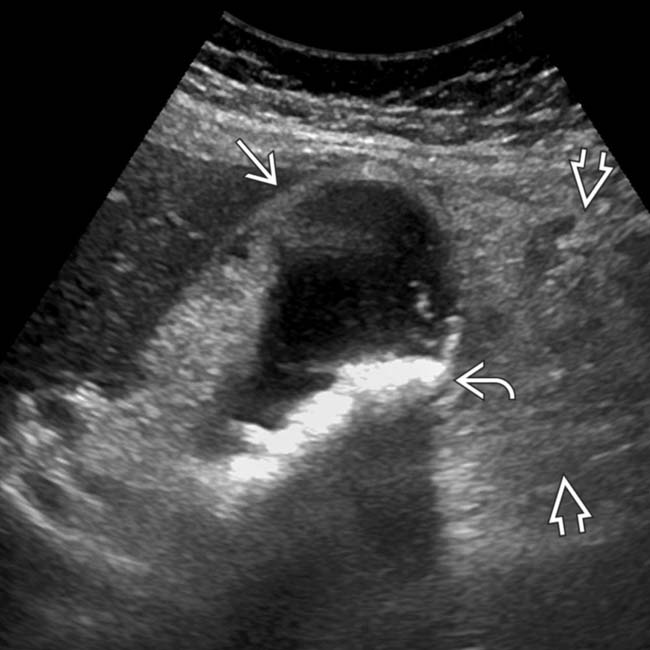
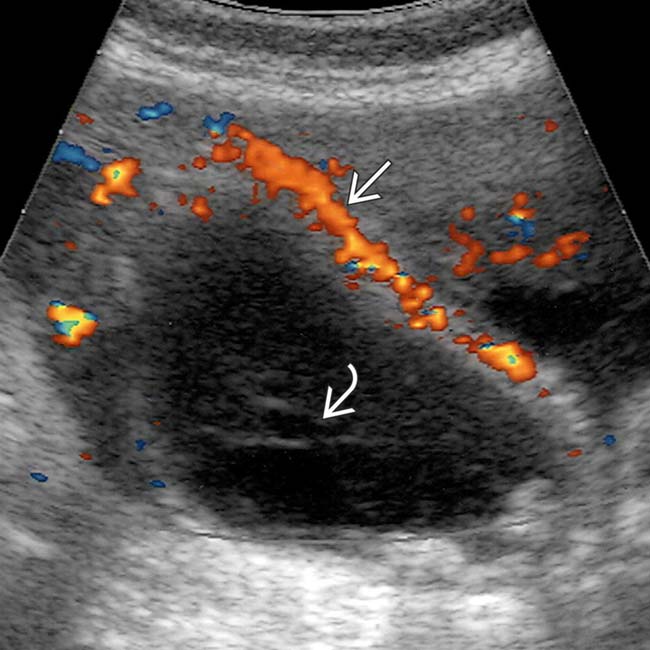
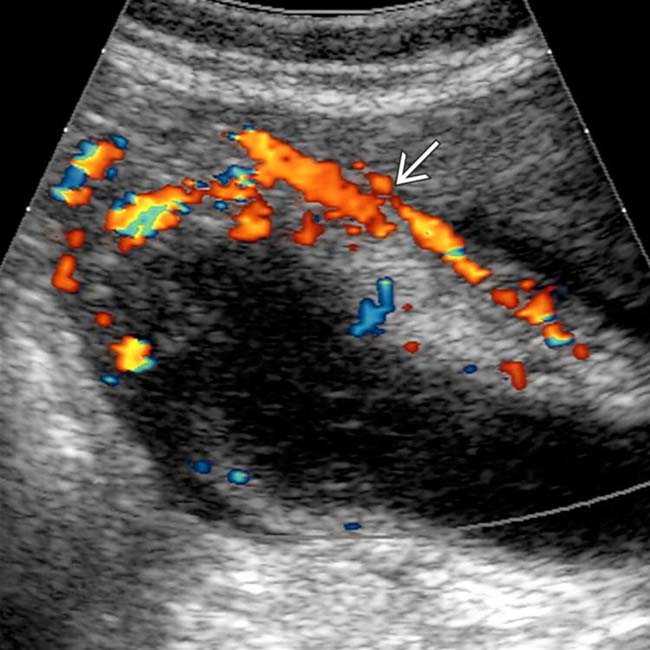
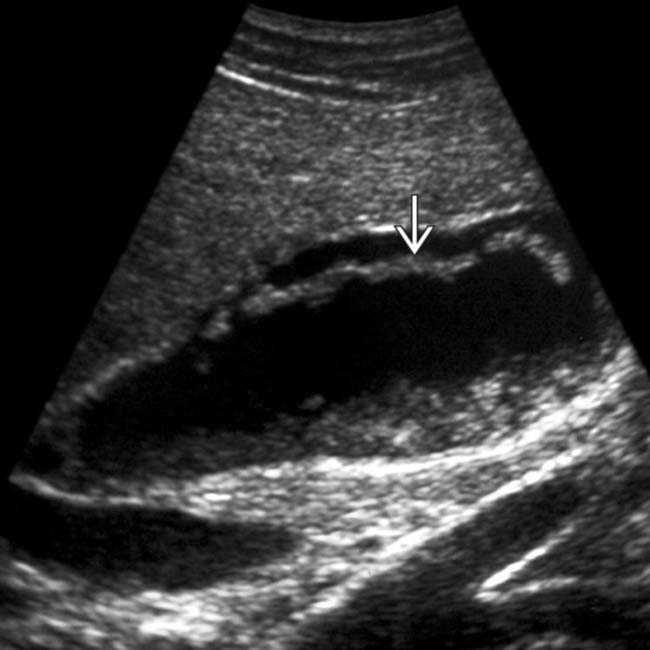
Cholelithiasis, sonographic Murphy sign, and GB wall thickening
• CT findings

 with an acoustic shadow
with an acoustic shadow  and a thickened gallbladder (GB) wall. These findings, along with a positive sonographic Murphy sign, suggested acute cholecystitis, confirmed at surgery.
and a thickened gallbladder (GB) wall. These findings, along with a positive sonographic Murphy sign, suggested acute cholecystitis, confirmed at surgery.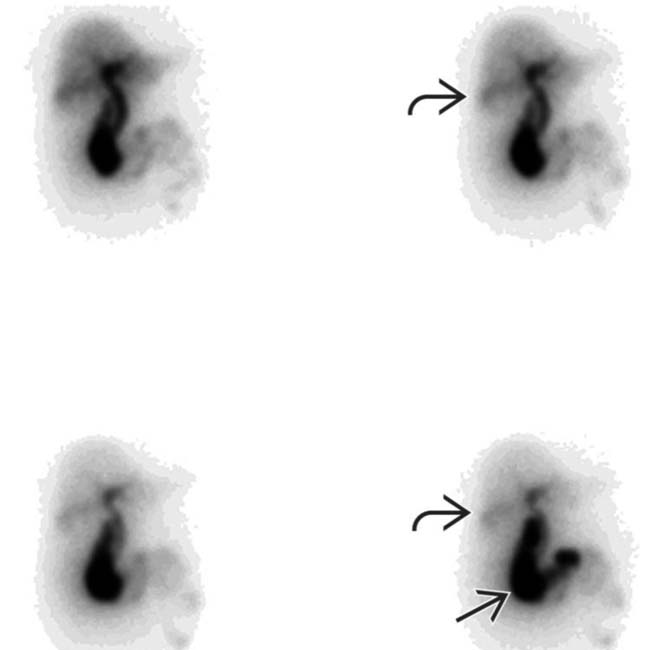
 , absence of GB activity, and a subtle GB fossa rim sign
, absence of GB activity, and a subtle GB fossa rim sign  . Persistent pericholecystic activity may be due to tissue edema and biliary stasis.
. Persistent pericholecystic activity may be due to tissue edema and biliary stasis.
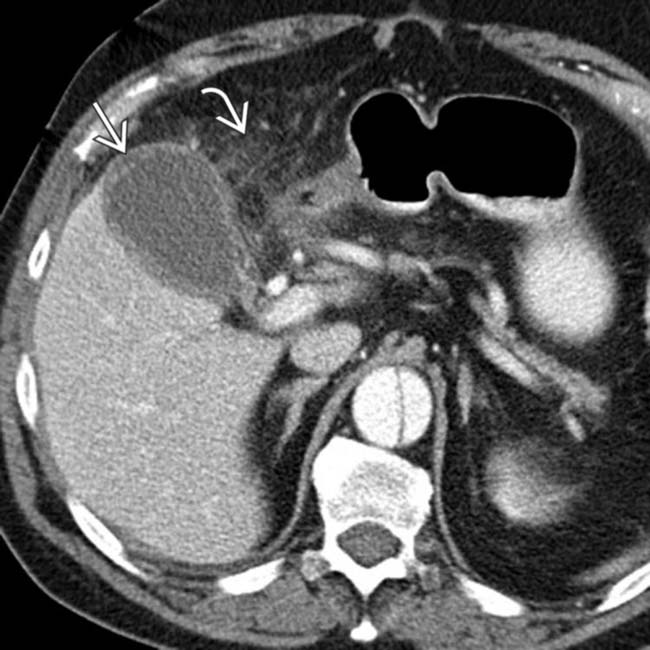
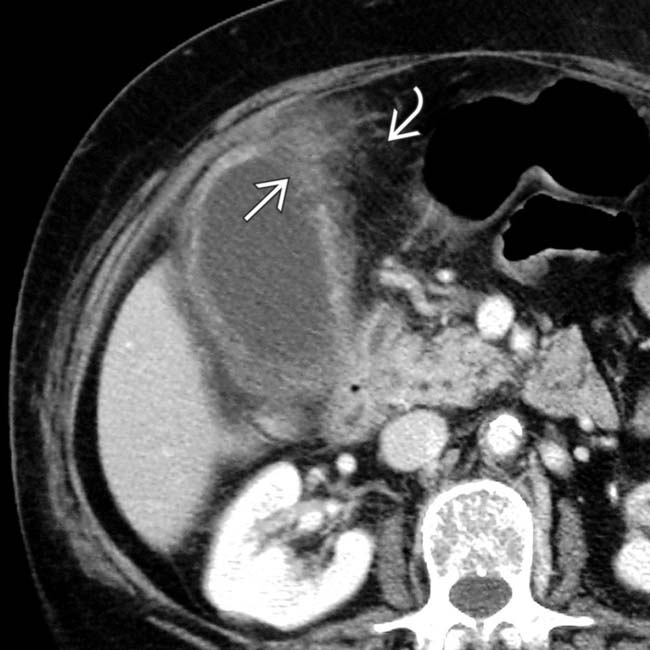
 within the gallbladder, with thickening of the GB wall, pericholecystic free fluid
within the gallbladder, with thickening of the GB wall, pericholecystic free fluid  , and fat stranding
, and fat stranding  , a constellation of findings diagnostic of acute cholecystitis.
, a constellation of findings diagnostic of acute cholecystitis.
 . This surrounding hepatic parenchymal hyperemia is analogous to the rim sign of hepatobiliary scintigraphy.
. This surrounding hepatic parenchymal hyperemia is analogous to the rim sign of hepatobiliary scintigraphy.IMAGING
General Features
CT Findings
• Uncomplicated cholecystitis
