Chapter 60 Acute Dislocations
Indications for Open Reduction
Open reduction of an acute dislocation usually is indicated in the following circumstances:
1. If anatomical, concentric reduction cannot be achieved by gentle, closed techniques with the patient under general anesthesia. Interposed soft tissues or osteochondral fragments may contribute to the irreducibility.
2. If a stable reduction cannot be maintained. Articular fractures often are unstable and must be reduced and fixed to ensure stability of the reduction.
3. If careful evaluation before closed reduction reveals normal neurological function and, after reduction, a definite, complete motor and sensory nerve deficit becomes evident.
4. If circulatory impairment distal to the injury is well documented before reduction and persists after reduction. Further assessment of the circulation is essential and should include arteriography.
5. If ischemia is persistent. Surgical exploration with appropriate management of the vascular injury is indicated.
Ankle
Dislocations of the ankle without fracture of either the medial or lateral malleolus or the anterior or posterior lip of the distal articular surface of the tibia are extremely rare. Usually, any dislocations that do occur are easily reduced by closed methods. Posterior dislocation of the fibula behind the tibia may contribute to difficulty with closed reduction and at times may require open reduction. Ruptures of the deltoid ligament, the anterior tibiotalar ligament, and the anterior and posterior talofibular ligaments occur alone or in combination. Controversy exists over acute ligamentous repair without evidence of fracture. Good-to-excellent results are possible without acute ligamentous repair; however, syndesmosis and mortise widening should be treated operatively if present. (For discussion of acute fractures of the ankle, see Chapter 54; of malunited fractures of the ankle, see Chapter 58; and of ruptures of the ligaments of the ankle, see Chapter 89.)
Patella
Acute Dislocations of the Patella
Acute dislocations of the patella usually are managed by closed methods (Fig. 60-1). The patella is almost always dislocated laterally, and extension of the flexed knee with pressure applied to the lateral margin of the patella results in reduction. The limb is immobilized in a knee immobilizer for 3 to 6 weeks and then motion is begun to prevent arthrofibrosis and to promote the formation of strong collagen along the lines of stress. Radiographs should be evaluated carefully to ensure that no osteochondral fragments are displaced within the joint. If a hemarthrosis is present, MRI is warranted to check for osteochondral fragments. One study demonstrated articular cartilage injury in 94% of patients; 72% had an osteochondral or chondral fracture, and 23% had patellar microfractures.
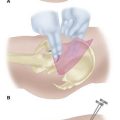
Arthroscopic techniques for the repair of the medial patellar retinaculum after acute patellar dislocations have been described, but we prefer the open method at our institution if repair is indicated (Fig. 60-2).
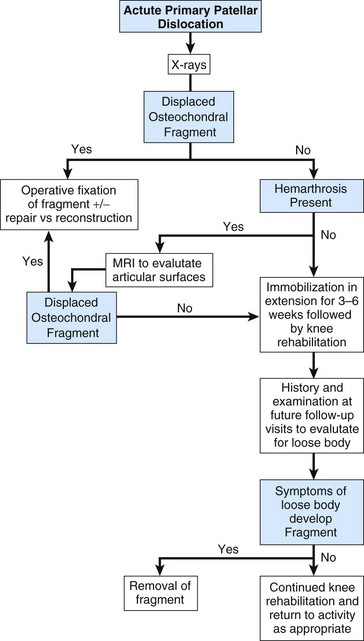
FIGURE 60-2 Algorithm for guiding the evaluation and management of acute primary patellar dislocation.
(Modified from Mehta VM, Inoue M, Nomura E, Fithian DC: An algorithm guiding the evaluation and treatment of acute primary patellar dislocation, Sports Med Arthrosc Rev 15:78, 2007.)
Open Reduction and Repair of Patellar Dislocation
 Through a medial parapatellar incision, explore the tear in the medial patellar retinaculum.
Through a medial parapatellar incision, explore the tear in the medial patellar retinaculum.
 Irrigate and explore the knee joint. Remove or fix any loose osteochondral fragments, and make a thorough search for any further loose fragments or intraarticular damage to the joint.
Irrigate and explore the knee joint. Remove or fix any loose osteochondral fragments, and make a thorough search for any further loose fragments or intraarticular damage to the joint.
 Repair any disruption in the vastus medialis muscle belly or in the medial patellar retinaculum.
Repair any disruption in the vastus medialis muscle belly or in the medial patellar retinaculum.
 Pay careful attention to that portion of the vastus medialis that originates in the region of the femoral adductor tubercle. If this origin has been disrupted and has retracted proximally, the angle of insertion of the vastus medialis muscle fibers into the patella is significantly changed. These fibers are vital to the prevention of recurrent lateral dislocation of the patella.
Pay careful attention to that portion of the vastus medialis that originates in the region of the femoral adductor tubercle. If this origin has been disrupted and has retracted proximally, the angle of insertion of the vastus medialis muscle fibers into the patella is significantly changed. These fibers are vital to the prevention of recurrent lateral dislocation of the patella.
Grafting of the Medial Patellar Retinaculum
 Prepare a semitendinosus autologous graft or allograft.
Prepare a semitendinosus autologous graft or allograft.
 Center the skin incision between the medial edge of the patella and adductor tubercle.
Center the skin incision between the medial edge of the patella and adductor tubercle.
 Identify the extensor retinaculum.
Identify the extensor retinaculum.
 Make a small incision at the medial edge of the patella and just distal to the adductor tubercle.
Make a small incision at the medial edge of the patella and just distal to the adductor tubercle.
 Using a hemostat, pass the graft through a tunnel between the capsule and retinaculum.
Using a hemostat, pass the graft through a tunnel between the capsule and retinaculum.
 Secure the graft to the femur using suture, interference screw, or a suture anchor.
Secure the graft to the femur using suture, interference screw, or a suture anchor.
 After cycling the knee to ensure correct isometry, attach the graft to the patella with an interference screw or suture anchor.
After cycling the knee to ensure correct isometry, attach the graft to the patella with an interference screw or suture anchor.
 Repair the retinaculum with figure-of-eight sutures.
Repair the retinaculum with figure-of-eight sutures.
 Close the wound in layers and apply a controlled-motion knee brace.
Close the wound in layers and apply a controlled-motion knee brace.
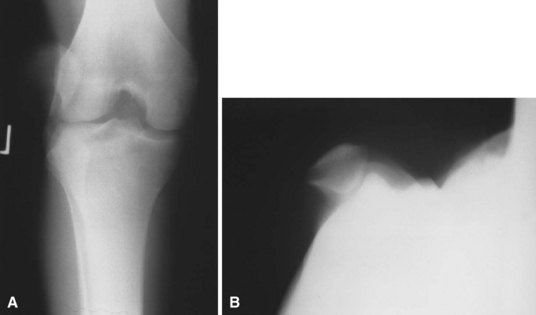
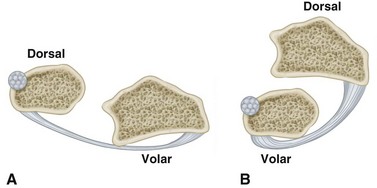
Intraarticular Dislocations of the Patella
Intraarticular dislocations of the patella are rare and are of two types. The most common type is a horizontal intraarticular dislocation of the patella with detachment of the quadriceps tendon; the articular surface of the patella is directed toward the tibial articular surface (Fig. 60-3). In the other type, the patella also is dislocated horizontally but its inferior pole is detached from the patellar tendon and the articular surface faces proximally. These dislocations frequently are difficult to reduce by closed methods, and open reduction generally is required, along with repair of the extensor mechanism.
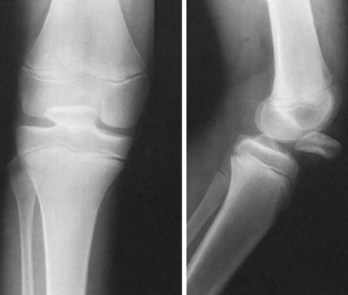
FIGURE 60-3 Intraarticular horizontal dislocation of patella. Quadriceps mechanism usually remains intact.
(From Brady TA, Russell D: Interarticular horizontal dislocation of the patella: a case report, J Bone Joint Surg 47A:1393, 1965.)
Open Reduction and Repair of the Extensor Mechanism
 Through a medial parapatellar incision, expose the dislocated patella, usually found in the intercondylar notch.
Through a medial parapatellar incision, expose the dislocated patella, usually found in the intercondylar notch.
 Replace the patella into its bed in the quadriceps or patellar tendon, and reattach it there with sutures. Placing the sutures through holes drilled in the patella may help secure the repair.
Replace the patella into its bed in the quadriceps or patellar tendon, and reattach it there with sutures. Placing the sutures through holes drilled in the patella may help secure the repair.
 Inspect the knee, and remove any loose osteochondral or cartilaginous fragments.
Inspect the knee, and remove any loose osteochondral or cartilaginous fragments.
Knee
Dislocation of the knee has been considered a rare injury, but it seems to have increased in frequency over the years. It has been noted that the incidence might be higher than recognized because many knee dislocations are reduced at the scene of the injury without subsequent accurate reporting of this diagnosis (Fig. 60-4).
Knee dislocations usually can be reduced satisfactorily by closed methods. After reduction and in the absence of additional complications, aspiration of the hemarthrosis using sterile technique and immobilizing the knee in full extension are satisfactory temporary treatments. The neurocirculatory status should be checked frequently for 5 to 7 days. A large transarticular pin can be placed through the intercondylar notch of the femur into the intercondylar eminence of the tibia to provide immediate stability for knees that redislocate in a splint or after vascular repair (Fig. 60-5). Transarticular pins have been associated with pin track infection and breakage and should be used with caution. We have found a transarticular pin to be useful when the posterior capsule is completely disrupted, preventing concentric reduction in full extension. The pin is left in place for 4 to 6 weeks, and range of motion is begun. A knee-spanning external fixator can be used in open-knee dislocations with extensive soft tissue injury or in unstable knees after vascular repair. When it is certain that the circulation is not impaired, treatment can be selected for repair of the injured ligaments, as discussed in Chapter 45. Closed reduction may be impossible, however, especially when the dislocation is posterolateral. Blocking of reduction by the interposition of the joint capsule and “buttonholing” of the femoral condyle medially through a tear in the capsule have been reported. A torn tibial collateral ligament or pes anserinus tendon also can block reduction. When an irreducible dislocation is encountered, open reduction through a medial approach often is necessary; however, the approach usually depends on the type of dislocation. The entrapping and torn structures are released and repaired, and the postoperative care is the same as for ligamentous injuries (see Chapter 45).
Several surgeons have advocated early repair of all injured structures in order to obtain satisfactory outcomes. Only fair or poor results can be expected with nonoperative treatment. When open treatment is selected, the surgeon must be prepared to repair structures medially, laterally, anteriorly, and posteriorly as indicated. MRI can be a valuable tool in preoperative planning. Techniques for repair and reconstruction of the ligaments are found in Chapters 45 and 51.
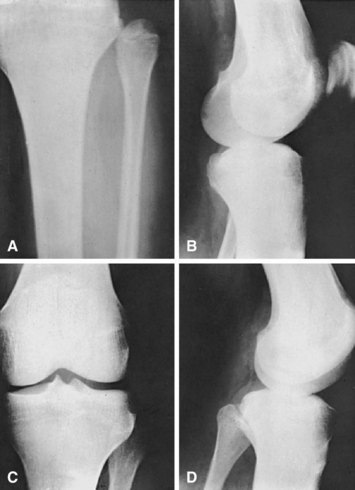
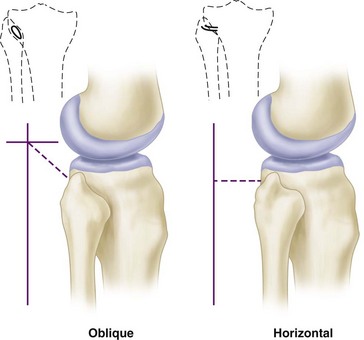
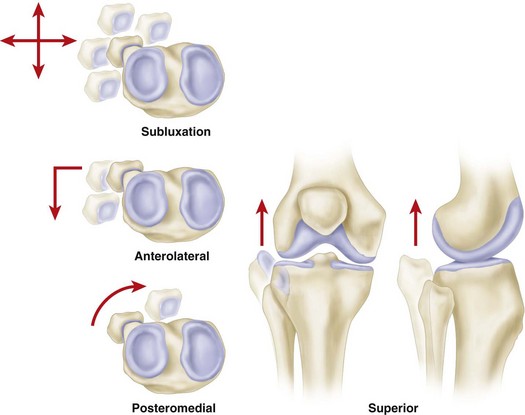
Proximal Tibiofibular Joint
Acute dislocation of the proximal tibiofibular joint is rare (Fig. 60-6). It usually is the result of a twisting trauma and may be seen in association with other injuries to the same extremity. Patients usually present with pain and a prominence in the lateral aspect of the knee. Injuries of the proximal tibiofibular joint frequently are overlooked. Patients with chronic dislocations or subluxation complain of popping and instability, which can be confused with a lateral meniscus injury. The proximal tibiofibular joint can be oblique or horizontal (Fig. 60-7). More motion is possible in horizontal joints, and the relative restriction of motion in oblique joints is presumably the reason why most injuries occur in them.
Ogden classified tibiofibular subluxations and dislocations into four types (Fig. 60-8): subluxation and anterolateral, posteromedial, and superior dislocations. Keogh et al. concluded after a cadaver study that the diagnosis of suspected dislocations of the proximal tibiofibular joint was best determined with an axial CT scan (Fig. 60-9).
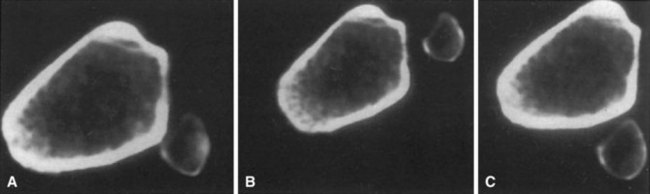
FIGURE 60-9 Axial CT scan of cadaver knee. A, Anatomical. B, Dislocated anteriorly. C, Dislocated posteriorly.
(From Keogh P, Masterson E, Murphy B, et al: The role of radiography and computed tomography in the diagnosis of acute dislocation of the proximal tibiofibular joint, Br J Radiol 66:108, 1993.)
Anterolateral dislocations (see Fig. 60-6) were the most common proximal tibiofibular dislocations in Ogden’s series. They usually were treated successfully by closed methods.
Hip
Hip dislocations are classified according to the position of the femoral head in relation to the acetabulum and according to associated fractures of the acetabulum and proximal femur. Posterior dislocations have been classified by Thompson and Epstein into five types: type I, with or without a minor fracture; type II, with a large single fracture of the posterior acetabular rim; type III, with a comminuted fracture of the rim of the acetabulum, with or without a major fragment; type IV, with fracture of the acetabular rim and floor; and type V, with fracture of the femoral head. Types II through IV with significant associated acetabular fractures are discussed in Chapter 56, and femoral head fractures are discussed in Chapter 55
Anterior dislocations also have been classified by Epstein as follows:
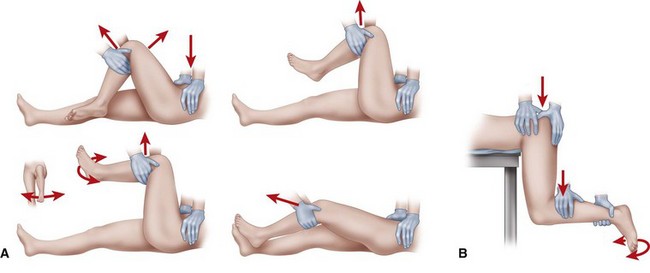
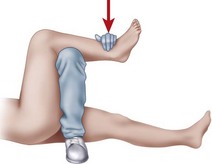
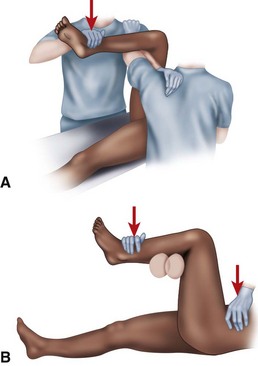
The following guidelines for treatment refer to hip dislocations without significant associated femoral head or acetabular fractures (Thompson and Epstein type I). Several methods of closed reduction have been used successfully, all of which generally consist of re-creating the injurious deforming force (for posterior dislocations—flexion, adduction, and internal rotation; for anterior dislocations—abduction and external rotation in extension). Traction in line with the affected femur and small amounts of rotation and abduction and adduction complete the reduction. The Allis maneuver is performed for posterior dislocations as previously described with the patient supine, whereas the Stimson maneuver is similarly performed with the patient prone (Fig. 60-11). Other reduction techniques involve levering the affected limb at the ankle over a fulcrum (Figs. 60-12 and 60-13). Regardless of the method chosen, only two or three attempts should be made at closed reduction. Multiple, increasingly forcible attempts at reduction could lead to an iatrogenic femoral head, neck, or shaft fracture or cartilaginous injury to the femoral head or acetabulum.
Open Reduction of Hip Dislocation
 Regardless of the direction of the dislocation, when the approach has been made, assess the capsule first.
Regardless of the direction of the dislocation, when the approach has been made, assess the capsule first.
 If the femoral head is buttonholed, extend the traumatic capsulotomy in a T-shaped fashion along the acetabular rim, carefully preserving the labrum, if possible.
If the femoral head is buttonholed, extend the traumatic capsulotomy in a T-shaped fashion along the acetabular rim, carefully preserving the labrum, if possible.
 Inspect the joint for intervening capsule, labrum, piriformis muscle, or bony fragments.
Inspect the joint for intervening capsule, labrum, piriformis muscle, or bony fragments.
 If necessary, retract or distract the hip manually or with skeletal traction applied through a fracture table or femoral distractor for better assessment of the joint.
If necessary, retract or distract the hip manually or with skeletal traction applied through a fracture table or femoral distractor for better assessment of the joint.
 When the joint has been cleared of debris, reduce the hip joint by releasing the traction.
When the joint has been cleared of debris, reduce the hip joint by releasing the traction.
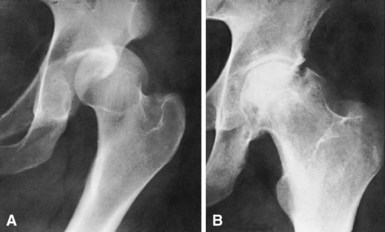
Complications
Osteonecrosis has been reported to occur in 4% to 22% of hip dislocations without associated femoral head or acetabular fracture (Fig. 60-14). Time to reduction plays a role in the development of this complication because multiple studies have shown a direct correlation between the time to reduction and the prevalence of osteonecrosis. In the best of circumstances, a percentage of patients develop avascular changes despite prompt reduction of a dislocated hip. Patients with posterior dislocations and multiple injuries are apparently at increased risk for the development of osteonecrosis. Most patients who develop osteonecrosis have symptoms within 2 years of injury, although late cases of osteonecrosis with radiographic changes delayed 5 years have been reported.
Pubic Symphysis and Sacroiliac Joints
Dislocations involving the symphysis pubis and sacroiliac joints occur only with high-energy trauma. Considerable force is required to overcome the complex ligamentous structures that provide stability to the adult pelvis. The relevant anatomy and appropriate diagnostic and treatment algorithms are included in Chapter 56.
Sternoclavicular Joint
For acute anterior sternoclavicular dislocations, Heinig recommended closed reduction after infiltrating the hematoma with a local anesthetic. In this situation, a meticulous sterile technique must be used. With the patient supine and with a large sandbag between the scapulae, traction is applied to the affected extremity, and the arm is abducted and extended while pressure is applied downward over the dislocated end of the clavicle. When the dislocation is reduced, the joint may be unstable, and the decision must be made whether to accept a residual subluxation or perform an open reduction and an internal fixation. In anterior dislocations, the deformity generally is accepted. If later instability is painful, ligament reconstruction (see Chapter 47) or resection of the medial end of the clavicle (see Chapter 61) may be indicated.
If open reduction is necessary, an attempt should be made to obtain stable fixation without the use of transarticular pins. Several deaths have been reported that resulted from the migration of Steinmann pins or Kirschner wires into the heart, pulmonary artery, innominate artery, or aorta. Occasionally, a whole pin migrates, or the pin breaks, and parts of it may migrate. Reports suggest that the incidence of significant complications may approach 25% after sternoclavicular procedures. Waters et al. advocated suture stabilization of costoclavicular and sternoclavicular ligaments for unstable reductions. Such considerations imply that surgical treatment should be reserved for irreducible posterior sternoclavicular dislocations and for significantly symptomatic, old, unreduced, or recurrent anterior sternoclavicular dislocations. If open reduction is required, the approach as described for old, unreduced (see Chapter 47) and recurrent (see Chapter 61) sternoclavicular dislocations can be modified.
