoid.24 Union was achieved in all patients within an average of 57 days (range, 38 to 71 days). With this percutaneous technique, the range of motion after union was equal to that of the contralateral limb, and grip strength averaged 90% at 3 months. The patients were able to return to sedentary work within 4 days and to manual work within 5 weeks.
Dorsal Percutaneous Approach
Slade and coworkers popularized the dorsal percutaneous approach.26,27 This technique has become popular because it involves limited surgical dissection and allows arthroscopic evaluation and reduction of the scaphoid fracture. The patient is placed in the supine position on the table with the arm extended. Several towels are placed under the elbow to support the forearm parallel to the floor. The wrist is then flexed and pronated under fluoroscopy until the distal and proximal poles of the scaphoid are aligned to form a perfect cylinder. Continuous fluoroscopy is recommended as the wrist is flexed to obtain a true ring sign as the proximal and distal poles are aligned.
Geissler Technique for Arthroscopic Reduction
The advantage of using my arthroscopic technique for reduction of acute scaphoid fractures and certain scaphoid nonunions33 is that the starting point for the guidewire is viewed directly through the arthroscope, and there is no guesswork concerning the insertion point and the location of the headless cannulated screw. I think this is a simpler approach than the dorsal percutaneous approach with the ring sign. The wrist is not hyperflexed, which could distract the scaphoid fracture and cause a humpback deformity.
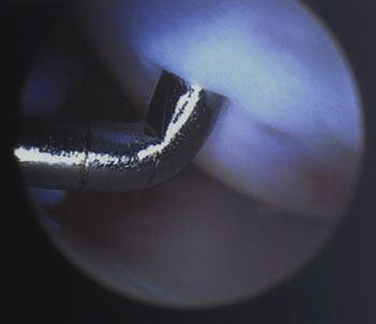
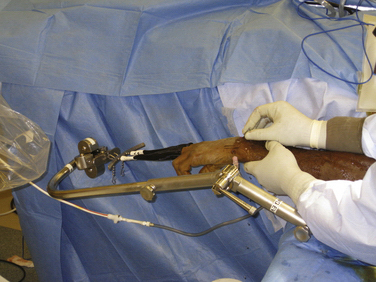
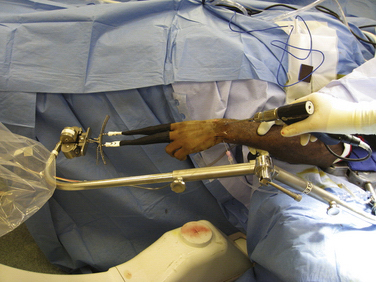
Using the Geissler technique, the wrist is initially suspended in a wrist traction tower (Acumed, Hillsboro, OR) (Fig. 27-1). The arthroscope is initially placed in the 3-4 portal to evaluate any associated soft tissue injuries that may occur with a scaphoid fracture. After evaluation and treatment of the soft tissue injuries, the arthroscope is transferred into the 6-R portal. The wrist is flexed approximately 30 degrees in the traction tower. A 14-gauge needle is inserted through the 3-4 portal, and the junction of the scapholunate interosseous ligament as it inserts onto the proximal pole of the scaphoid is palpated. The junction of the scapholunate interosseous ligament onto the scaphoid along the middle third is the ideal starting point for the screw (Fig. 27-2). A 14-gauge needle is advanced and impaled into the proximal pole of the scaphoid at the insertion of the scapholunate interosseous ligament (Figs. 27-3 and 27-4). Occasionally, some dorsal synovitis blocks visualization of the starting point and may need to be débrided.
The traction tower is then flexed, and the starting point of the needle is evaluated under fluoroscopy (Figs. 27-5 and 27-6). With this technique, the starting point is consistently determined to be at the most proximal pole of the scaphoid. The needle is simply aimed toward the thumb under fluoroscopy, and a guidewire is advanced through the needle down the central axis of the scaphoid to abut the distal pole. The position of the guidewire is checked in the posteroanterior, oblique, and lateral planes under fluoroscopy by rotating the forearm in the traction tower (Figs. 27-7 and 27-8). The fluoroscopic image is not hindered by the support beam of the tower, which is off to the side rather than in the central axis. A second guidewire is advanced against the proximal pole of the scaphoid, and the length of the screw is determined by the difference of the two guidewires. A screw at least 4 mm shorter than this measurement is recommended.