 GB wall thickening (> 3 mm) with mural and mucosal hyperenhancement and pericholecystic fat stranding
GB wall thickening (> 3 mm) with mural and mucosal hyperenhancement and pericholecystic fat stranding
 GB wall thickening (> 3 mm) with mural and mucosal hyperenhancement and pericholecystic fat stranding
GB wall thickening (> 3 mm) with mural and mucosal hyperenhancement and pericholecystic fat strandingUltrasonographic Findings
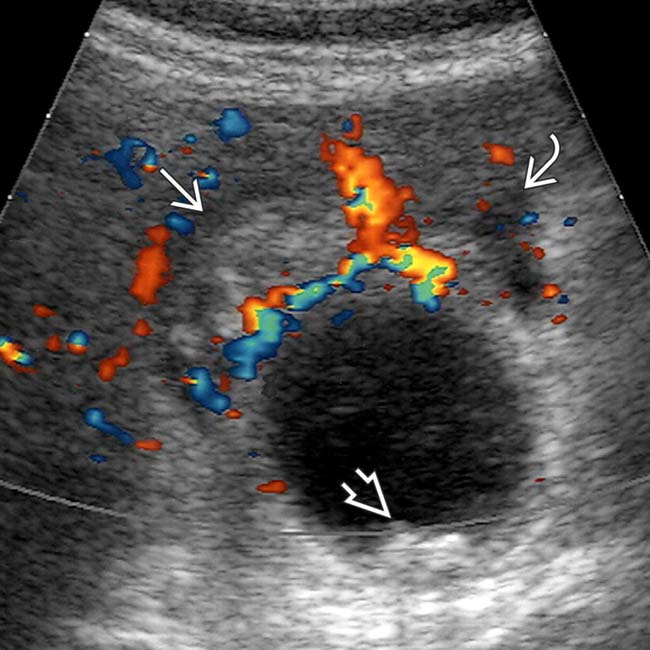
• Grayscale ultrasound
 Uncomplicated cholecystitis
Uncomplicated cholecystitis
 Complicated cholecystitis
Complicated cholecystitis
 Uncomplicated cholecystitis
Uncomplicated cholecystitis
 Complicated cholecystitis
Complicated cholecystitis
– Perforated cholecystitis: Pericholecystic abscess with collapsed GB
– Gangrenous cholecystitis: Asymmetric wall thickening, intraluminal linear membranes, and irregularity and ulcerations of GB wall
Nuclear Medicine Findings
• Hepatobiliary scintigraphy
 Nonvisualization of GB 4 hours after radiotracer injection (or 30 minutes after morphine administration)
Nonvisualization of GB 4 hours after radiotracer injection (or 30 minutes after morphine administration)
 Nonvisualization of GB 4 hours after radiotracer injection (or 30 minutes after morphine administration)
Nonvisualization of GB 4 hours after radiotracer injection (or 30 minutes after morphine administration)PATHOLOGY
General Features
CLINICAL ISSUES
Presentation
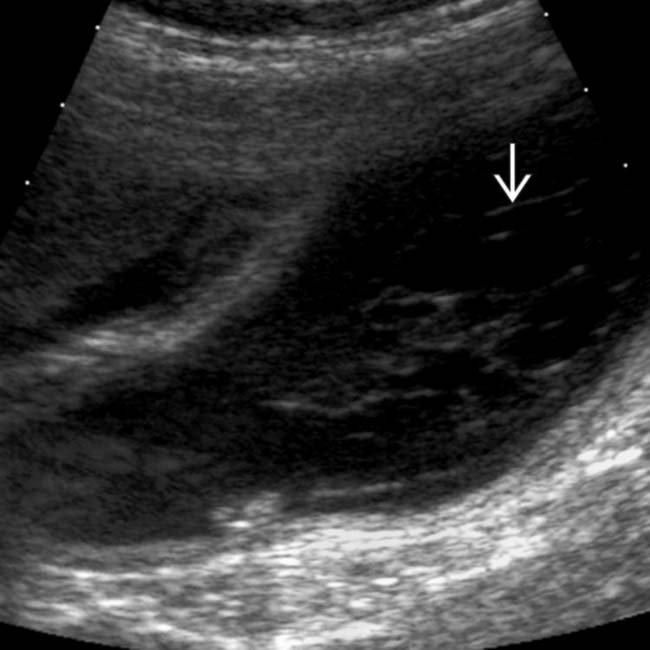
 with adjacent fat stranding
with adjacent fat stranding  , suggesting acute cholecystitis.
, suggesting acute cholecystitis.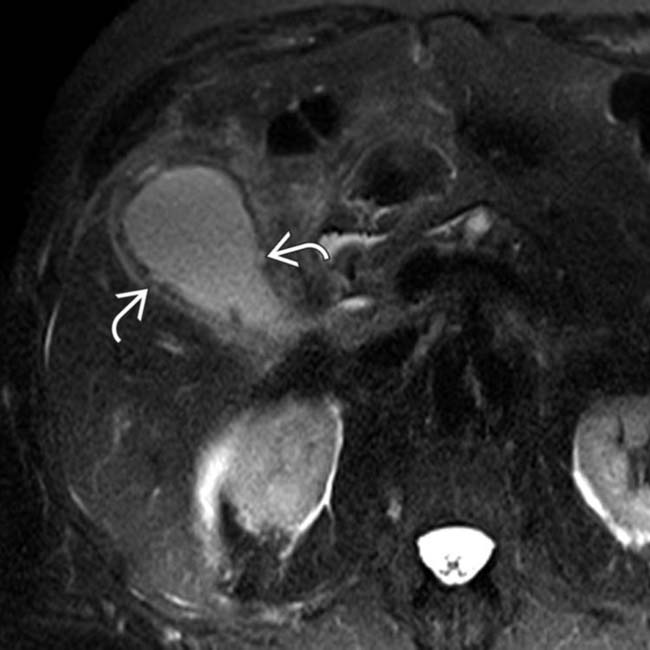
 . This was confirmed to represent gangrenous cholecystitis at surgery.
. This was confirmed to represent gangrenous cholecystitis at surgery.
 near the fundus. Most importantly, there is active extravasation
near the fundus. Most importantly, there is active extravasation  within the GB lumen, in keeping with this patient’s surgically confirmed hemorrhagic cholecystitis.
within the GB lumen, in keeping with this patient’s surgically confirmed hemorrhagic cholecystitis.
 , with similar density blood tracking in Morison pouch and medial to the GB
, with similar density blood tracking in Morison pouch and medial to the GB  . At surgery, the GB was gangrenous and contained hemorrhagic bile.
. At surgery, the GB was gangrenous and contained hemorrhagic bile.
