Chapter 619 Abnormalities of the Cornea
Neonatal Corneal Opacities
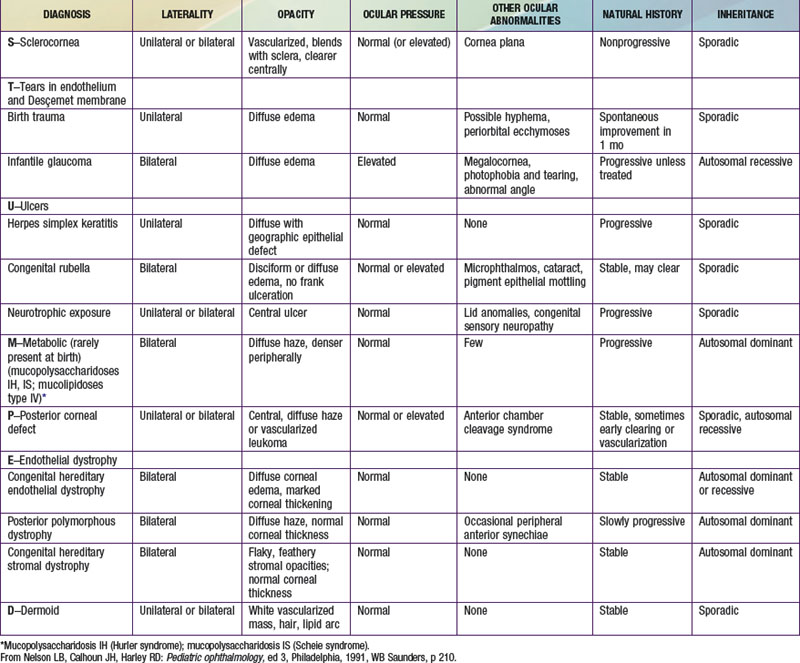
Loss of the normal transparency of the cornea in neonates may occur secondary to either intrinsic hereditary or extrinsic environmental causes (Table 619-1).
Peters Anomaly
Peters anomaly is a central corneal opacity (leukoma) that is present at birth (Fig. 619-1). It is often associated with iridocorneal adhesions that extend from the iris collarette to the border of the corneal opacity. Approximately half of patients have other ocular abnormalities, which may include cataracts, glaucoma, and microcornea. As many as 80% of cases may be bilateral, and 60% are associated with systemic malformations that may affect any major organ system. Some investigators have divided Peters anomaly into 2 types: a mesodermal or neuroectodermal form (type I), which shows no associated lens changes, and a surface ectodermal form (type II), which does. Histologic findings include a focal absence of Desçemet membrane and corneal endothelium in the region of the opacity. Peters anomaly may be caused by incomplete migration and differentiation of the precursor cells of the central corneal endothelium and Desçemet membrane or a defective separation between the primitive lens and cornea during embryogenesis.
Corneal Manifestations of Systemic Disease
Several metabolic diseases produce distinctive corneal changes in childhood. Refractile polychromatic crystals are deposited throughout the cornea in cystinosis (Chapter 79.4). Corneal deposits producing various degrees of corneal haze also occur in certain types of mucopolysaccharidosis (MPS; Chapter 82), particularly MPS IH (Hurler), MPS IS (Scheie), MPS I H/S (Hurler-Scheie compound), MPS IV (Morquio), MPS VI (Maroteaux-Lamy), and sometimes MPS VII (Sly). Corneal deposits may develop in patients with GM1 (generalized) gangliosidosis (Chapter 80.4). In Fabry disease, fine opacities radiating in a whorl or fanlike pattern occur, and corneal changes can be important in identifying the carrier state (Chapter 80.4). A spraylike pattern of corneal opacities may also be seen in the Bloch-Sulzberger syndrome. In Wilson disease, the distinctive corneal sign is the Kayser-Fleischer ring, a golden brown ring in the peripheral cornea resulting from changes in Desçemet membrane (Chapter 349.2). Pigmented corneal rings may develop in neonates with cholestatic liver disease. Corneal changes may occur in autoimmune hypoparathyroidism and band keratopathy in patients with hypercalcemia. Transient keratitis may occur with rubeola and sometimes with rubella.
Beauchamp GR, Gillette TE, Friendly DS. Phlyctenular keratoconjunctivitis. J Pediatr Ophthalmol Strabismus. 1981;18:22-28.
Chang DC, Grant GB, O’Donnell K, et al. Multistate outbreak of Fusarium keratitis associated with use of a contact lens solution. JAMA. 2006;296:953-963.
Comer RM, Daya SM, O’Keefe M. Penetrating keratoplasty in infants. J AAPOS. 2001;5:285-290.
Dana MR, Moyes AL, Gomes JA, et al. The indications for and outcome in pediatric keratoplasty. A multicenter study. Ophthalmology. 1995;102:1129-1138.
Garg P, Krishna PV, Stratis AK, et al. The value of corneal transplantation in reducing blindness. Eye (Lond). 2005;19:1106-1114.
Mackey DA, Buttery RG, Wise GM, et al. Description of X-linked megalocornea with identification of the gene locus. Arch Ophthalmol. 1991;109:829-833.
Michaeli A, Markovich A, Rootman DS. Corneal transplants for the treatment of congenital corneal opacities. J Pediatr Ophthalmol Strabismus. 2005;42:34-44.
Mohandessan MM, Romano PE. Neuroparalytic keratitis in Goldenhar-Gorlin syndrome. Am J Ophthalmol. 1978;85:111-113.
Reidy JJ. Congenital corneal opacities. Ophthalmol Clin North Am. 1996;2:199-213.
Traboulsi EI, Maumenee IH. Peters’ anomaly and associated congenital malformations. Arch Ophthalmol. 1992;110:1739-1742.
Yang LL, Lambert SR, Fernhoff PM, et al. Peters’ anomaly: associated congenital malformations and etiology. Invest Ophthalmol Vis Sci. 1995;36:S41.
Yang LL, Lambert SR, Lynn MJ, et al. Long-term results of corneal graft survival in infants and children with Peters anomaly. Ophthalmology. 1999;106:833-848.