The reduction of the scaphoid is evaluated with the arthroscope in the radial and ulnar midcarpal portals. If reduction is unsatisfactory, the guidewire is advanced volarly across the wrist but still within the distal pole of the scaphoid. An additional Kirschner wire may be placed in the proximal pole of the scaphoid. These wires may be used as joysticks to further reduce the fracture anatomically under direct view with the arthroscope in the midcarpal portal. It helps to manipulate the wrist in the traction tower, usually with the wrist in extension, which further reduces the fracture. After the fracture is judged to be satisfactory, the guidewire is advanced proximally into the proximal pole of the scaphoid. The scaphoid is then reamed with the cannulated drill (Fig. 27-9).
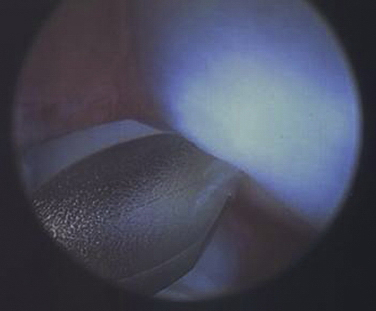
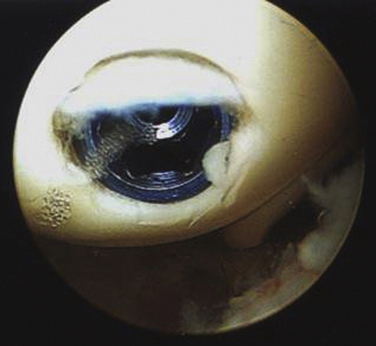
In cases of acute fractures or stable fibrous nonunions, demineralized bone matrix (DBM) is not used, and a headless cannulated screw is inserted over the guidewire (Fig. 27-10). The position of the screw is checked in the posteroanterior, oblique, and lateral planes under fluoroscopy with the wrist stabilized by the traction tower (Figs. 27-11 and 27-12). The wrist is again evaluated from the radiocarpal and midcarpal spaces. It is important to check from the radiocarpal space that the headless screw is inserted into the scaphoid and is not protruding, which may injure the articular cartilage of the scaphoid facet and the distal radius. The final reduction of the scaphoid fracture may be viewed with the arthroscope in the midcarpal space (Figs. 27-13 and 27-14).
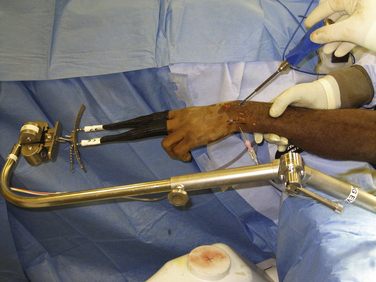
FIGURE 27-10 The headless cannulated screw is inserted over the guidewire and down the central axis of the scaphoid.

FIGURE 27-11 On the posteroanterior view, fluoroscopy shows ideal placement of the screw and reduction of the scaphoid.

FIGURE 27-12 On the oblique view, fluoroscopy shows ideal placement of the headless cannulated screw.
Scaphoid Nonunions
Geissler and Slade described their use of Slade’s dorsal percutaneous fixation technique in 15 patients with stable fibrous nonunion of the scaphoid.32 Their series included 12 horizontal oblique fractures, 1 transverse fracture, and 2 proximal pole fractures. The average time between presentation and surgery was 8 months. All patients underwent percutaneous dorsal fixation with a headless cannulated screw and no accessory bone grafting procedure, and all fractures healed in an average time of 3 months. Eight of the 15 patients underwent CT evaluation to further document healing. The patients had excellent range of motion at their final follow-up visit because of minimal surgical dissection. Twelve of the 15 patients had excellent results according to the modified Mayo wrist scale. Dorsal percutaneous fixation without bone grafting is recommended for patients with a stable fibrous nonunion who have no signs of humpback deformity and do not have extensive sclerosis of the fracture site. The scaphoid nonunion classification scheme proposed by Slade and Geissler was used to include patients with type I through III scaphoid nonunions in the study, with a 100% success rate.
For patients who have cystic scaphoid nonunions without a humpback deformity, percutaneous cancellous bone grafting or injection of DMB may be used. Applying Geissler’s technique, the scaphoid is reamed through a soft tissue protector.33 A bone biopsy needle is filled with DBM putty. The needle is placed over the guidewire from dorsal to proximal and inserted through the drill hole directly into the nonunion site. The guidewire is then retracted distally out of the proximal pole of the scaphoid while still remaining in the distal pole of the scaphoid. DBM is injected through the bone biopsy needle directly into the central hole of the scaphoid at the nonunion site. The guidewire is advanced back through the bone biopsy needle from volar to dorsal. In this manner, the guidewire passes back through the original reamed hole of the proximal pole of the scaphoid and out dorsally, protruding from the skin. The needle is then removed, and a headless cannulated screw is inserted over the guidewire across the scaphoid nonunion. The radiocarpal and midcarpal spaces are re-evaluated arthroscopically to confirm reduction and placement of the screw.
I described a technique of arthroscopic reduction of cystic scaphoid nonunions without humpback deformity using DBM putty.33 In this technique, 1 mL of DBM (Accell, Irving, CA) is injected percutaneously into the nonunion site of the scaphoid. According to the Slade and Geissler classification, the series was composed of type IV cystic scaphoid nonunions. In 14 of the 15 patients, the scaphoid nonunion healed after use of this technique. Arthroscopic evaluation of the wrist from the radiocarpal and midcarpal spaces showed no extravasation of the DBM into the joint.
PEARLS& PITFALLS
CONCLUSIONS
Fractures of the scaphoid are a common athletic injury, especially in young men.34,35 Although most nondisplaced fractures of the scaphoid heal with cast immobilization, nonunion rates of 10% to 15% have been reported. Union rates of 100% for acute fractures of the scaphoid managed by percutaneous arthroscopically assisted fixation have been consistently reported in the literature.
Arthroscopically assisted fixation has been beneficial in treating type I through type IV scaphoid nonunions by the classification scheme of Slade and Geissler.36 In patients with a stable fibrous nonunion, stabilization with a screw alone has been effective. In patients with cystic changes, arthroscopic stabilization and percutaneous injection of DBM into the nonunion site has been successful.33 Percutaneous bone grafting may be another option.
Compared with previously described percutaneous fluoroscopic techniques, arthroscopic fixation limits the guesswork concerning the exact location of the starting point of the screw. The guidewire starting point is at the most proximal pole of the scaphoid, at the junction of the scapholunate interosseous ligament. It is reproducible, as confirmed under fluoroscopy. The wrist is not hyperflexed, because such movement may flex the fracture fragment into a humpback deformity. Dorsal insertion of the screw enables central placement down the axis of the scaphoid. Early arthroscopic evaluation allows detection and management of associated soft tissue injuries (Figs. 27-15 to 27-18).

FIGURE 27-15 The posteroanterior radiograph of a 42-year-old man shows a combined distal radius and scaphoid fracture.
Neither arthroscopic nor percutaneous techniques are indicated for patients who have a severe humpback deformity, which is not correctable, or for those with advanced arthrosis of the radiocarpal joint (i.e., SNAC).37
1. Gelberman RH, Wolock BS, Siegel DB. Current concepts review: fractures and nonunions of the carpal scaphoid. J Bone Joint Surg Am. 1989;71:1560-1565.
2. Cooney WP, Dobyns JH, Linscheid RL. Fractures of the scaphoid: a rational approach to management. Clin Orthop. 1980;149:90-97.
3. Rettig AC, Ryan RO, Stone JA. Epidemiology of hand injuries in sports. In: Strickland JW, Rettig AC, editors. Hand Injuries in Athletes. Philadelphia, PA: WB Saunders; 1992:37-48.
4. Gellman H, Caputo RJ, Carter V, et al. Comparison of short and long thumb spica casts for non-displaced fractures of the carpal scaphoid. J Bone Joint Surg Am. 1989;71:354-357.
5. Kaneshiro SA, Failla JM, Tashman S. Scaphoid fracture displacement with forearm rotation in a short arm thumb spica cast. J Hand Surg. 1989;71:354-357.
6. Skirven T, Trope J. Complications of immobilization. Hand Clin. 1994;10:53-61.
7. Gelberman RH, Menon J. The vascularity of the scaphoid bone. J Hand Surg. 1980;5:508-513.
8. Rettig AC, Weidenbener EJ, Gloyeske R. Alternative management of mid-third scaphoid fractures in the athlete. Am J Sports Med. 1994;22:711-714.
9. DeMaagd RL, Engber WD. Retrograde Herbert screw fixation for treatment of proximal pole scaphoid nonunions. J Hand Surg. 1989;14:996-1003.
10. Filan SL, Herbert TJ. Herbert screw fixation of scaphoid fractures. J Bone Joint Surg Br. 1996;78:519-529.
11. Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Am. 1984;66:114-123.
