3. Acromegaly
Definition
Acromegaly is the abnormal enlargement of limbs and facial features as a result of hypersecretion of growth hormone after maturity. The disease is usually the result of a pituitary tumor.
Incidence
The incidence of acromegaly is estimated to be 3:1,000,000 to 4:1,000,000.
Etiology
More than 95% of growth hormone–releasing hormone (GHRH) independent cases of acromegaly are the result of growth hormone (GH)–secreting pituitary adenoma. These adenomas are either macroadenomas (>1 cm) or microadenomas (<1 cm). Macroadenomas predominate, accounting for more than 80% of the tumors.
Signs and Symptoms
• Arthritis
• Bitemporal hemianopia
• Congestive heart failure
• Enlarged thyroid
• Enlarging extremities
• Facial feature coarsening
• Frontal bossing
• Headaches
• Hypercalciuria
• Hyperhidrosis
• Hyperphosphatemia
• Hypertriglyceridemia
• Increased incidence of CHF
• Increased incidence of colonic polyps
• Increased incidence of glucose intolerance
• Increased obstructive apnea
• Increased shoe or ring size
• Macroglossia
• Mild hirsutism (females)
• Multinodular goiter
• Nose thickening
• Prognathism
• Soft tissue swelling
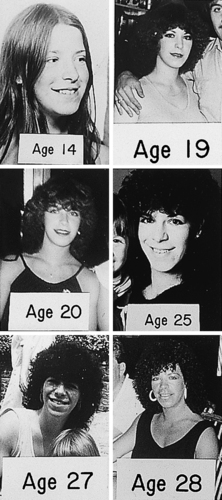 |
| Acromegaly. Chronologic sequence of photographs showing slow development of acromegaly. |
Medical Management
The goal of treatment for acromegaly is symptom alleviation via a multimodal treatment plan. The first line of treatment is surgical removal of the pituitary tumor, which is 80% to 85% successful for microadenomas and 50% to 65% successful for macroadenomas. When complete remission is not achieved by surgical excision of the tumor, somatostatin analogues, dopamine analogues, and growth hormone receptor antagonists dominate subsequent medical management.
Complications
If left untreated, acromegaly produces somatic hypertrophy in all organ systems, including the heart muscle, soft tissue, and kidneys. Articular overgrowth of synovial tissue and hypertrophic arthropathy cause joint and back pain. Soft tissue overgrowth also produces thick skin, hyperhidrosis (malodorous), and carpal tunnel syndrome. Macroglossia can produce obstructive sleep apnea.
Hypertrophic growth of the heart produces hypertension, left ventricular hypertrophy, and acromegalic cardiomyopathy with dysfunction and dysrhythmias.
Anesthesia Implications
Soft tissue thickening may increase the challenge of obtaining intravenous access.
Hypertrophy of the tongue and mandible may interfere with securing an adequate mask fit during induction of anesthesia. Direct visualization of the glottis may also be more difficult. A difficult airway cart with fiberoptic capabilities should be on hand when caring for the patient with acromegaly. Surgical tracheostomy may be required if intubation becomes impossible.
The patient may have mild diabetes mellitus, ventricular hypertrophy, hypertension, degenerative vascular disease, and cardiac disease. Intraoperative monitoring of capillary blood glucose levels with or without insulin coverage may therefore be appropriate.
The patient may be more susceptible to cardiac ischemia.
Venous air embolism is a real concern during transsphenoidal surgery.
Steroid coverage and prophylactic antibiotics should be administered.
Because of the patient’s propensity toward obstructive sleep apnea, short-acting medications, whether inhalational or intravenous, should dominate the anesthetic plan. Sevoflurane, propofol, and remifentanil are all appropriate choices to allow for relatively rapid change in the depth of anesthesia, along with rapid induction and emergence.
Muscle paralysis must be fully reversed to minimize recurization phenomenon and airway obstruction.
Extubation should not occur until the patient has good control of the airway reflexes; however, the anesthetist must take care that the patient not dislodge the nasal packing in place as a result of the transsphenoidal tumor resection.
Throat packing must be removed before extubation. Although this may seem a trivial, common sense matter, this simple step has been overlooked in the past and has been the cause of serious airway emergencies.
Narcotic administration, intraoperatively and postoperatively, must be done with caution because of the potential of sleep apnea.
For the patient with sleep apnea, nasal continuous positive airway pressure (CPAP) will not be an option, particularly if the transsphenoidal approach has been used.







