Chapter 17 Activities of Daily Living (Basic)
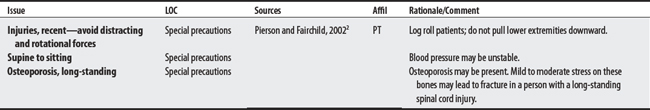
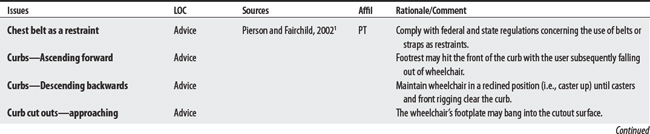
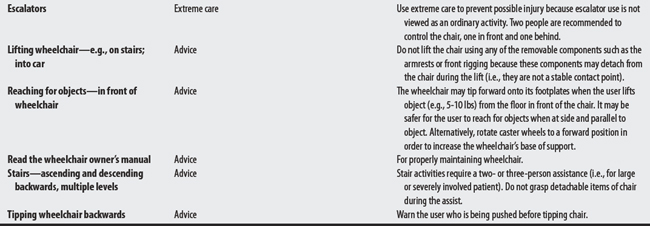
In the following sections, bed activities, transfer, feeding (aspiration), carrying, and lifting concerns will be listed. These concerns are activity (dynamic) related. (For static issues, see Positioning.)
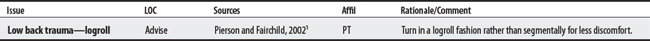
17.1 Bed Activities
CONTRAINDICATIONS AND PRECAUTIONS
L00-L99 DISEASES OF THE SKIN AND SUBCUTANEOUS TISSUE
M00-M99 DISEASES OF THE MUSCULOSKELETAL SYSTEM AND CONNECTIVE
1 Pierson FM, Fairchild SL. Principles and techniques of patient care, ed 3. Philadelphia: W.B. Saunders, 2002.
2 Maihafer GC. Rehabilitation of total hip replacements and fracture management considerations. In: Echternach JL, editor. Physical therapy of the hip. New York: Churchill Livingstone, 1990.
3 AHCPR. Pressure ulcers in adults: prediction and prevention. Clinical Practice Guideline Number 3, AHCPR Pub. No. 92-0047, May 1992.
17.2 Carrying
Carrying is defined as the act of moving something from one place to another place and is applied below within the context of UE activity.1 Upper limb prosthetic concerns and ergonomic issues are listed below.
1 Webster’s third new international dictionary. Springfield (MA): Merriam-Webster, 1981.
2 Kisner C, Colby LA. Therapeutic exercise: foundations and techniques, ed 3. Philadelphia: F.A. Davis, 1996.
3 Pierson FM, Fairchild SL. Principles and techniques of patient care, ed 3. Philadelphia: W.B. Saunders, 2002.
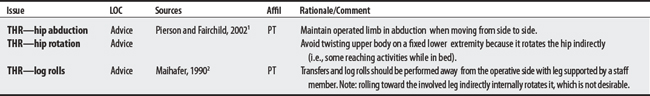
17.3 Feeding/Swallowing Problems (Dysphagia)
OVERVIEW.
Aspiration of vomitus involves the inhalation of regurgitated gastric contents into the pulmonary system.1 It may be unsafe to have patients feed by mouth if they are at high risk for aspiration. Signs of a person with high risk for aspiration include decreased alertness, decreased responsiveness, absent swallow, absent protective cough, difficulty handling secretions (excessive cough, choking), copious secretions, a wet gurgling voice quality, or a decreased movement (range and strength) of oral, pharyngeal, and laryngeal areas.2
PROCEDURAL CONCERNS
Aspiration Precaution for Neurologically Impaired Patients with Dysphagia
Reflux refers to an abnormal return or backward flow of fluids. In gastroesophageal reflux, there is a backflow of contents from the stomach to the esophagus.1 Homer and Massey3 list some reflux precautions for neurologically impaired patients with dysphagia below.
1 Anderson K, Anderson L, Glanze WD. Mosby’s medical, nursing, and allied health dictionary, ed 5. St. Louis: Mosby, 1998.
2 Tan JC. Practical manual of physical medicine and rehabilitation: diagnostics, therapeutics, and basic problems. St. Louis: Mosby, 1998.
3 Horner J, Massey EW. Managing dysphagia: special problems in patients with neurologic disease. Postgrad Med. 1991;89(5):203-213.
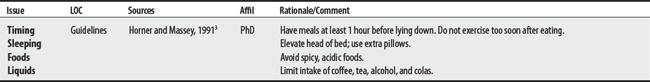
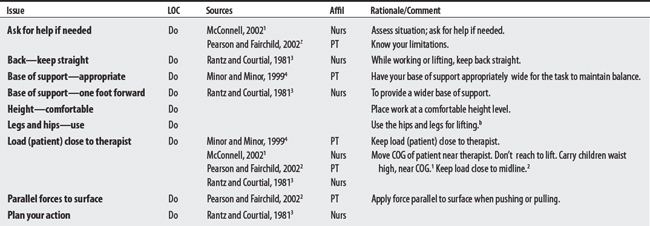
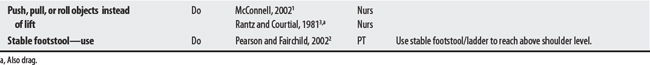
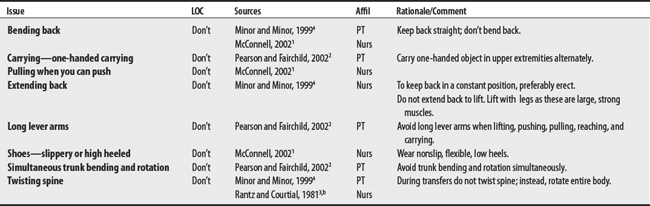
17.4 Moving and Lifting: Body Mechanics (Moving Heavy Items or Patients)
This section lists recommendations on basic body mechanics while lifting and moving loads. Four sources (two physical therapists and two nurses) mentioned 19 do’s and don’ts for moving heavy items (such as patients) that ranged from five to seven per source. The most frequently mentioned recommendation is to keep the load (patient) close to the therapist.