12. O’Brien L, Herbert TJ. Internal fixation of acute scaphoid fractures: a new approach to treatment. Aust N Z J Surg. 1985;55:387-389.
13. Rettig ME, Raskin KB. Retrograde compression screw fixation of acute proximal pole scaphoid fractures. J Hand Surg. 1999;24:1206-1210.
14. Russe O. Fracture of the carpal navicular: diagnosis, nonoperative treatment and operative treatment. J Bone Joint Surg Am. 1960;42:759.
15. Toby EB, Butler TE, McCormack TJ, et al. A comparison of fixation screws for the scaphoid during application of cyclic bending loads. J Bone Joint Surg Am. 1997;79:1190-1197.
16. Trumble TE, Clarke T, Kreder HJ. Nonunion of the scaphoid: treatment with cannulated screws compared with treatment with Herbert screws. J Bone Joint Surg Am. 1996;78:1829-1837.
17. Garcia-Elias M, Vall A, Salo JM, et al. Carpal alignment after different surgical approaches to the scaphoid: a comparative study. J Hand Surg. 1988;13:604-612.
18. Adams BD, Blair WF, Regan DS, et al. Technical factors related to Herbert screw fixation. J Hand Surg Am. 1988;13:893-899.
19. Whipple TL. The role of arthroscopy in the treatment of intraarticular wrist fractures. Hand Clin. 1995;11:13-18.
20. Slade JF, Merrell GA, Geissler WB. Fixation of acute and selected nonunion scaphoid fractures. In: Geissler WB, editor. Wrist Arthroscopy. New York, NY: Springer; 2005:112-124.
21. Geissler WB. Arthroscopic assisted fixation of fractures of the scaphoid. Atlas Hand Clin. 2003;8:37-56.
22. Geissler WB, Hammit MD. Arthroscopic aided fixation of scaphoid fractures. Hand Clin. 2001;17:575-588.
23. Cosio MQ, Camp RA. Percutaneous pinning of symptomatic scaphoid nonunions. J Hand Surg. 1986;11:350-355.
24. Haddad FS, Goddard NJ. Acute percutaneous scaphoid fixation: a pilot study. J Bone Joint Surg Br. 1998;80:95-99.
25. Shin A, Bond A, McBride M, et al. Acute screw fixation versus cast immobilization for stable scaphoid fractures: a prospective randomized study, Paper presented at the annual meeting of the American Society Surgery for the Hand, October 5-7, 2000, Seattle, WA, 2000.
26. Slade JFIII, Grauer JN, Mahoney JD. Arthroscopic reduction and percutaneous fixation of scaphoid fractures with a novel dorsal technique. Orthop Clin North Am. 2000;30:247-261.
27. Slade JFIII, Jaskwhich J. Percutaneous fixation of scaphoid fractures. Hand Clin. 2001;17:553-574.
28. Taras JS, Sweet S, Shum W, et al. Percutaneous and arthroscopic screw fixation of scaphoid fractures in the athlete. Hand Clin. 1999;15:467-473.
29. Slade JFIII, Grauer JN. Dorsal percutaneous repair of scaphoid fractures with arthroscopic guidance. Atlas Hand Clin. 2001;6:307-323.
30. Wozasek GE, Moser KD. Percutaneous screw fixation of fractures of the scaphoid. J Bone Joint Surg Br. 1991;73:138-142.
31. Kamineni S, Lavy CBD. Percutaneous fixation of scaphoid fractures: an anatomic study. J Hand Surg. 1999;24:85-88.
32. Geissler WB, Slade JF. Arthroscopic fixation of scaphoid nonunions without bone grafting, Paper presented at the 33rd Annual Meeting of the American Society Surgery of the Hand, September 2002, Phoenix, AZ, 2002.
33. Geissler WB. Arthroscopic fixation of cystic scaphoid nonunions with DBM, Paper presented at the annual meeting of the American Association Hand Surgery, January 2006, Tucson, AZ, 2006.
34. Geissler WB. Carpal fractures in athletes. Clin Sports Med. 2001;20:167-188.
35. Rettig AC, Kollias SC. Internal fixation of acute stable scaphoid fractures in the athlete. Am J Sports Med. 1996;24:182-186.
36. Geissler WB. Wrist Arthroscopy. New York, NY: Springer; 2005.
37. Fernandez DL. Anterior bone grafting and conventional lag screw fixation to treat scaphoid nonunions. J Hand Surg Am. 1990;15:140-147.