Acromioclavicular Joint
Etiology and Classification
Injuries to the acromioclavicular joint usually are the result of a force applied downward on the acromion. The most common mechanism of injury is a fall directly onto the dome of the shoulder. The clavicle rests against the first rib, and the rib blocks further downward displacement of the clavicle. As a result, if the clavicle is not fractured, the acromioclavicular and coracoclavicular ligaments are ruptured. Injuries to the other structures in this area may include tears in the clavicular attachments of the deltoid and trapezius muscles (Fig. 60-15); fractures of the acromion, clavicle, and coracoid; disruption of the acromioclavicular fibrocartilage; and fractures of the articular cartilage of the acromioclavicular joint.
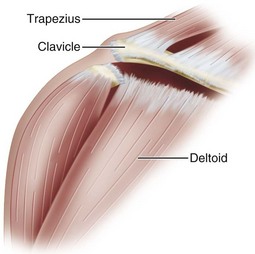
FIGURE 60-15 Dislocation of clavicle often causes tears in clavicular attachments of deltoid and trapezius muscles.
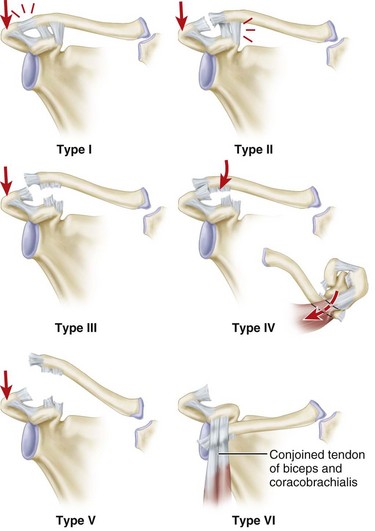
Although many surgeons still use three grades of severity of separation, Rockwood and others subclassify these injuries further into types I through VI (Fig. 60-16). Type I injuries result from minor strains of the acromioclavicular ligament and joint capsule. The acromioclavicular joint is stable, and pain is minimal. Although radiographs initially may be negative, periosteal calcification at the distal end of the clavicle may be apparent later. More significant forces cause type II, and the acromioclavicular ligament and the joint capsule are ruptured. The coracoclavicular ligaments remain intact. In this instance, the acromioclavicular joint is unstable. This instability, especially in the anteroposterior plane, causes deformity, and on radiographs the lateral end of the clavicle may ride higher than the acromion, usually by less than the thickness of the clavicle even when stress is applied to the joint. Considerable pain and tenderness are present over the acromioclavicular joint, but stress radiographs are necessary to assess the degree of instability after these injuries. Injuries that result from a force sufficient to rupture the acromioclavicular and coracoclavicular ligaments have been considered grade III injuries.
Clinical Findings
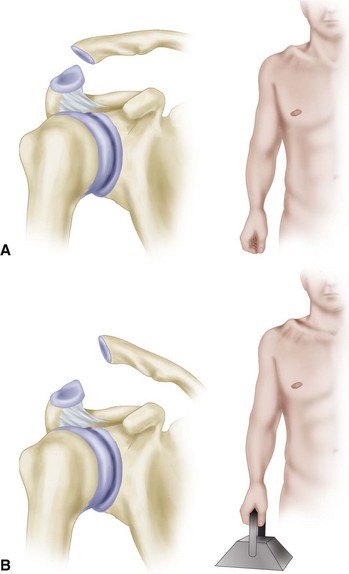
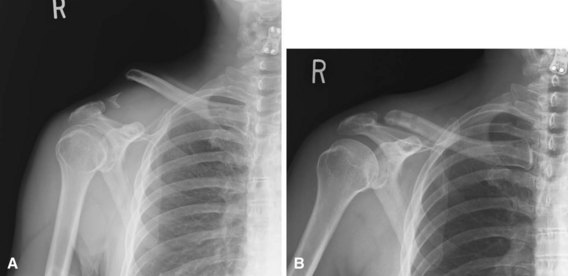
In addition to the physical findings of pain, swelling, and an unstable acromioclavicular joint with a mobile distal clavicle, radiographs are helpful in assessing the degree of injury. If the acromioclavicular ligament has been torn, and the coracoclavicular ligaments are intact, anteroposterior instability is the usual finding. Widening of the acromioclavicular joint is noted in the anteroposterior projection in these grade II injuries. Further instability in the acromioclavicular joint is detected by suspending 10 to 15 lb (4.5 to 6.8 kg) of weights to both of the patient’s wrists. If possible, the weights should be tied to the wrists to avoid having the patient hold them; this allows the upper extremity muscles to relax completely. With the patient standing erect, anteroposterior radiographs are made of each acromioclavicular joint, and the two sides are compared. In significant subluxations, the lateral end of the clavicle is displaced superiorly, or the scapula and arm are displaced inferiorly, more than one half the thickness of the clavicle. In dislocations, the distal clavicle is displaced a distance that is equal to or more than its thickness (Fig. 60-17).
Treatment
Resection of the lateral or distal end of the clavicle has been proposed for the treatment of acute and old acromioclavicular dislocations. If the coracoclavicular ligaments are disrupted, they must be repaired or reconstructed; internal fixation is required, either across the acromioclavicular defect or between the coracoid and the clavicle. Dewar and Barrington described transfer of the coracoid to the clavicle to hold the lateral end of the bone in position. This technique can be combined with resection of the lateral end of the clavicle (see Chapter 47).
Most of the procedures that reduce and fix the acromioclavicular joint should be reserved for patients younger than 45 years old. DePalma’s anatomical dissections and studies suggest that early degenerative changes are developing in the acromioclavicular joint by the third decade, and that significant changes are present by the fourth decade. Although procedures in which the distal clavicle is excised can be used satisfactorily in young patients, older patients with painful, disabling, old acromioclavicular dislocations with degenerative changes should especially be considered as candidates for such a procedure. Various arthroscopic techniques also have been described for acromioclavicular joint fixation, showing fair-to-good results at short-term follow-up. We have limited experience with the arthroscopic treatment of acromioclavicular joint injuries and prefer an open procedure. The treatment of old acromioclavicular dislocations is discussed in Chapter 61.
Anatomic Reconstruction of the Conoid and Trapezoid Ligaments
 Make a curvilinear incision 3.5 cm from the distal clavicle in the lines of Langer to the tip of the coracoid (Fig. 60-18A).
Make a curvilinear incision 3.5 cm from the distal clavicle in the lines of Langer to the tip of the coracoid (Fig. 60-18A).
 Raise full-thickness flaps anteriorly and posteriorly on the clavicle, skeletonizing the clavicle.
Raise full-thickness flaps anteriorly and posteriorly on the clavicle, skeletonizing the clavicle.
 Resect the last 10 mm of the distal clavicle, beveling the inferior bone.
Resect the last 10 mm of the distal clavicle, beveling the inferior bone.
 Dissect the coracoid posterior to the deltoid. Once the coracoid is exposed, create a tunnel under the coracoid with a right-angle clamp to ensure easy graft passage.
Dissect the coracoid posterior to the deltoid. Once the coracoid is exposed, create a tunnel under the coracoid with a right-angle clamp to ensure easy graft passage.
 Drill the first tunnel 45 mm from the distal clavicle (35 mm if distal clavicular resection has already been performed) using an appropriate steel reamer. It should be positioned slightly posterior to re-create normal conoid position (see Fig. 60-18A).
Drill the first tunnel 45 mm from the distal clavicle (35 mm if distal clavicular resection has already been performed) using an appropriate steel reamer. It should be positioned slightly posterior to re-create normal conoid position (see Fig. 60-18A).
 Drill the second tunnel 15 mm lateral to the first tunnel slightly anteriorly to re-create trapezoid position (see Fig. 60-18A).
Drill the second tunnel 15 mm lateral to the first tunnel slightly anteriorly to re-create trapezoid position (see Fig. 60-18A).
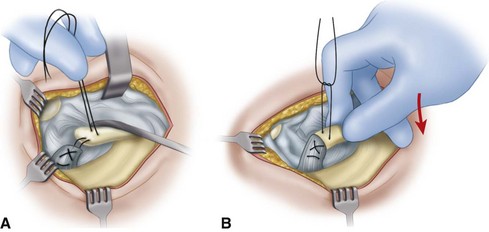
 Pass the lateral limb of the graft with suture through the first (posterior) tunnel, cross it posteriorly so that it will ultimately be a figure-of-eight. Then feed the medial limb of the graft through the anterior tunnel. Do not cross the suture, but pass it directly so that it will be a circle (Fig. 60-18B).
Pass the lateral limb of the graft with suture through the first (posterior) tunnel, cross it posteriorly so that it will ultimately be a figure-of-eight. Then feed the medial limb of the graft through the anterior tunnel. Do not cross the suture, but pass it directly so that it will be a circle (Fig. 60-18B).
 Secure the graft with a soft tissue interference screw in the posterior or anterior tunnel, bringing the suture up through the cannulated screw.
Secure the graft with a soft tissue interference screw in the posterior or anterior tunnel, bringing the suture up through the cannulated screw.
 With upper displacement of the scapulohumeral complex, slightly overreduce the acromioclavicular joint. After assessment of correct screw placement, place a second screw in the final bone tunnel.
With upper displacement of the scapulohumeral complex, slightly overreduce the acromioclavicular joint. After assessment of correct screw placement, place a second screw in the final bone tunnel.
 Confirm the reduction with C-arm Zanca view. Tie the suture (Fig. 60-19).
Confirm the reduction with C-arm Zanca view. Tie the suture (Fig. 60-19).
 Route the remaining lateral limb of the tendon graft, and suture it to the acromion as in an acromioclavicular ligament reconstruction (Fig. 60-20).
Route the remaining lateral limb of the tendon graft, and suture it to the acromion as in an acromioclavicular ligament reconstruction (Fig. 60-20).
 Close the deltotrapezial interval securely, and close the skin with absorbable monofilament suture (Fig. 60-21).