 . There also appears to be a collection of gas more medially
. There also appears to be a collection of gas more medially  . Ureteral stents
. Ureteral stents  and surgical clips are noted from the patient’s recent surgery.
and surgical clips are noted from the patient’s recent surgery.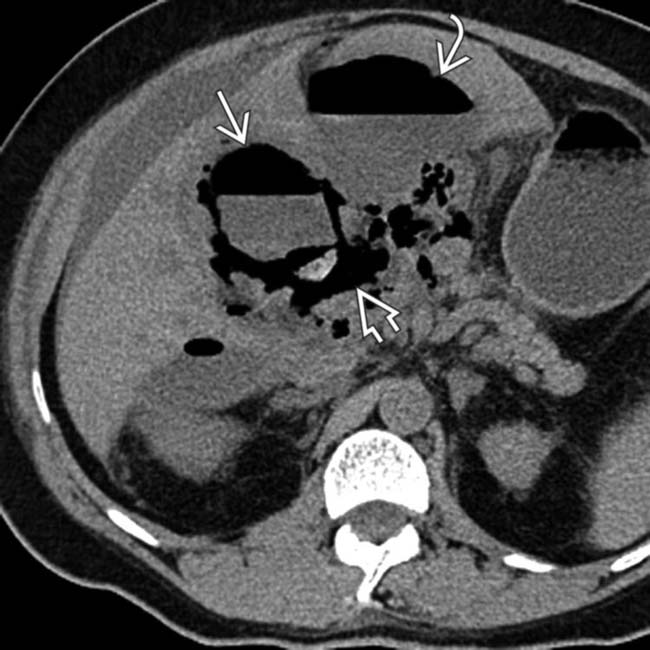
 in the GB lumen and wall. The fluid/gas
in the GB lumen and wall. The fluid/gas  tracking outward from the GB, as well as the adjacent gas and fluid collection
tracking outward from the GB, as well as the adjacent gas and fluid collection  , are consistent with perforation.
, are consistent with perforation.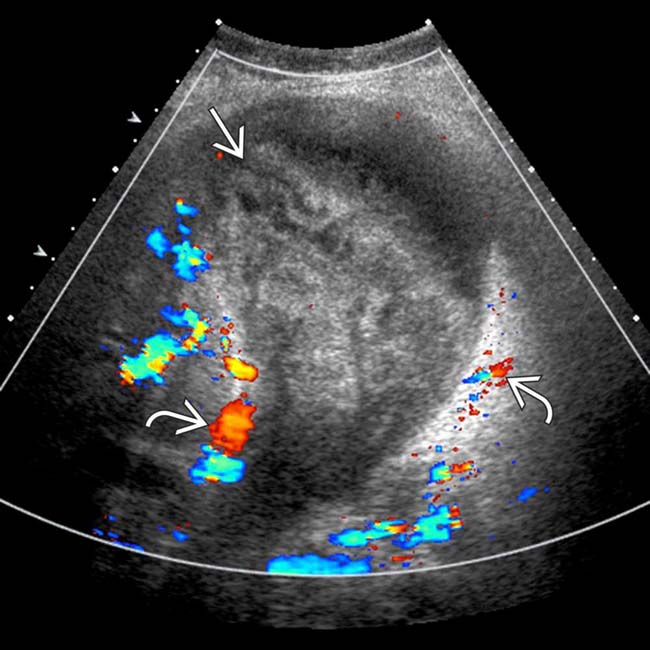
 , suggesting acute cholecystitis. However, the GB is distended and filled with high-density, heterogeneous blood products
, suggesting acute cholecystitis. However, the GB is distended and filled with high-density, heterogeneous blood products  , suggesting hemorrhagic cholecystitis.
, suggesting hemorrhagic cholecystitis.
 within the GB, which appears thickened and inflamed, in keeping with acute cholecystitis.
within the GB, which appears thickened and inflamed, in keeping with acute cholecystitis.
 within the GB lumen, suggesting acute hemorrhagic cholecystitis.
within the GB lumen, suggesting acute hemorrhagic cholecystitis.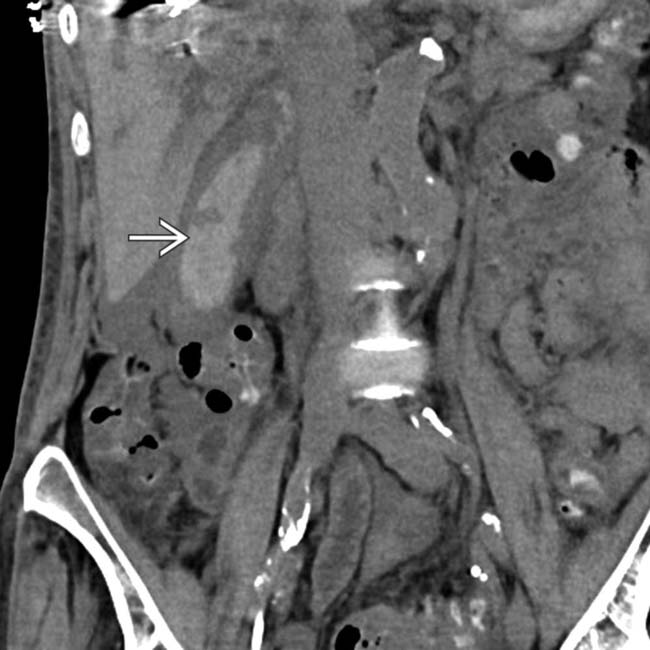
 has grown and now fills much of the GB lumen.
