Abnormal Movements
BACKGROUND
Abnormal movements are best appreciated by seeing affected patients. If you are armed with the right vocabulary, most common abnormal movements can be described. However, many experts will describe the same movements in different ways—so journals about movement disorders come with video clips to illustrate the movements!
In most patients with movement disorder, the diagnosis depends on an accurate description of the clinical phenomenon.
There is frequently a considerable overlap between syndromes, and several types of abnormal movement are often seen in the same patient—for example, tremor and dystonia in a parkinsonian patient on treatment.
The anatomy of the basal ganglia is complicated and wiring diagrams illustrating the connections between the various structures become more complicated as more research is done. Neuro-anatomical correlations are of limited clinical value as most movement disorders are classified as syndromes rather than on anatomical grounds. Correlations of significance include unilateral parkinsonism due to lesions of contralateral substantia nigra and unilateral hemiballismus due to lesions of the contralateral subthalamic nucleus or its connections.
In evaluating movement disorders, there are three aspects to the examination:
– the abnormal positions maintained
– the additional movements seen.
– the inability to do things: for example, a slowness in initiating actions (bradykinesia).
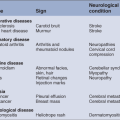
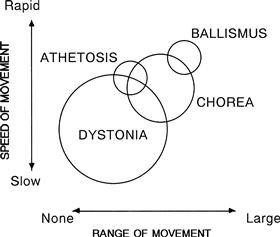
Terms used in movement disorders (Fig. 24.1)
WHAT TO DO
Look at the patient’s face.
Look at the patient’s head position.
Look at the arms and the legs.
Ask the patient to:
• smile
• hold his hands out in front of him with his wrists cocked back (Fig. 24.2A)
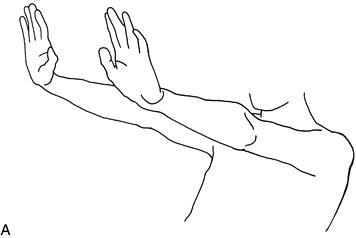
Figure 24.2A Testing for tremor
• lift his elbows out sideways and point his index fingers at one another in front of his nose (Fig. 24.2B)
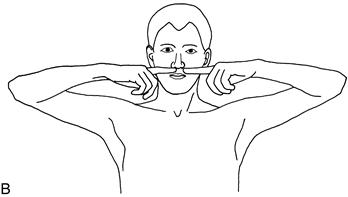
Figure 24.2B Testing for tremor
If there is a tremor, note the frequency, the degree of the excursion (fine, moderate, large) and the body parts affected. Look for a tongue tremor (see Chapter 13).
Test eye movements (Chapter 9).
Test tone (Chapter 16).
Test fast repeating movements.
– bring thumb and index finger rapidly together (demonstrate)
– touch the thumb with each finger rapidly in turn (demonstrate)
– tap his toe as if listening to fast music.
Observe the speed of the movements and whether they break up; compare right with left.
Test gait (Chapter 4).
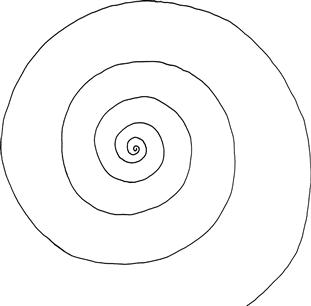
Test writing.
WHAT YOU FIND
Face
Positive phenomena
Commonly:
• Lip-smacking and twisting of mouth: orofacial dyskinesia.
• Flickering of muscles, particularly around eye: facial myokymia.
Rarely:
Head
Positive phenomena
Position
Arms and legs
Positive phenomena
Tremor
• Present when limb (particularly hand) is at rest: rest tremor.
• Present when limb is maintained in a position (especially as in Fig. 24.2): postural tremor.
• Present during an action (e.g. finger–nose testing): action tremor.
• Present and increasing as the finger reaches its target: intention tremor.
Asterixis
• Irregular jerky movements of the hands, seen especially in the position illustrated in Figure 24.2. This is actually a sudden loss of tone—negative myoclonus.
Position
Additional movements (as described above). Describe which part of the movements are seen to be affected:
Latent phenomena
On walking, the following may occur or increase:
Finger–nose testing may reveal:
and exacerbate:
Writing
WHAT IT MEANS
Akinetic–rigid syndromes (parkinsonism) (common)
• Key features: rigidity, bradykinesia and tremor. Features include reduced facial expression (mask-like), rest tremor, stooped posture with reduced arm-swing and increased tremor on walking. Gait may be festinant (see Chapter 4). Bradykinesia on fast repeating movements and walking. Extrapyramidal dysarthria (see Chapter 2). There may be limitation of convergence.
Tremors (common)
Chorea (uncommon)
Common cause:
Rare causes:
Hemiballismus (rare)
Dystonia (uncommon)
Affects only one part of the body during a particular action: task-specific dystonia
Affects only one part of the body: focal dystonia
Affecting two or more adjacent parts of the body: segmental dystonia. For example:
Affects parts of the body that are not adjacent:
Common causes:
Rare cause: dystonia musculorum deformans.
Tic (uncommon)
Usually an isolated finding which may be associated with coprolalia (muttering of obscenities); then referred to as Gilles de la Tourette syndrome.
Myoclonic jerk (rare)
May be seen as part of other movement disorders where chorea or dystonia is predominant.
Associated with a number of metabolic encephalopathies, myoclonic epilepsies—seen in rare neurological diseases such as Creutzfeldt–Jakob disease and postanoxic encephalopathy.

 TIP
TIP TIP
TIP