Close the deltotrapezial interval securely, and close the skin with absorbable monofilament suture (Fig. 60-21).
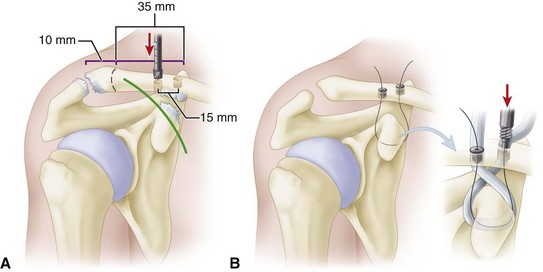
FIGURE 60-18 Mazzocca anatomic coracoclavicular reconstruction. A, Incision and tunnel placement. B, Graft passage. SEE TECHNIQUE 60-5.
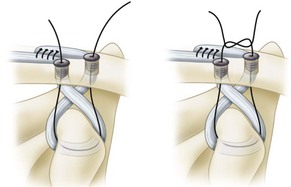
FIGURE 60-19 Mazzocca anatomic coracoclavicular reconstruction. Interference screw fixation of graft to clavicle. SEE TECHNIQUE 60-5.
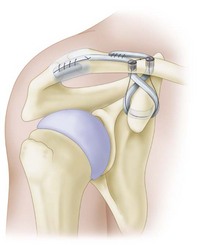
FIGURE 60-20 Mazzocca anatomic coracoclavicular reconstruction. Final placement of grafts. SEE TECHNIQUE 60-5.
Coracoclavicular Suture Fixation
 Make a curved incision to expose the acromioclavicular joint, the distal end of the clavicle, and the coracoid process.
Make a curved incision to expose the acromioclavicular joint, the distal end of the clavicle, and the coracoid process.
 Expose the acromioclavicular joint, and remove any loose fragments or other debris.
Expose the acromioclavicular joint, and remove any loose fragments or other debris.
 Place mattress sutures in the ruptured coracoclavicular ligaments, but do not tie them.
Place mattress sutures in the ruptured coracoclavicular ligaments, but do not tie them.
 Using a
Using a  -inch drill bit, make two holes in the clavicle above the coracoid in the anteroposterior plane.
-inch drill bit, make two holes in the clavicle above the coracoid in the anteroposterior plane.
 Pass a No. 5 nonabsorbable suture beneath the base of the coracoid and superiorly through the two holes in the clavicle. With the joint reduced, tie the sutures. The entire clavicle is not encircled by the sutures because motion might cause the suture to erode through the entire bone.
Pass a No. 5 nonabsorbable suture beneath the base of the coracoid and superiorly through the two holes in the clavicle. With the joint reduced, tie the sutures. The entire clavicle is not encircled by the sutures because motion might cause the suture to erode through the entire bone.
 At this point, if the surgeon is concerned about anteroposterior instability, a small Kirschner wire can be passed across the acromioclavicular joint and bent on its end. Tie the sutures already placed in the coracoclavicular ligaments.
At this point, if the surgeon is concerned about anteroposterior instability, a small Kirschner wire can be passed across the acromioclavicular joint and bent on its end. Tie the sutures already placed in the coracoclavicular ligaments.
 Repair the acromioclavicular joint capsule, and reattach the origins of the deltoid and trapezius muscles to the distal clavicle.
Repair the acromioclavicular joint capsule, and reattach the origins of the deltoid and trapezius muscles to the distal clavicle.
Distal Clavicular Excision
 Expose the acromioclavicular joint, the lateral end of the clavicle, and the coracoid through an anterior curved incision.
Expose the acromioclavicular joint, the lateral end of the clavicle, and the coracoid through an anterior curved incision.
 Incise the capsule and the superior acromioclavicular ligament in line with the clavicle to allow subperiosteal exposure of the clavicle and subsequent capsular and ligamentous repair.
Incise the capsule and the superior acromioclavicular ligament in line with the clavicle to allow subperiosteal exposure of the clavicle and subsequent capsular and ligamentous repair.
 Resect subperiosteally the lateral 1 cm of the clavicle; use a bone-cutting forceps or an oscillating saw to osteotomize the bone obliquely in an inferolateral direction (Fig. 60-22).
Resect subperiosteally the lateral 1 cm of the clavicle; use a bone-cutting forceps or an oscillating saw to osteotomize the bone obliquely in an inferolateral direction (Fig. 60-22).
 Remove the superior subcutaneous edge of the remaining end of the bone with a file.
Remove the superior subcutaneous edge of the remaining end of the bone with a file.
 Place mattress sutures in the ruptured coracoclavicular ligaments, but do not tie them.
Place mattress sutures in the ruptured coracoclavicular ligaments, but do not tie them.
 Insert two Kirschner wires the size of a guidewire about 2 cm apart through the lateral border of the acromion so that they enter the middle of the articular facet of the acromion. To accomplish this more easily, pass the wires retrograde from the acromial articular surface through the acromion and out through the skin.
Insert two Kirschner wires the size of a guidewire about 2 cm apart through the lateral border of the acromion so that they enter the middle of the articular facet of the acromion. To accomplish this more easily, pass the wires retrograde from the acromial articular surface through the acromion and out through the skin.
 While the lateral end of the clavicle is held in normal position, advance the wires into the clavicle for 2.5 to 4.0 cm. As described for the modified Phemister technique, check the position of the wires by radiographs, bend them, and cut them off beneath the skin.
While the lateral end of the clavicle is held in normal position, advance the wires into the clavicle for 2.5 to 4.0 cm. As described for the modified Phemister technique, check the position of the wires by radiographs, bend them, and cut them off beneath the skin.
 As an alternative, the method of coracoclavicular fixation described by Weaver and Dunn can be used.
As an alternative, the method of coracoclavicular fixation described by Weaver and Dunn can be used.
 Hold the clavicle in the reduced position relative to the acromion and coracoid.
Hold the clavicle in the reduced position relative to the acromion and coracoid.
 Apply traction to the coracoacromial ligament to determine the proper length of ligament necessary to maintain the reduction. Excise the excess ligament, and place a mattress suture of a No. 1 nonabsorbable material in the ligament, leaving the suture ends free.
Apply traction to the coracoacromial ligament to determine the proper length of ligament necessary to maintain the reduction. Excise the excess ligament, and place a mattress suture of a No. 1 nonabsorbable material in the ligament, leaving the suture ends free.
 Drill two small holes in the superior cortex of the clavicle, and pass a suture end through each (Fig. 60-23A).
Drill two small holes in the superior cortex of the clavicle, and pass a suture end through each (Fig. 60-23A).
 Hold the clavicle in the reduced position, and pull on the suture to bring the coracoacromial ligament into the medullary canal of the clavicle (Fig. 60-23B). Tie the suture while the reduction is maintained.
Hold the clavicle in the reduced position, and pull on the suture to bring the coracoacromial ligament into the medullary canal of the clavicle (Fig. 60-23B). Tie the suture while the reduction is maintained.
 Repair the capsule and ligament of the acromioclavicular joint, and tie the sutures previously placed in the coracoclavicular ligaments.
Repair the capsule and ligament of the acromioclavicular joint, and tie the sutures previously placed in the coracoclavicular ligaments.
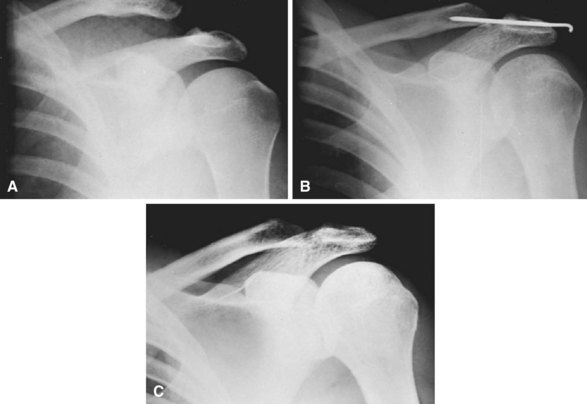
FIGURE 60-22 Stewart technique for acute dislocation of acromioclavicular joint. A, Soon after injury. B, Six weeks after surgery. C, Three months after surgery. SEE TECHNIQUE 60-7.
Shoulder
Uncomplicated dislocations of the shoulder rarely require open reduction. Some acute anterior dislocations of the shoulder are irreducible because of interposition of the long head of the biceps tendon, greater tuberosity, or fracture fragments of the glenoid. Fracture-dislocations of the shoulder are discussed in Chapter 57. Rotator cuff tears that require repair also have been reported with shoulder dislocation (see Chapter 46).
The biomechanics and pathoanatomy seen with recurrent dislocations are discussed in Chapter 47. In an effort to determine which shoulders are prone to recurrent dislocation, Baker et al. identified intraarticular lesions of the shoulder and classified these into three groups. Group 1 (6 patients) had capsular tears with no labral lesions. The shoulders were stable on examination under anesthesia, and hemorrhage was present in the inferior capsule between the middle and inferior glenohumeral ligaments. No Hill-Sachs lesions were identified. Group 2 (11 patients) had subluxable shoulders on examination under anesthesia with partial detachment of the labrum from the glenoid rim and the inferior glenohumeral ligament attachment to the biceps insertion. Hill-Sachs lesions were identified in this group. Group 3 (28 shoulders) showed gross instability on examination under anesthesia and complete disruption of the inferior glenohumeral ligament insertion anteriorly. Hill-Sachs lesions also were seen.
Recurrent instability in young patients has been reported in up to 90% of patients treated nonoperatively. Up to 12% recurrence has been reported in operatively treated shoulders. Arthroscopic stabilization has been recommended in active young patients with no history of subluxation or impingement who may otherwise have recurrent dislocations after acute traumatic dislocation. We currently favor initial nonoperative management for first-time dislocations but consider arthroscopic stabilization procedures an appropriate alternative in selected patients (see Chapter 52 for arthroscopic shoulder stabilization techniques).
Elbow
Dislocation of the Radial Head
If dislocation of the radial head occurs without dislocation of the humeroulnar joint, the radial head is almost always displaced anteriorly and can be easily reduced manually. Because the annular ligament has been ruptured or displaced, the pull of the biceps muscle often causes the dislocation to recur, and unless the radial head remains reduced, it would limit flexion of the joint. Consequently, open reduction and repair or reconstruction of the annular ligament is indicated (1) when the dislocation recurs after closed reduction and immobilization of the elbow in more than 90 degrees of flexion; (2) when it has gone untreated for 2 to 4 weeks; or (3) when it is irreducible by closed means, usually because the radial head is trapped by interposed soft tissues. When the dislocation has gone untreated for more than 4 or 5 weeks in an adult, the radial head should be excised (see Chapter 57).