has grown and now fills much of the GB lumen.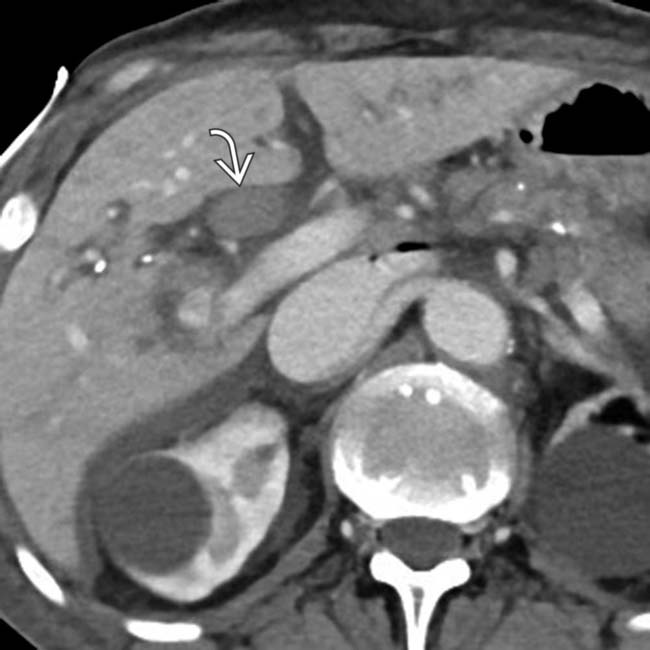
 distending and filling the common bile duct. Hemorrhagic cholecystitis in this patient was thought to be secondary to a recent embolization procedure.
distending and filling the common bile duct. Hemorrhagic cholecystitis in this patient was thought to be secondary to a recent embolization procedure.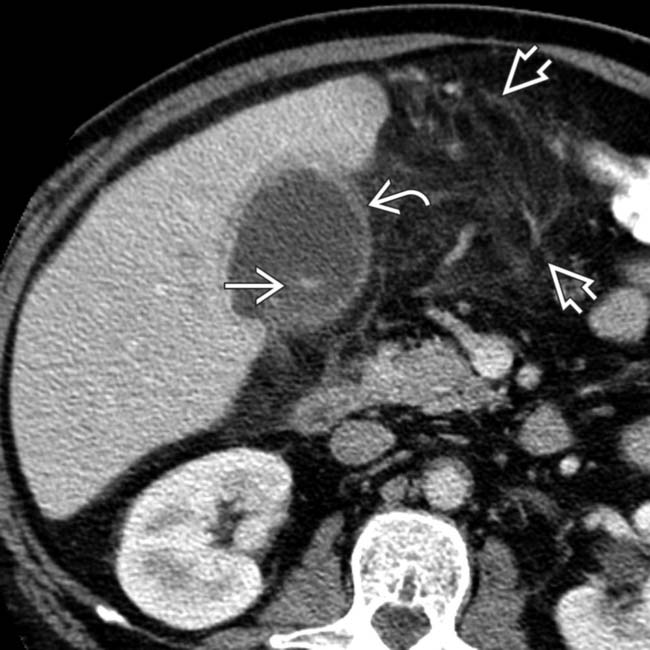
 , omental infiltration
, omental infiltration  , and subtle layering of calcified stones
, and subtle layering of calcified stones  .
.
 , mild GB thickening
, mild GB thickening  , and sludge. Omentum is infiltrated
, and sludge. Omentum is infiltrated  , and an unequivocal sonographic Murphy sign was easily elicited to make the diagnosis of acute cholecystitis.