1 McConnell EA. Using proper body mechanics: Clinical do’s and don’ts. Nursing. 2002;32(5):17.
2 Pierson FM, Fairchild SL. Principles and techniques of patient care, ed 3. Philadelphia: W.B. Saunders, 2002.
3 Rantz MR, Courtial D. Lifting, moving, and transferring patients: a manual, ed 2. St. Louis: Mosby, 1981.
4 Minor MAS, Minor SD. Patient care skills, ed 4. Stamford (CT): Appleton & Lange, 1999.
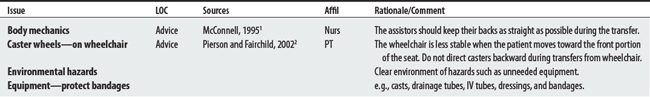
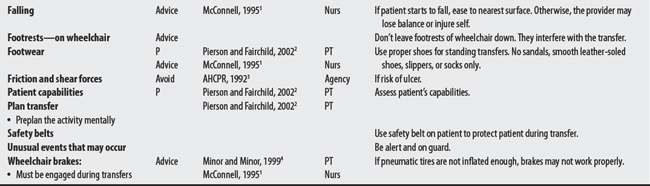
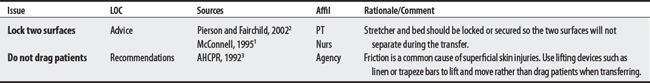
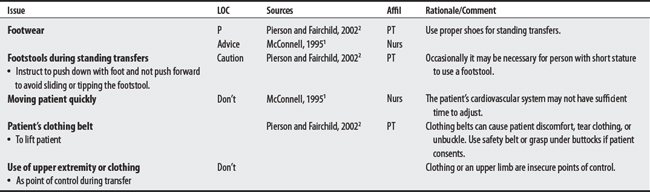
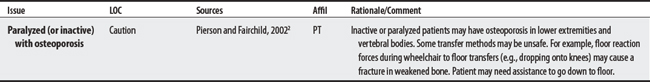
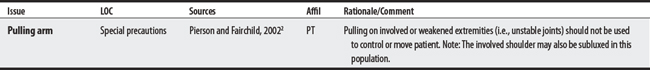
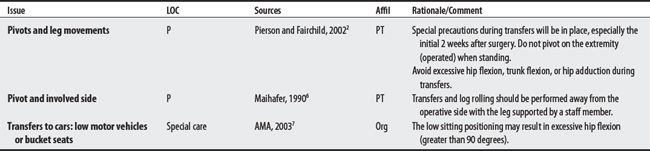
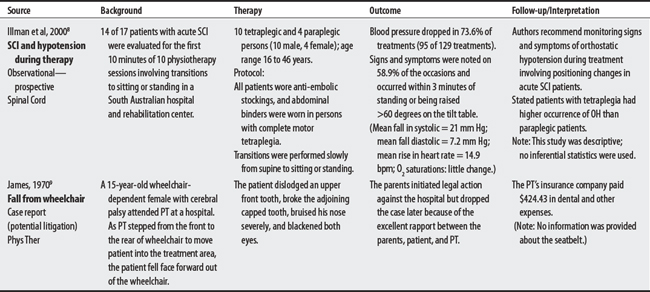
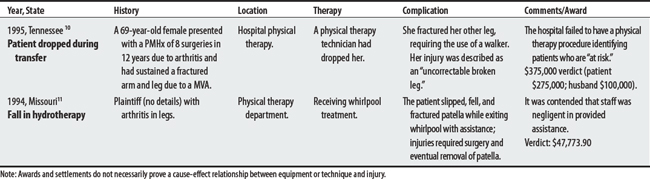
17.5 Transfer Training
Transfer refers to the movement of someone from one surface to another one. The advice below is organized by type (general concerns, stretcher, stand-pivot, sliding board, floor) and by diagnosis (hemiplegia, spinal cord injury, burns). Complications such as falls have occurred during transfers from wheelchairs, plinths, and while in hydrotherapy (see also Mechanical lift).
1 McConnell EA. Transferring a patient from bed to chair. Nursing. 1995;25(11):30.
2 Pierson FM, Fairchild SL. Principles and techniques of patient care, ed 3. Philadelphia: Saunders, 2002.
3 AHCPR: Pressure ulcers in adults: prediction and prevention. Clinical Practice Guideline Number 3, AHCPR Pub. No. 92-0047, May 1992.
4 Minor MAS, Minor SD. Patient care skills, ed 4. Stamford (CT): Appleton & Lange, 1999.
5 Medical Devices Agency. Moving and transferring equipment: a comparative evaluation. DEA A19. London: Medical Devices Agency, 1996.
6 Maihafer GC. Rehabilitation of total hip replacements and fracture management considerations. In: Echternach JL, editor. Physical therapy of the hip. New York: Churchill Livingstone, 1990.
7 American Medical Association. Physician’s guide to assessing and counseling older drivers [2003]. Available at: http://www.ama-assn.org/ama/pub/category/10791.html. Accessed November 7, 2005
8 Illman A, Stiller K, Williams M. The prevalence of orthostatic hypotension during physiotherapy treatment in patients with an acute spinal cord injury. Spinal Cord. 2000;38(12):741-747.
9 James CA. Medico-legal considerations in the practice of physical therapy. Phys Ther. 1970;50(8):1203-1207.
10 Medical malpractice verdict settlement, and experts, June 1995, p 27, loc 1.
11 Medical malpractice verdict settlement, and experts, December 1994, p 45, loc 4.