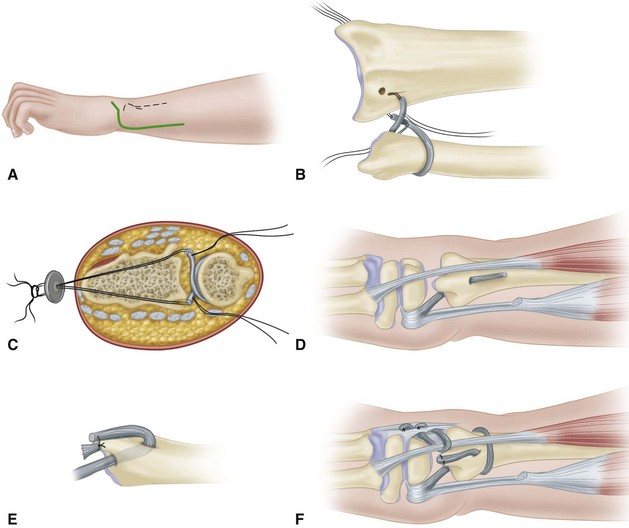
Open Reduction of Radial Head Dislocation
 Make an incision over the posterior aspect of the radial head, expose the head, and identify the annular ligament (Fig. 60-24).
Make an incision over the posterior aspect of the radial head, expose the head, and identify the annular ligament (Fig. 60-24).
 Reduce the dislocation, and, if possible, repair the ligament and disrupted capsule with fine interrupted sutures.
Reduce the dislocation, and, if possible, repair the ligament and disrupted capsule with fine interrupted sutures.
 If repair is impossible, take a fascial graft 1.3 cm wide × 10 cm long from the outer aspect of the thigh (or from the deep fascia on the dorsal aspect of the forearm, as described in Chapter 57).
If repair is impossible, take a fascial graft 1.3 cm wide × 10 cm long from the outer aspect of the thigh (or from the deep fascia on the dorsal aspect of the forearm, as described in Chapter 57).
 Expose the posterior surface of the ulna through a second incision 5.0 cm long, and drill a hole transversely through the bone 1.3 cm distal to the level of the radial head.
Expose the posterior surface of the ulna through a second incision 5.0 cm long, and drill a hole transversely through the bone 1.3 cm distal to the level of the radial head.
 Pass the strip of fascia lata through this hole and around the radial neck, and suture its ends together without tension, creating a new annular ligament.
Pass the strip of fascia lata through this hole and around the radial neck, and suture its ends together without tension, creating a new annular ligament.
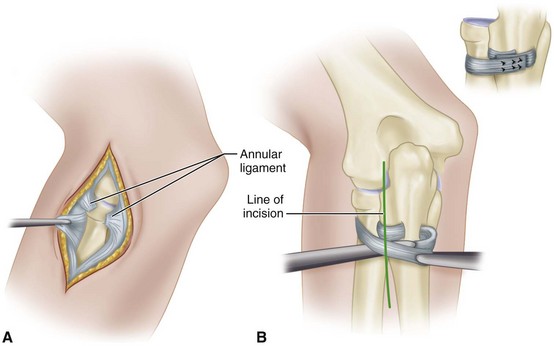
FIGURE 60-24 Dislocation of radial head. A, Annular ligament has been ruptured. Often, this ligament can be sutured satisfactorily. B, If necessary, annular ligament can be reconstructed with strip of fascia lata. Inset, Reconstruction has been completed. SEE TECHNIQUE 60-8.
Dislocation of Radial Head and Fracture of Proximal Third of Ulna (monteggia Fracture)
The treatment of a Monteggia fracture is described in Chapters 36 and 57.
Fracture-Dislocation of Elbow with Severe Damage of Soft Structures
Complex elbow dislocations with associated fractures may require surgical intervention to obtain joint stability. This typically includes ligament or fracture repair. A fracture-dislocation of the adult elbow in which the soft structures have been severely damaged should not be treated by closed methods but by débridement and repair. This operation occasionally is indicated if the radial head and the coronoid process of the ulna have been fractured and severe damage to the soft tissues is evident. Large periarticular fractures have been shown to affect functional results adversely. A fractured coronoid process strongly suggests that the elbow had become at least partially dislocated at the time of the injury. At surgery, the brachialis muscle may be found to be torn, the anterior part of the capsule of the elbow joint to be avulsed, and either one or both collateral ligaments to be ruptured. If the injuries of the soft structures are repaired at the same time as the injuries to the bone, the return of function can be hastened, the final range of motion can be improved, and the potential for myositis ossificans around the elbow can be reduced. This open reduction is only for fracture-dislocations of the elbow with severe damage (see Chapter 57 for ligament repair techniques). In a severe fracture-dislocation of the elbow, it is important to assess the integrity of the distal radioulnar joint.
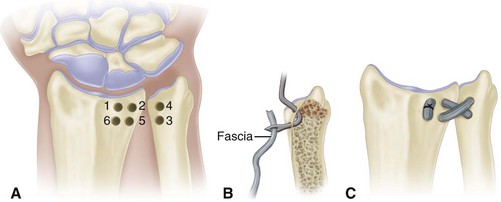
Distal Radioulnar Joint
A distal radioulnar dislocation can be dorsal or volar (Fig. 60-25). If the dislocation is with the ulna in the dorsal position, reduction usually is accomplished by supination of the forearm with pressure on the distal ulna. If the dislocation is with the ulna in the volar position, pronation of the forearm usually is successful in reducing the dislocation. An excellent result usually can be expected if it is reduced early and immobilized for 1 month in plaster. If the dislocation is less than 2 months old and cannot be reduced closed, open reduction with exposure and repair of the triangular fibrocartilage is advised. If the dislocation is reduced surgically after more than 2 months, consideration should be given to excision of the distal ulna and distal ligament reconstruction. According to Milch, rupture of the distal radioulnar ligaments usually causes diastasis of the distal radioulnar joint. He stated that this separation can be seen on radiographs and is a pathognomonic sign that the ligaments have been ruptured and should be repaired. Irreducible dislocations of the distal radioulnar joint have been described In most patients, the extensor carpi ulnaris was entrapped in the joint and prevented closed reduction. A dorsal approach was used to free the extensor carpi ulnaris, and repair of the triangular fibrocartilage or transosseous pinning was used to stabilize the joint.
Rupture of the ligaments around the distal radioulnar joint without a fracture usually is considered to be only a sprain, and the joint seldom is properly immobilized. The ligaments may not heal well, and, if not, the damage rarely is discovered before 6 to 8 weeks after injury. By this time, degenerative changes in the articular surfaces of the joint may have become so severe that restoring the normal radioulnar relationship would be undesirable. In these instances, resection of the distal ulna (see Chapter 58) usually is indicated; reconstruction of the ligaments is indicated only rarely. Operations to reconstruct permanently damaged ligaments of the distal radioulnar joint cannot be successful unless the component bones are undeformed.
Because operations to stabilize the distal radioulnar joint are so rarely indicated, the techniques for performing them are not described here. In Figures 60-26 and 60-27, two such operations are shown, and the reader is referred to the original works for details of the techniques. Acute dislocations of the wrist, the carpus, and the joints of the hand are discussed in Chapters 67 and 69.
Wolf JM, Athwal GS, Shin AY, Dennison DG. Acute trauma to the upper extremity: what to do and when to do it. J Bone Joint Surg. 2009;91A:1240.
Kiefer EA, Wikstrom EA, Douglas McDonald J. Ankle dislocation without fracture: an on-field perspective. Clin J Sport Med. 2006;16:269.
Ramasamy P, Ward A. Distal tibiofibular joint dislocation with an intact fibula: a classification system. Injury. 2003;34:862.
Shaik MM, Tandon T, Agrawal Y, et al. Medial and lateral rotatory dislocations of the ankle after trivial trauma—pathomechanics and results of two cases. J Foot Ankle Surg. 2006;45:346.
Uyar M, Tan A, Isler M, et al. Closed posteromedial dislocation of the tibiotalar joint without fracture in a basketball player. Br J Sports Med. 2004;38:342.
Ahmad CS, Stein BE, Matuz D, et al. Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation: a review of eight cases. Am J Sports Med. 2000;28:804.
Atkin DM, Fithian DC, Marangi KS, et al. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28:472.
Balcarek P, Ammon J, Frosch S, et al. Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity-trochlear groove distance. Arthroscopy. 2010;26:926.
Camanho GL, Viegas AD, Bitar AC, et al. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy. 2009;25:620.
Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114.
Mehta VM, Inoue M, Nomura E, Fithian DC. An algorithm guiding the evaluation and treatment of acute primary patellar dislocation. Sports Med Arthrosc Rev. 2007;15:78.
Palmu S, Kallio PE, Donnell ST, et al. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg. 2008;90A:463.
Satterfield WH, Johnson DL. Arthroscopic patellar “Bankart” repair after acute dislocation. Arthroscopy. 2005;21:627.
Sillanpää PJ, Mäenpää HM, Mattila VM, et al. Arthroscopic surgery for primary traumatic patellar dislocation. Am J Sports Med. 2008;36:2301.
Knee and Proximal Tibiofibular Joint
Lonner JH, Dupuy DE, Siliski JM. Comparison of magnetic resonance imaging with operative findings in acute traumatic dislocations of the adult knee. J Orthop Trauma. 2000;14:183.
Reckling FW, Peltier LF. Acute knee dislocations and their complications: 1969. Clin Orthop Relat Res. 2004;422:135.
Seikiya JK, Kuhn JE. Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg. 2003;11:120.
Ashraf T, Iraqi AA. Bilateral and posterior traumatic hip dislocation. J Orthop Trauma. 2001;15:367.
Brooks RA, Ribbans WJ. Diagnosis and imaging studies of traumatic hip dislocations in the adult. Clin Orthop Relat Res. 2000;377:15.
Cornwall R, Radomisli TE. Nerve injury in traumatic dislocation of the hip. Clin Orthop Relat Res. 2000;377:84.
