CHAPTER 13 Acute abdomen
Basic principles
History
Pain
Examination
Vaginal examination
Investigations
Causes
Some causes of the acute abdomen are shown in Table 13.1. These conditions are covered in the relevant chapters. (For information on the site of abdominal pain in relation to suspected pathology → Table 13.2.)
| Gastrointestinal | |
| Gut | Acute appendicitis |
| Intestinal obstruction | |
| Perforated peptic ulcer | |
| Diverticulitis | |
| Inflammatory bowel disease | |
| Acute exacerbation of peptic ulcer | |
| Gastroenteritis | |
| Mesenteric adenitis | |
| Meckel’s diverticulitis | |
| Liver and biliary tract | Cholecystitis |
| Cholangitis | |
| Hepatitis | |
| Biliary colic | |
| Pancreas | Acute pancreatitis |
| Spleen | Splenic infarct and spontaneous rupture |
| Urinary tract | Cystitis |
| Acute pyelonephritis | |
| Ureteric colic | |
| Acute retention | |
| Gynaecological | Ruptured ectopic pregnancy |
| Torsion of ovarian cyst | |
| Ruptured ovarian cyst | |
| Salpingitis | |
| Severe dysmenorrhoea | |
| Mittelschmerz | |
| Endometriosis | |
| Vascular | Ruptured aortic aneurysm |
| Mesenteric embolus | |
| Mesenteric venous thrombosis | |
| Ischaemic colitis | |
| Acute aortic dissection | |
| Peritoneum | Primary peritonitis |
| Secondary peritonitis | |
| Abdominal wall | Rectus sheath haematoma |
| Retroperitoneal | Haemorrhage, e.g. anticoagulants |
TABLE 13.2 Site of abdominal pain in relation to suspected pathology
| Whole abdomen | Generalized peritonitis and mesenteric infarction |
| Right upper quadrant | Acute cholecystitis |
| Cholangitis | |
| Hepatitis | |
| Peptic ulceration | |
| Left upper quadrant | Peptic ulceration |
| Pancreatitis | |
| Splenic infarct | |
| Right lower quadrant | Appendicitis |
| Ovarian cyst | |
| Ectopic pregnancy | |
| Pelvic inflammatory disease | |
| Meckel’s diverticulum | |
| Mesenteric adenitis | |
| Ureteric colic | |
| Rectus sheath haematoma | |
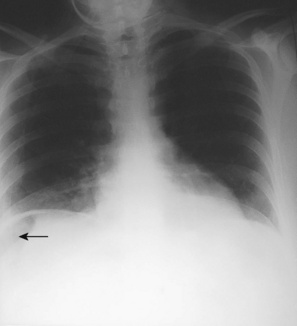
| Right-sided lobar pneumonia | |
| Left lower quadrant | Sigmoid diverticular disease |
| Ovarian cyst | |
| Ectopic pregnancy | |
| Pelvic inflammatory disease | |
| Ureteric colic | |
| Rectus sheath haematoma | |
| Left-sided lobar pneumonia | |
| Radiating pain | Peptic ulcer |
| Back | Pancreatitis |
| Aortic aneurysm | |
| Acute aortic dissection | |
| Groin | Ureteric colic |
| Testicular torsion |
Management
Medical causes of acute abdominal pain
Peritonitis
Peritonitis is an inflammatory or suppurative response of the peritoneal lining to direct irritation. It may be localized or generalized, bacterial or chemical. Localized peritonitis is due to transmural inflammation of a viscus, e.g. appendicitis, cholecystitis, diverticulitis. It may remain localized through being contained by omental wrapping or adhesion of adjacent structures. In many cases, however, it becomes generalized, spreading to involve the whole peritoneum. Sudden perforation of a viscus usually results in generalized peritonitis. With the latter the patient is seriously ill. Hypovolaemia results from massive exudation into the peritoneal cavity, and septicaemia may result if the cause is infective, e.g. faecal peritonitis from perforated diverticulitis. Chemical peritonitis results from gastric or pancreatic juice, bile, urine or blood in the peritoneal cavity. Bile causes little reaction if sterile but causes severe peritonitis if infected or mixed with pancreatic juice. Blood and urine cause little reaction if sterile but a severe reaction occurs if they are infective. (For a classification of peritonitis, → Table 13.3.)
| Acute | |
| Bacterial | Primary (rare): |
Intra-abdominal abscesses
Intraperitoneal abscesses
These tend to arise in dependent areas of the abdomen where fluid may collect. They include:
Extraperitoneal abscesses
Symptoms and signs
Treatment
Laparotomy
Perforated peptic ulcer
The following are steps in the procedure: