104
Acute cutaneous
lupus erythematosus
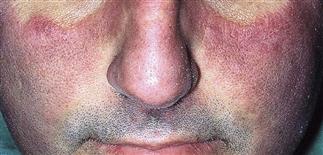
Violaceous malar plaques are evident, also involving the nose but sparing the nasolabial folds.

Violaceous patches and erosions in a photodistribution on the face—the characteristic ‘butterfly’ rash. Evaluation for systemic disease is essential.

Violaceous papules of acute lupus, nearly coalescing in a photodistribution of the upper chest and extensor arms.

Acute cutaneous lupus affecting the hands. The lesions are violaceous macules and patches scattered on the palmar surface.
DESCRIPTION
Serious multisystem disease associated with autoantibody formation. May involve skin, joints, or hematopoietic, pulmonary, renal, or central nervous system.
HISTORY
• Women affected more often than men, in a ratio of 8 : 1. • Occurs most frequently in people aged 30–40 years. • Sunlight exacerbates acute cutaneous lupus erythematosus and may induce it. • A multisystem disease; may be fever, arthritis, renal, cardiac, pulmonary, and central nervous system involvement. • Assessing lupus erythematosus rashes and categorizing the process as chronic cutaneous lupus, subacute cutaneous lupus, or acute lupus is vital to effective and appropriate treatment. It involves careful attention to systemic symptoms, and hematologic, renal, and serologic evaluation. • Constitutional symptoms of fatigue, weight loss, fever, and myalgias are more often present in patients with systemic disease.
PHYSICAL FINDINGS
• Superficial and indurated, non-pruritic, erythematous to violaceous plaques appear on sun-exposed chest, shoulders, extensor arms, and backs of hands. • May be fine scaling on the surface, and obvious follicular plugging. • In 10–50% of patients, a ‘butterfly’ rash appears over malar area and nasal bridge. • Atrophy does not occur. • Nail fold capillary microscopy reveals tortuous, ‘meandering’ capillary loops. • The patient may have excess vellus hair at the frontal margin (lupus hair) or diffuse hair thinning. • Alopecia (scarring and non-scarring) occurs in 20% of cases. • Obtain biopsy of lesional skin for routine study. • Underlying systemic lupus erythematosus is screened for by using an antinuclear antibody titer, a complete blood count, a serum chemistry profile, and urinalysis. Antibodies to dsDNA are associated with acute cutaneous lupus.
TREATMENT
• Sunscreens are an essential aspect of therapy. A broad-spectrum, water-resistant sunscreen should be applied daily. • Topical steroids, groups II–V, may be used twice daily on affected skin. • Immunomodulators such as tacrolimus ointment (Protopic) may be tried b.i.d. • Hydroxychloroquine 200 mg b.i.d. is a standard treatment for systemic and cutaneous disease. Response to therapy is slow, over 2–3 months. • Other options for systemic disease include prednisone, azathioprine, cyclophosphamide, mycophenolate mofetil.