Goddard NJ. Classification of traumatic hip dislocation. Clin Orthop Relat Res. 2000;377:11.
Moorman CT, III., Warren RF, Hershman EB, et al. Traumatic posterior hip subluxation in American football. J Bone Joint Surg. 2003;85A:1190.
Pape H-C, Rice J, Wolfram K, et al. Hip dislocation in patients with multiple injuries. Clin Orthop Relat Res. 2000;377:99.
Phillips AM, Konchwall A. The pathologic features and mechanism of traumatic dislocation of the hip. Clin Orthop Relat Res. 2000;377:7.
Rodriguez-Merchan EC. Coxarthrosis after traumatic hip dislocation in the adult. Clin Orthop Relat Res. 2000;377:92.
Rodriguez-Merchan EC. Osteonecrosis of the femoral head after traumatic hip dislocation in the adult. Clin Orthop Relat Res. 2000;377:68.
Tabuenca J, Truan JR. Knee injuries in traumatic hip dislocation. Clin Orthop Relat Res. 2000;377:78.
Yang EC, Cornwall R. Initial treatment of traumatic hip dislocations in the adult. Clin Orthop Relat Res. 2000;377:24.
Bradley JP, Elkousy H. Decision making: operative versus nonoperative treatment of acromioclavicular joint injuries. Clin Sports Med. 2003;22:277.
Brucker PU, Gruen GS, Kaufmann RA. Scapulothoracic dissociation: evaluation and management. Injury. 2005;36:1147.
Ceccarelli E, Bondi R, Alviti F, et al. Treatment of acute grade III acromioclavicular dislocation: a lack of evidence. J Orthopaed Traumatol. 2008;9:105.
Groh GI, Wirth MA, Rockwood CA. Treatment of traumatic posterior sternoclavicular dislocations. J Shoulder Elbow Surg. 2011;20:107.
Guttmann D, Paksima NE, Zukerman JD. Complications of treatment of complete acromioclavicular joint dislocation. Instr Course Lect. 2000;49:407.
Mazzocca A, Arciero R, Romeo A: Anatomic coracoclavicular reconstruction surgical technique, Technique Manual, Arthrex, Naples, FL, 2007.
Mouhsine E, Garofalo R, Crevoisier X, et al. Grade I and II acromioclavicular dislocations: results of conservative treatment. J Shoulder Elbow Surg. 2003;12:599.
Omer GE, Jr. Osteotomy of the clavicle in surgical reduction of anterior sternoclavicular dislocation. J Trauma. 1967;7:584.
Osti M, Seil R, Bachelier F, et al. Minimally invasive endoscopic reconstruction technique of acute AC-joint dislocations: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2006;14:686.
Waters PM, Bae DS, Kadiyala RK. Short-term outcomes after surgical treatment of traumatic posterior sternoclavicular fracture-dislocations in children and adolescents. J Pediatr Orthop. 2003;23:464.
Wolf EM, Pennington WT. Arthroscopic reconstruction for acromioclavicular joint dislocation. Arthroscopy. 2001;17:558.
Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576.
Burra G, Andrews JR. Acute shoulder and elbow dislocations in the athlete. Orthop Clin North Am. 2002;33:479.
DeBerardino TM, Arciero RA, Taylor DC, et al. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes: two- to five-year follow-up. Am J Sports Med. 2001;29:586.
Duralde XA, Fogle EF. The success of closed reduction in acute locked posterior fracture-dislocations of the shoulder. J Shoulder Elbow Surg. 2006;15:701.
Eachempati KK, Dua A, Malhotra R, et al. The external rotation method for reduction of acute anterior dislocations and fracture-dislocations of the shoulder. J Bone Joint Surg. 2004;86A:2431.
Kim SH, Ha KI, Cho YB, et al. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg. 2003;85A:1511.
Kirkley A, Werstine R, Ratjek A, et al. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21:55.
Larrain MV, Botto GJ, Montenegro HJ, et al. Arthroscopic repair of acute traumatic anterior shoulder dislocations in young athletes. Arthroscopy. 2001;17:373.
Mazzocca AD, Brown FM, Jr., Carreira DS, et al. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33:52.
Mihata T, Doi M, Abe M. Irreducible acute anterior dislocation of the shoulder caused by interposed fragment of the anterior glenoid rim. J Orthop Sci. 2000;5:404.
O’Driscoll SW, Jupiter JB, King GJ, et al. The unstable elbow. Instr Course Lect. 2001;50:89.
Sparks DR, DeLaRose J, Bergan JJ, et al. Arterial injury in uncomplicated upper extremity dislocations. Ann Vasc Surg. 2000;14:110.
Berthold M, Rikli DA. Elbow dislocation with multidirectional instability: avulsion of the triceps tendon; and injury to the ulnar, median, and radial nerves: case report. J Trauma. 2002;53:1176.
Deutch SR, Olsen BS, Jensen SL, et al. Ligamentous and capsular restraints to experimental posterior elbow joint dislocation. Scand J Med Sci Sports. 2003;13:311.
Lee BP, Teo LH. Surgical reconstruction for posterolateral rotatory instability of the elbow. J Shoulder Elbow Surg. 2003;12:476.
Lindenhovius ALC, Jupiter JB, Ring D. Comparison of acute versus subacute treatment of terrible triad injuries of the elbow. J Hand Surg. 2008;33A:920.
Lippe CN, Williams DP. Combined posterior and convergent elbow dislocations in an adult: a case report and review of the literature. J Bone Joint Surg. 2005;87A:1597.
Mehta JA, Bain GI. Elbow dislocations in adults and children. Clin Sports Med. 2004;23:609.
Mehta JA, Bain GI. Posterolateral rotatory instability of the elbow. J Am Acad Orthop Surg. 2004;12:405.
Rettig AC. Traumatic elbow injuries in the athlete. Orthop Clin North Am. 2002;33:509.
Sheps DM, Hildebrand KA, Boorman RS. Simple dislocations of the elbow: evaluation and treatment. Hand Clin. 2004;20:389.
Squires NA, Tomaino MM. Brachial artery rupture without median nerve dysfunction after closed elbow dislocation. Am J Orthop. 2003;32:298.
Symeonides PP, Grigoriadis NC, Natzokos IG. Anterior dislocation of the elbow. J Shoulder Elbow Surg. 2006;15:249.
Tashjian RZ, Katarincic J. Complex elbow instability. J Am Acad Orthop Surg. 2006;14:278.
Böhler L. The treatment of fractures, ed 4. Baltimore: William Wood & Co (translated by EW Hey Groves); 1936.
Stewart MJ. Unusual athletic injuries. Instr Course Lect. 1960;17:377.
Watson-Jones R. Fractures and joint injuries, ed 4. Baltimore: Williams & Wilkins; 1952.
Finkemeier C, Engegbretsen L, Gannon J. Tibial-talar dislocation without fracture: treatment principles and outcome. Knee Surg Sports Traumatol Arthrosc. 1995;3:47.
Cash JD, Hughston JC. Treatment of acute patellar dislocation. Am J Sports Med. 1988;16:244.
Dainer RD, Barrack RL, Buckley SL, et al. Arthroscopic treatment of acute patellar dislocations. Arthroscopy. 1988;4:267.
Goldthwait JE. Dislocation of the patella. Trans Am Orthop Assoc. 1985;8:237.
Goletz TH, Brodhead WT. Intra-articular dislocation of the patella: a case report. Orthopedics. 1981;9:1022.
Hawkins RJ, Bell K, Garth W. Acute patellar dislocation. Am J Sports Med. 1986;14:117.
Hughston JC. Subluxation of the patella. J Bone Joint Surg. 1968;50A:1003.
Hughston JC. Reconstruction of the extensor mechanism for subluxation of the patella. J Sports Med. 1972;1:6.
Jensen CM, Roosen JU. Acute traumatic dislocation of the patella. J Trauma. 1985;25:160.
Larsen E, Lauridsen F. Conservative treatment of patellar dislocations: influence of evident factors on the tendency to redislocation and therapeutic result. Clin Orthop Relat Res. 1982;171:131.
Maletius W, Gillquist J, Messner K. Acute patellar dislocation during eccentric muscle testing on the Biodex dynamometer. Arthroscopy. 1994;10:473.
Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14:513.
Nsouli AZ, Nahabedian AM. Intraarticular dislocation of the patella. J Trauma. 1988;28:256.
Pedersen P, Pedersen T. Conservative treatment of acute patellar dislocation. Adv Orthop Surg. 1989;12:205.
Sallay PI, Poggi J, Speer KP, et al. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24:52.
Stanitski CL. Articular hypermobility and chondral injury in patients with acute patellar dislocation. Am J Sports Med. 1995;23:146.
Stanitski CL, Paletta GA. Articular cartilage injury with acute dislocation in adolescents. Am J Sports Med. 1998;26:52.
Virolainen H, Visuri T, Kuusela T. Acute dislocation of the patella: MR findings. Radiology. 1993;189:243.
Knee and Proximal Tibiofibular Joint
Anderson RL. Dislocation of the knee: report of four cases. Arch Surg. 1945;46:598.
Brennan JJ, Krause ME, Macdonald WF. Irreducible posterolateral dislocation of the knee joint with grossly intact cruciate ligaments. Am J Surg. 1962;104:117.
Burman MS. Subluxation of the head of the fibula. Am J Surg. 1931;11:108.
Conwell HE. Dislocations of the knee joint. Am J Surg. 1939;43:492.
Conwell HE, Alldredge RH. Complete dislocations of the knee joint: a report of 7 cases with end-results. Surg Gynecol Obstet. 1937;64:94.
Kennedy JC. Complete dislocation of the knee joint. J Bone Joint Surg. 1963;45A:889.
Keogh P, Masterson E, Murphy B, et al. The role of radiography and computed tomography in the diagnosis of acute dislocation of the proximal tibiofibular joint. Br J Radiol. 1993;66:108.
Meyers MH, Harvey JPJr. Traumatic dislocations of the knee joint: a study of eighteen cases. J Bone Joint Surg. 1971;53A:16.
Meyers MH, Moore TM, Harvey JPJr. Follow-up notes on articles previously published in the Journal: traumatic dislocation of the knee joint. J Bone Joint Surg. 1975;57A:430.
Montgomery JB. Dislocation of the knee. Orthop Clin North Am. 1987;18:149.
Ogden JA. Dislocation of the proximal fibula. Radiology. 1972;105:547.
Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res. 1974;101:186.
Ogden JA. Subluxation and dislocation of the proximal tibiofibular joint. J Bone Joint Surg. 1974;56A:145.
Quinlan AG. Irreducible posterolateral dislocation of the knee with button-holing of the medial femoral condyle. J Bone Joint Surg. 1966;48A:1619.
Quinlan AG, Sharrard WJW. Posterolateral dislocation of the knee with capsular interposition. J Bone Joint Surg. 1958;40B:660.
Roman PD, Hopson CN, Zenni EJ, Jr. Traumatic dislocation of the knee: a report of 30 cases and literature review. Orthop Rev. 1987;16:917.
Shields L, Mital M, Cave EF. Complete dislocation of the knee: experience at the Massachusetts General Hospital. J Trauma. 1969;9:192.
Sisk TD, King LM: Unpublished data, 1983.
Thomasen PB, Rud B, Jensen UH. Stability and motion after traumatic dislocation of the knee. Acta Orthop Scand. 1984;55:278.
Twaddle BC, Hunter JC, Chapman JR, et al. MRI in acute knee dislocation: a prospective study of clinical, MRI, and surgical findings. J Bone Joint Surg. 1996;78B:573.
Voglino JA, Denton JR. Acute traumatic proximal tibiofibular joint dislocation confirmed by computed tomography. Orthopedics. 1999;22:255.
Watson-Jones R. Fractures and joint injuries. Edinburgh: E & S Livingstone; 1955.
Welling RE, Kakkasseril J, Cranley JJ. Complete dislocations of the knee with popliteal vascular injury. J Trauma. 1981;21:450.
Dahners LE, Hundley JD. Reduction of posterior hip dislocations in the lateral position using traction-countertraction: safer for the surgeon? J Orthop Trauma. 1999;13:373.
DeLee JC, Evans JA, Thomas J. Anterior dislocation of the hip and associated femoral-head fractures. J Bone Joint Surg. 1980;62A:960.
Dreinhöfer KE, Schwarzkopf SR, Haas NP, et al. Isolated traumatic dislocation of the hip: long-term results in 50 patients. J Bone Joint Surg. 1994;76B:6.
Epstein HC. Traumatic anterior and simple posterior dislocations of the hip in adults and children. Instr Course Lect. 1973;22:115.
Epstein HC. Traumatic dislocations of the hip. Clin Orthop Relat Res. 1973;92:116.
Epstein HC. Posterior fracture-dislocations of the hip. J Bone Joint Surg. 1974;56A:1103.
Gregory CF. Fractures and dislocations of the hip and fractures of the acetabulum: early complications of dislocation and fracture-dislocations of the hip joint. Instr Course Lect. 1973;22:105.
Hougaard K, Lindequist S, Nielsen LB. Computerized tomography after posterior dislocation of the hip. J Bone Joint Surg. 1987;69B:556.
Hougaard K, Thomsen PB. Traumatic posterior dislocation of the hip—prognostic factors influencing the incidence of osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 1986;106:32.
Hougaard K, Thomsen PB. Coxarthrosis following traumatic posterior dislocation of the hip. J Bone Joint Surg. 1987;69A:679.
Jaskulka RA, Fischer G, Fenzl G. Dislocation and fracture-dislocation of the hip. J Bone Joint Surg. 1991;73B:465.
Mac SS, Schein AJ. Rectus femoris muscle: an obstacle in reduction of acute traumatic anterior dislocation of the hip in an adult. Orthopedics. 1982;5:880.
Nordt WE, III. Maneuvers for reducing dislocated hips: a new technique and a literature review. Clin Orthop Relat Res. 1999;360:260.
Ordway CB, Xeller CF. Transverse computerized axial tomography of patients with posterior dislocation of the hip. J Trauma. 1984;24:76.
Patterson FP, Morton KS. Neurological complications of fractures and dislocations of the pelvis. J Trauma. 1972;12:1013.
Pietrafesa CA, Hoffman JR. Traumatic dislocation of the hip. JAMA. 1983;249:3342.
Reigstad A. Traumatic dislocation of the hip. J Trauma. 1980;20:603.
Sherlock DA. Traumatic anterior dislocation of the hip. J Trauma. 1988;28:411.
Slátis P, Latvala A. Irreducible traumatic posterior dislocation of the hip. Injury. 1971;5:188.
Stewart MJ, Milford LW. Fracture-dislocation of the hip: an end-result study. J Bone Joint Surg. 1954;36A:315.
Thompson VP, Epstein HC. Traumatic dislocation of the hip: a survey of 204 cases covering a period of 21 years. J Bone Joint Surg. 1951;33A:746.
Toni A, Gulino G, Baldini N, et al. Clinical and radiographic long-term results of acetabular fractures associated with dislocations of the hip. Ital J Orthop Traumatol. 1985;11:443.
Tornetta P, III., Mostafavi HR. Hip dislocation: current treatment regimens. J Am Acad Orthop Surg. 1997;5:27.
Upadhyay SS, Moulton A. The long-term results of traumatic posterior dislocation of the hip. J Bone Joint Surg. 1981;63B:548.
Upadhyay SS, Moulton A, Srikrishnamurthy K. An analysis of the late effects of traumatic posterior dislocation of the hip without fractures. J Bone Joint Surg. 1983;65B:150.
Urist MR. Fracture-dislocation of the hip joint. J Bone Joint Surg. 1948;30A:699.
Weber M, Ganz R. Recurrent traumatic dislocation of the hip: report of a case and review of the literature. J Orthop Trauma. 1997;11:382.
Ahstrom JP, Jr. Surgical repair of complete acromioclavicular separation. JAMA. 1971;217:785.
Alldredge RH. Surgical treatment of acromioclavicular dislocations. J Bone Joint Surg. 1965;47A:1278.
Bannister GC, Wallace WA, Stableforth PG, et al. The management of acute acromioclavicular dislocations: a randomised prospective controlled trial. J Bone Joint Surg. 1989;71B:848.
Bannister GC, Wallace WA, Stableforth PG, et al. A classification of acute acromioclavicular dislocation: a clinical radiological and anatomical study. Injury. 1992;23:194.
Bearden JM, Hughston JC, Whatley GS. Acromioclavicular dislocation: method of treatment. Am J Sports Med. 1973;1:5.
Bjerneld H, Hovelius L, Thorling J. Acromioclavicular separation treated conservatively: five-year follow-up study. Acta Orthop Scand. 1983;54:743.
Bosworth BM. Acromioclavicular separation: new method of repair. Surg Gynecol Obstet. 1941;73:866.
Brown JE. Anterior sternoclavicular dislocation: a method of repair. Am J Orthop. 1961;3:184.
Brown JE, Stanley RF, Tullos HS. Acromioclavicular joint dislocations: comparative results following operative treatment with and without primary distal clavisectomy. Am J Sports Med. 1977;5:258.
Buckerfield CT, Castle ME. Acute traumatic retrosternal dislocation of the clavicle. J Bone Joint Surg. 1984;66A:379.
Bundens WD, Cook JI. Repair of acromioclavicular separations by deltoid-trapezius imbrication. Clin Orthop Relat Res. 1961;20:109.
Cook FF, Tibone JE. The Mumford procedure in athletes: an objective analysis of function. Am J Sports Med. 1988;16:97.
Copeland S, Kessel L. Disruption of the acromioclavicular joint: surgical anatomy and biological reconstruction. Injury. 1980;11:208.
Darrow JC, Jr., Smith JA, Lockwood RC. A new conservative method for treatment of type III acromioclavicular separations. Orthop Clin North Am. 1980;11:727.
DePalma AF. Surgical anatomy of acromioclavicular and sternoclavicular joints. Surg Clin North Am. 1963;43:1541.
Dewar FP, Barrington TW. The treatment of chronic acromioclavicular dislocation. J Bone Joint Surg. 1965;47B:32.
Dias JJ, Steingold RF, Richardson RA, et al. The conservative treatment of acromioclavicular dislocation: review after five years. J Bone Joint Surg. 1987;69B:719.
Dumontier C, Sautet A, Man M, et al. Acromioclavicular dislocations: treatment by coracoacromial ligamentoplasty. J Shoulder Elbow Surg. 1995;4:130.
Ejeskär A. Coracoclavicular wiring for acromioclavicular joint dislocation: a ten-year follow-up study. Acta Orthop Scand. 1974;45:652.
Eskola A, Vainionpää S, Korkala S, et al. Four-year outcome of operative treatment of acute acromioclavicular dislocation. J Orthop Trauma. 1991;5:9.
Féry A, Sommelet J. Dislocation of the sternoclavicular joint: a review of 49 cases. Int Orthop. 1988;12:187.
Fukuda K, Craig EV, An KN, et al. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg. 1986;68A:434.
Galpin RD, Hawkins RJ, Grainger RW. A comparative analysis of operative versus nonoperative treatment of grade III acromioclavicular separations. Clin Orthop Relat Res. 1985;193:150.
Gerber C, Rockwood CAJr. Subcoracoid dislocation of the lateral end of the clavicle: a report of 3 cases. J Bone Joint Surg. 1987;69A:924.
Gillespie HS. Excision of the outer end of the clavicle for dislocation of the acromioclavicular joint. Can J Surg. 1964;7:18.
Gurd FB. The treatment of complete dislocation of the outer end of the clavicle. Ann Surg. 1941;113:1094.
Heinig CF. Retrosternal dislocation of the clavicle: early recognition, x-ray diagnosis, and management. J Bone Joint Surg. 1968;50A:830.
Hobbs DW. Sternoclavicular joint: a new axial radiographic view. Radiology. 1968;90:801.
Horn JS. The traumatic anatomy and treatment of acute acromioclavicular dislocation. J Bone Joint Surg. 1954;36B:194.
Jacobs B, Wade PA. Acromioclavicular-joint injury: an end-result study. J Bone Joint Surg. 1966;48A:475.
Jalovaara P, Päivänsalo M, Myllylä V, et al. Acute acromioclavicular dislocations treated by fixation of the joint and ligament repair or reconstruction. Acta Orthop Belg. 1991;57:296.
Jay GR, Monnet JC: The Bosworth screw in acute dislocations of the acromioclavicular joint. Paper presented at clinical conference, University of Oklahoma Medical Center, April 1969.
Kattan KR. Modified view for use in roentgen examination of the sternoclavicular joints. Radiology. 1973;108:8.