, and an unequivocal sonographic Murphy sign was easily elicited to make the diagnosis of acute cholecystitis.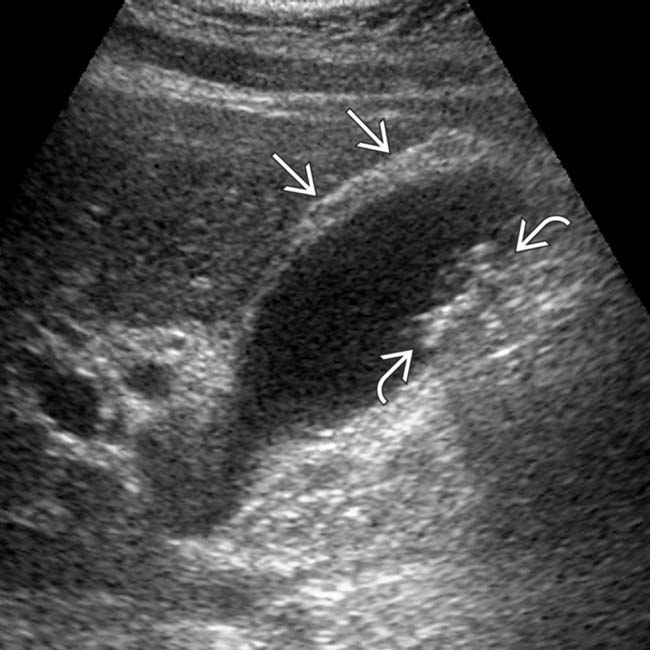
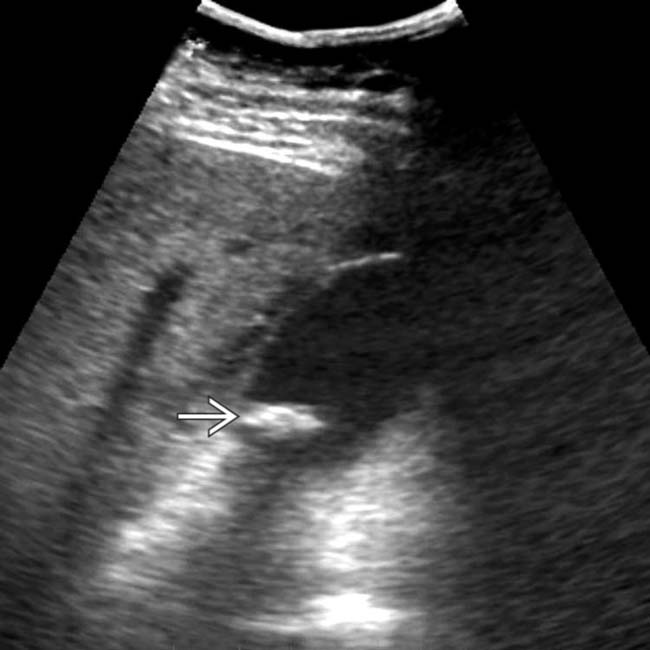
 and multiple small, weakly shadowing stones
and multiple small, weakly shadowing stones  . A sonographic Murphy sign was confidently elicited.
. A sonographic Murphy sign was confidently elicited.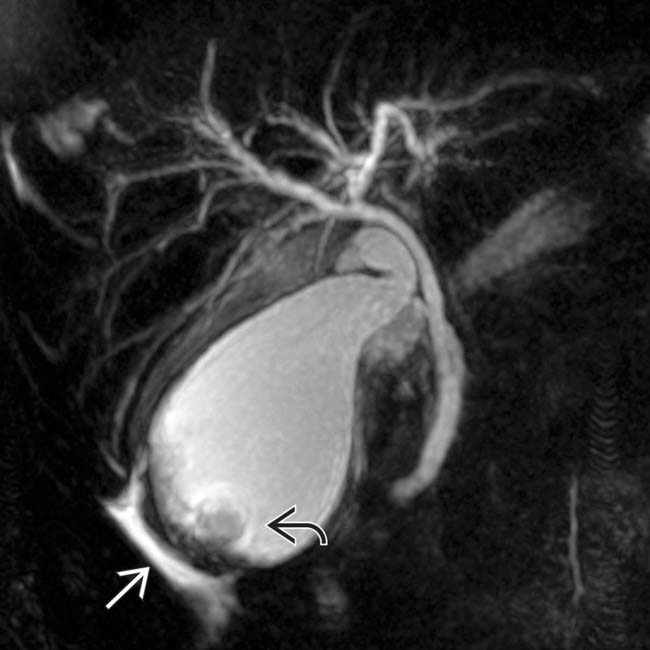
 , and pericholecystic fluid
, and pericholecystic fluid  .
.
 , a small amount of pericholecystic fluid
, a small amount of pericholecystic fluid  , and small gallstones
, and small gallstones  .
