1. Achalasia
Definition
Achalasia is the failure to relax by the smooth muscle fibers at any junction of one part of the gastrointestinal tract with another, especially failure of the esophagogastric sphincter to relax with swallowing due to degeneration of ganglion cells in the wall of the organ.
Incidence
The incidence of achalasia is approximately 1:10,000. Patients with achalasia usually range in age from 25 to 60 years, but it may also be seen in teenagers. It is a chronic problem that worsens over time.
Etiology
The cause of achalasia is not known; the underlying problem may have a neural origin with the involvement of Auerbach’s (myenteric) plexus. There are some histologic and physiologic alterations in the vagus nerve have been described in connection with the disorder.
Signs and Symptoms
• Chest pain
• Difficulty swallowing
• Heartburn
• Hiccups
• “Lump” in the throat
• Regurgitation of swallowed food, both solid and liquid
• Sense of fullness
• Weight loss
Medical Management
Achalasia is suspected based on the presence of symptoms. The following tests are performed to confirm the diagnosis: chest x-ray, barium swallow, endoscopy, and manometry.
Pharmacologic treatment is directed toward decreasing lower esophageal pressure. A calcium channel blocker or a nitrate is used most commonly to achieve this goal. The calcium channel blocker currently employed most often is nifedipine, while isosorbide dinitrate is the nitrate currently utilized. These medications are taken sublingually 10 to 30 minutes before meals and on an as-needed basis before bedtime if reflux is an issue during the overnight hours.
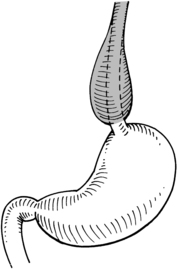 |
| Achalasia. Decreased muscle tone and peristaltic function prevent food from entering the stomach, causing esophageal distention. |
Botulinum toxin (Botox) is occasionally directly injected into the esophageal sphincter during endoscopy to restore the balance between excitatory and inhibitory neurotransmissions. Botox treatment is of limited value and duration. Treatment must be repeated in approximately 70% of patients that have been injected with Botox. Botox treatment can cause an inflammatory response in the sphincter.
The stricture can be mechanically dilated with a pneumatic (balloon) catheter. The catheter is threaded through the stricture so that the sphincter is situated at the midportion of the balloon, which is then gradually inflated to a predetermined pressure. The balloon remains inflated for a period of time after which it is deflated and the catheter withdrawn. Pneumatic dilation is successful in 70% to 80% of those treated in this manner.
Complications
• Injection of Botox can result in anaphylaxis.
• Pneumatic dilation results in esophageal perforation in approximately 5% of patients receiving this treatment. In the event of esophageal rupture or perforation, this patient is an emergent surgical candidate.
Anesthesia Implications
Whether treated or untreated, the patient with achalasia should receive a rapid sequence induction—a true rapid sequence induction for general anesthesia consisting of thorough preoxygenation prior to medication administration, reverse Trendelenburg’s position, and respiratory “silence” after medication administration. Direct laryngoscopy and tracheal intubation should occur as quickly as possible. The patient is not a “full stomach” risk; rather, the patient should be considered a “full esophagus.” “Silent” aspiration is a very real possibility in patients with achalasia.
The patient with achalasia may have had episodes of pneumonitis in the past as the result of “silent” aspiration during sleep. NPO status is not a guarantee that aspiration will not occur. Antacid treatment with citric acid/sodium citrate may not offer any advantage since it, too, may be stationary near the gastroesophageal junction rather than passing through the stomach.
Postoperatively the patient should be transported with oxygen by simple mask to the post-anesthesia care unit (PACU) with the head of the bed elevated ≥30 degrees to reduce the potential for reflux and aspiration of esophageal contents.