Kennedy JC. Retrosternal dislocation of the clavicle. J Bone Joint Surg. 1949;31B:74.
Kennedy JC. Complete dislocation of the acromioclavicular joint: 14 years later. J Trauma. 1968;8:311.
Kennedy JC, Cameron H. Complete dislocation of the acromioclavicular joint. J Bone Joint Surg. 1954;36B:202.
Lancaster S, Horowitz M, Alonso J. Complete acromioclavicular separations: a comparison of operative methods. Clin Orthop Relat Res. 1987;216:809.
Larsen E, Bjerg-Nielsen A, Christensen P. Conservative or surgical treatment of acromioclavicular dislocations: a prospective, controlled, randomized study. J Bone Joint Surg. 1986;68A:552.
Lemos MJ. The evaluation and treatment of the injured acromioclavicular joints in athletes. Am J Sports Med. 1998;26:137.
Lizaur A, Marco L, Cebrian R. Acute dislocation of the acromioclavicular joint: traumatic anatomy and the importance of deltoid and trapezius. J Bone Joint Surg. 1994;76B:602.
McPhee IB. Inferior dislocation of the outer end of the clavicle. J Trauma. 1980;20:709.
Moseley HF. Athletic injuries to the shoulder region. Am J Surg. 1959;98:401.
Mumford EB. Acromioclavicular dislocation: a new operative treatment. J Bone Joint Surg. 1941;23:799.
Murray JWG. Reconstruction of the dislocated acromioclavicular joint: a simplified method. Orthop Rev. 1973;2:55.
Neer CS, II. Shoulder reconstruction. Philadelphia: Saunders; 1990.
Neviaser JS. Acromioclavicular dislocation treated by transference of the coraco-acromial ligament: a long-term follow-up in a series of 112 cases. Clin Orthop Relat Res. 1968;58:57.
Neviaser JS. Injuries of the clavicle and its articulations. Orthop Clin North Am. 1980;11:233.
Patterson WR. Inferior dislocation of the distal end of the clavicle. J Bone Joint Surg. 1967;49A:1184.
Petersson CJ. Resection of the lateral end of the clavicle: 3- to 30-year follow-up. Acta Orthop Scand. 1983;54:904.
Phemister DB. The treatment of dislocation of the acromioclavicular joint by open reduction and threaded-wire fixation. J Bone Joint Surg. 1942;24:166.
Rockwood CA, Jr. Dislocations of the sternoclavicular joint. Instr Course Lect. 1975;24:144.
Rockwood CA, Jr., Green DP, Fractures, vol 1, Philadelphia, Lippincott, 1966.
Roper BA, Levack B. Surgical treatment of acromioclavicular dislocations. J Bone Joint Surg. 1982;64B:597.
Rosenørn M, Pederson EB. A comparison between conservative and operative treatment of acute acromioclavicular dislocation. Acta Orthop Scand. 1974;45:50.
Rosenørn M, Pedersen EB. The significance of the coracoclavicular ligament in experimental dislocation of the acromioclavicular joint. Acta Orthop Scand. 1974;45:346.
Rowe CR. Dislocations of the shoulder. In: Rowe, CR, ed. The shoulder. New York: Churchill Livingstone, 1988.
Sage FP, Salvatore JE. Injuries of the acromioclavicular joint: a study of results in 96 patients. South Med J. 1963;56:486.
Selesnick FH, Jablon M, Frank C, et al. Retrosternal dislocation of the clavicle: report of four cases. J Bone Joint Surg. 1984;66A:287.
Skjeldl S, Lundblad R, Dullerud R. Coracoid process transfer for acromioclavicular dislocation. Acta Orthop Scand. 1988;59:180.
Smith MJ, Stewart MJ. Acute acromioclavicular separations: a 20-year study. Am J Sports Med. 1979;7:62.
Sundaram N, Patel DV, Porter DS. Stabilization of acute acromioclavicular dislocation by a modified Bosworth technique: a long-term follow-up study. Injury. 1992;23:189.
Taft TN, Wilson FC, Oglesby JW. Dislocation of the acromioclavicular joint: an end-result study. J Bone Joint Surg. 1987;69A:1045.
Urist MR. Complete dislocations of the acromioclavicular joint: the nature of the traumatic lesion and effective methods of treatment with an analysis of forty-one cases. J Bone Joint Surg. 1946;28:813.
Vere-Hodge N. Coraco-clavicular fixation by screw. In: Watson Jones, R, ed. Fractures and joint injuries. Baltimore: Williams & Wilkins, 1946.
Walsh WM, Peterson DA, Shelton G, et al. Shoulder strength following acromioclavicular injury. Am J Sports Med. 1985;13:153.
Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg. 1972;54A:1187.
Weinstein DM, McCann PD, McIlveen SJ, et al. Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med. 1995;23:324.
Weitzman G. Treatment of acute acromioclavicular joint dislocation by a modified Bosworth method. J Bone Joint Surg. 1967;49A:1167.
Wirth MA, Rockwood CA, Jr. Acute and chronic traumatic injuries of the sternoclavicular joint. J Am Acad Orthop Surg. 1996;4:268.
Worman LW, Leagus C. Intrathoracic injury following retrosternal dislocation of the clavicle. J Trauma. 1967;7:416.
Zaricznyj B. Late reconstruction of the ligaments following acromioclavicular separation. J Bone Joint Surg. 1976;58A:792.
Arciero RA, St. Pierre P: Acute shoulder dislocation: indications and techniques for operative management. Clin Sports Med. 1995;14:937.
Arciero RA, Wheeler JH, Ryan JB, et al. Arthroscopic Bankart repair versus nonoperative treatment for acute initial anterior shoulder dislocations. Am J Sports Med. 1994;22:589.
Baker CL, Uribe JW, Whitman C. Arthroscopic evaluation of acute initial anterior shoulder dislocations. Am J Sports Med. 1990;18:25.
DeBerardino TM, Arciero RA, Taylor DC. Arthroscopic stabilization of acute initial anterior shoulder dislocation: the West Point experience. J South Orthop Assoc. 1996;5:263.
DePalma AF. Surgery of the shoulder. Philadelphia: Lippincott; 1950.
Kuhnen W, Groves RJ. Irreducible acute anterior dislocation of the shoulder: a case report. Clin Orthop Relat Res. 1979;139:167.
Moseley HF. Athletic injuries to the shoulder region. Am J Surg. 1959;98:401.
Neviaser RJ, Neviaser TJ, Neviaser JS. Concurrent rupture of the rotator cuff and anterior dislocation of the shoulder in the older patient. J Bone Joint Surg. 1988;70A:1308.
Nicola FG, Ellman H, Eckardt J, et al. Bilateral posterior fracture-dislocation of the shoulder treated with a modification of the McLaughlin procedure. J Bone Joint Surg. 1981;63A:1175.
Norlin R. Intraarticular pathology in acute, first-time anterior shoulder dislocation: an arthroscopic study. Arthroscopy. 1993;9:546.
Oni OOA. Irreducible acute anterior dislocation of the shoulder due to a loose fragment from an associated fracture of the greater tuberosity. Injury. 1983;15:138.
Salmon JM, Bell SN. Arthroscopic stabilization of the shoulder for acute primary dislocations using a transglenoid suture technique. Arthroscopy. 1998;14:143.
Seradge H, Orme G. Acute irreducible anterior dislocation of the shoulder. J Trauma. 1982;22:330.
Simonet WT, Melton LJ, III., Cofield RH, et al. Incidence of anterior shoulder dislocations in Olmstead County, Minn. Clin Orthop Relat Res. 1984;186:186.
Borris LC, Lassen MR, Christensen CS. Elbow dislocation in children and adults: a long-term follow-up of conservatively treated patients. Acta Orthop Scand. 1987;58:649.
Cohen MS, Hastings H, II. Acute elbow dislocation: evaluation and management. J Am Acad Orthop Surg. 1998;6:15.
Hildebrand KA, Patterson SD, King GJ. Acute elbow dislocations: simple and complex. Orthop Clin North Am. 1999;30:63.
Josefsson PO, Gentz C-F, Johnell O, et al. Surgical versus nonsurgical treatment of ligamentous injuries following dislocation of the elbow joint: a prospective randomized study. J Bone Joint Surg. 1987;69A:605.
Josefsson PO, Johnell O, Gentz CF. Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg. 1984;66A:927.
Josefsson PO, Johnell O, Wendenberg B. Ligamentous injuries in dislocations of the elbow joint. Clin Orthop Relat Res. 1987;221:221.
Mehlhoff TL, Noble PC, Bennett JB, et al. Simple dislocation of the elbow in the adult: results after closed treatment. J Bone Joint Surg. 1988;70A:244.
Neviaser RJ, LeFevre GW. Irreducible isolated dislocation of the radial head: a case report. Clin Orthop Relat Res. 1971;80:72.
Pheasant H: Primary operative repair in severe elbow injuries, personal communication, 1950.
Stewart MJ. Mobilization of the elbow joint following injury or disease. J Phys Ment Rehabil. 1952;5:5.
Bruckner JD, Alexander AH, Lichtman DM. Acute dislocations of the distal radioulnar joint. Instr Course Lect. 1996;45:27.
Cetti NE. An unusual case of blocked reduction of the Galeazzi injury. Injury. 1977;9:59.
Dameron TBJr. Traumatic dislocation of the distal radio-ulnar joint. Clin Orthop Relat Res. 1972;83:55.
Gleason TF, Goldstein WM. Traumatic recurrent posterior dislocation of the radial head: a case report. Clin Orthop Relat Res. 1984;184:186.
Hanel DP, Scheid DK. Irreducible fracture-dislocation of the distal radioulnar joint secondary to entrapment of the extensor carpi ulnaris tendon. Clin Orthop Relat Res. 1988;234:56.
Jenkins NH, Mintowt-Czyz WJ, Fairclough JA. Irreducible dislocation of the distal radioulnar joint. Injury. 1987;18:40.
Liebolt FL. A new method for repair of the distal radioulnar ligaments. N Y State J Med. 1950;50:2817.
Liebolt FL. A new procedure for the treatment of luxation of the distal end of the ulna. J Bone Joint Surg. 1953;35A:261.
Milch H. Dislocation of the inferior end of the ulna: suggestions for new operative procedure. Am J Surg. 1926;1:141.