.
 and linear membranes in the GB lumen
and linear membranes in the GB lumen  from fibrous strands of pus.
from fibrous strands of pus.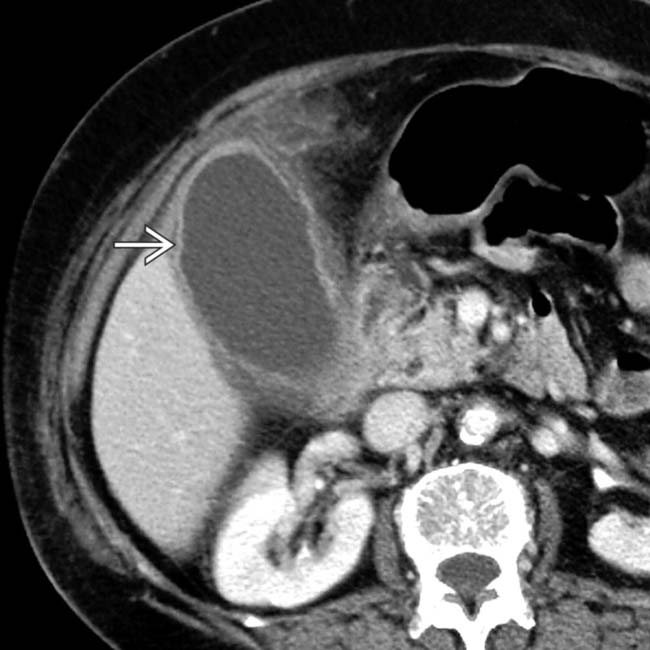
 .
.
 . Note the adjacent inflammatory changes in the omental fat
. Note the adjacent inflammatory changes in the omental fat  .
.
 , but the GB wall was judged to be of normal thickness, and the area above it was not very tender.
, but the GB wall was judged to be of normal thickness, and the area above it was not very tender.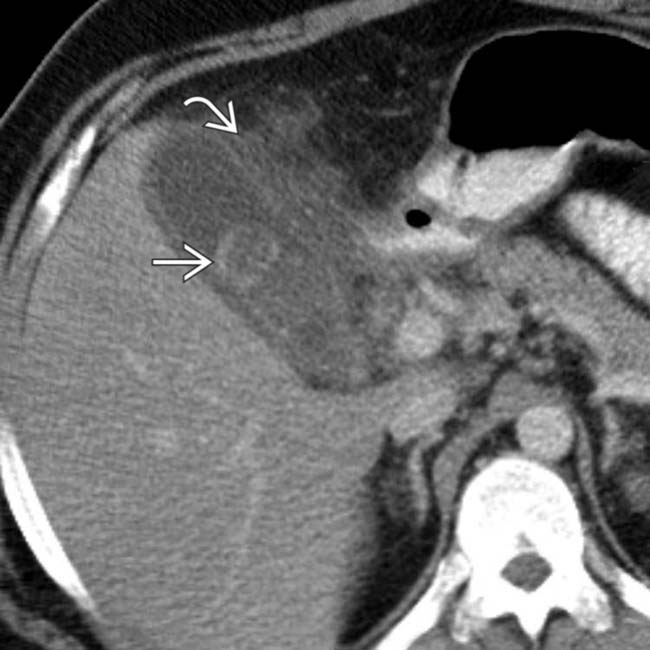
 as well as mural thickening and pericholecystic inflammation
as well as mural thickening and pericholecystic inflammation  . Acute cholecystitis was confirmed at surgery.
. Acute cholecystitis was confirmed at surgery.
 .
.
 of a thickened GB wall.
of a thickened GB wall.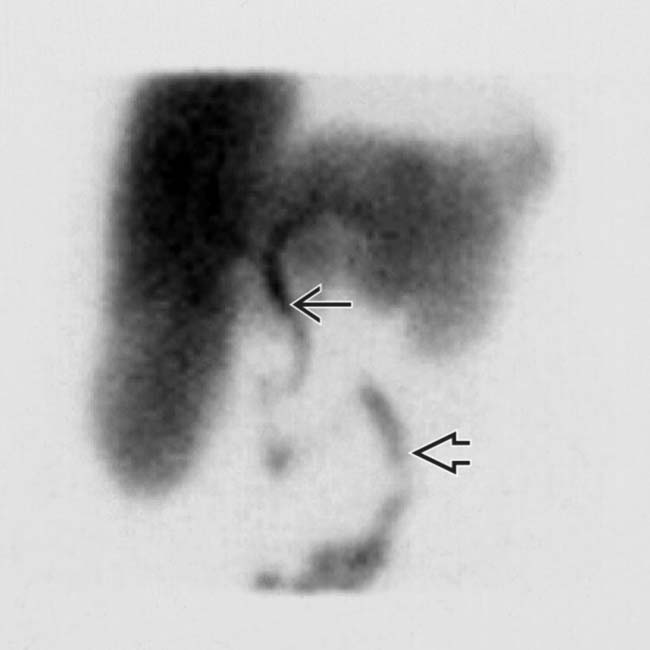
 and the small bowel
and the small bowel  without filling of the GB.
without filling of the GB.






















































































 .
.
 .
.
 .
.

