CHAPTER 10 Abductor Tears
Tendinopathy and tears of the gluteus medius and minimus tendons are a common cause of recalcitrant pain along the lateral side of the hip. Tears of the gluteus medius and minimus tendon were first described by Bunker and Kagan and colleagues in the late 1990s.1,2 Bunker and associates1 reported a 22% incidence of concomitant medius tears in 50 patients treated for femoral neck fractures. The tears were most commonly seen distally at the junction of the gluteus medius and minimus. Howell and coworkers3 reported that 22% of women and 16% of men who underwent total hip arthroplasty for osteoarthritis (N = 176) had abductor tears. The incidence was greater with increased age in both groups.
Abductor tears should certainly be suspected in patients with intractable GTPS in whom conservative management has failed. The pain can be variable, but is characteristically exacerbated by weight-bearing and resisted hip abduction. Bird and colleagues4 used MRI to evaluate the integrity of the gluteus medius in 24 women with recalcitrant GTPS. A tear of the medius tendon insertion was found in 46% of patients, and an additional 38% had gluteus medius tendonitis without an appreciable tear. Kagan and associates2 performed an open medius tendon repair in 7 patients with recalcitrant GTPS and magnetic resonance imaging (MRI) evidence of a tear. In all cases, the tear was located anteriorly in the lateral facet portion of the insertion. Repairs were performed using bone tunnels and anchors. At a median follow-up of 45 months, all patients were pain-free and all but one returned to previous levels of activity.
Although the causes of these tears are likely multifactorial, gluteus medius and minimus tears likely reflect a progressive degenerative process. A precipitating traumatic event is possible but uncommon. Most patients describe an insidious but often debilitating lateral-sided hip pain. The abductors have been likened to the rotator cuff of the hip, with the medius and minimus tendon analogous to the supraspinatus and subscapularis muscles. The medius tendon inserts on the lateral and posterosuperior facets, resulting in a moment arm similar in direction and force to the supraspinatus. The minimus inserts on the anterior facet and, depending on the position of the femur, can exert several different moments, including flexion, abduction, and internal and external rotation. Based on these observations, it follows that one of the primary functions of the minimus is to act as a head stabilizer. However, in many functional flexion angles, it provides a primary internal rotation force similar to that of the subscapularis.5 Similar to the rotator cuff, tears of the medius are significantly more common than those of the minimus. It has been estimated that almost 25% of middle-aged women and 10% of middle-aged men will develop a tear of the gluteus medius tendon.3,6 Tears are four times more common in women than in men.
Tear progression appears to occur by degeneration of the undersurface propagating posteriorly into a full-thickness tear.3,6 Most tears occur in the anterior portion of the tendon as it attaches into the lateral facet of the greater trochanter. These frequently start as partial-thickness undersurface tears that propagate into full-thickness lesions that can extend posteriorly.
Both open and arthroscopic techniques of repair can provide excellent symptomatic relief and restore abductor function. Arthroscopic techniques provide a less invasive alternative and can be readily performed. Regardless of the technique, however, determining the anatomic gluteus medius footprint is critical and can often be difficult. Unlike the supraspinatus tendon, no articular margin is present to be used as a reference landmark.6
ANATOMY
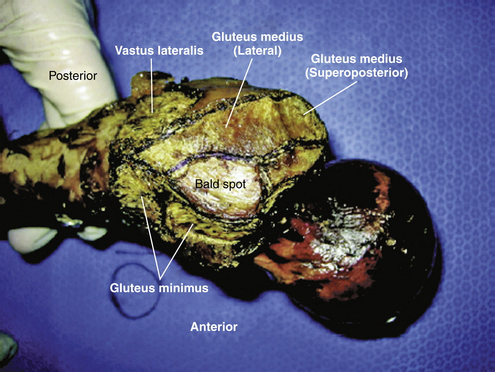
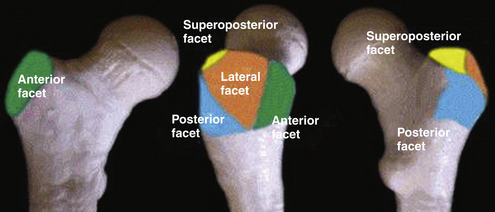
The gluteus medius tendon has two separate entheses on the greater trochanter. The posterior fibers attach to the posterosuperior facet (PSF), whereas the central and anterior fibers insert on the lateral facet (LF) of the trochanter. The facets are oriented at different planes relative to one another (Figs. 10-1 and 10-2).7 The tendinous portion inserting into the PSF is robust, with a circular insertion site of approximate radius of 8.5 mm. The surface area of this insertion is approximately 200 mm2. The lateral facet insertion is more rectangular in shape, with a surface area approximating 440 mm2.
The trochanteric insertion of the gluteus minimus is separated from the proximal portion of the LF footprint by the trochanteric bald spot. Near the midsubstance of the LF footprint, the bald spot ends and the long head of the minimus begins. At this location, the medius footprint abuts and covers a portion of the gluteus minimus.7 The trochanteric bald spot is circular in shape, with a radius of approximately 11 mm. Although it combines with the gluteus medius to comprise the entire lateral facet of the greater trochanter (see Fig. 10-1 and 2), it is critical not to overestimate the size of tendon detachment with an abductor tear by mistakenly incorporating the normal bald spot into the anatomic footprint of the medius tendon.6
The anatomically distinct insertions of the medius are thought to correlate with anatomically distinct portions that function in a phasic manner during the gait cycle. The posterior portion that inserts into the PSF is thought to stabilize the femoral head in the acetabulum during heel strike. The central portion, inserting into the PSF and LF junction, runs more vertically and is thought to be critical in initiating hip abduction. The anterior portion aids in abduction but also functions as an external rotator of the pelvis during swing-through on the contralateral limb.7
CLASSIFICATION
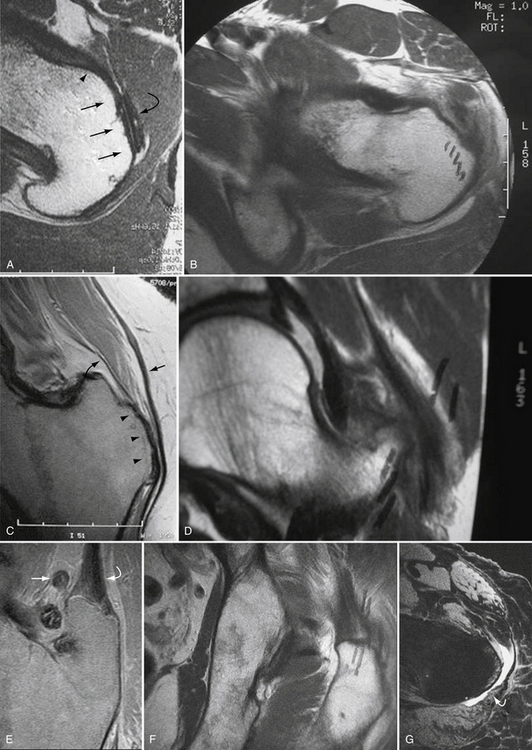
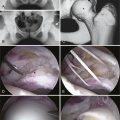
Dwek and associates8 and others9–14 have described a standardized MRI approach to abductor tear classification. They have divided the greater trochanter into four facets—posterosuperior, lateral, anterior, and posterior (Fig. 10-3; see Fig. 10-2). The minimus attaches to the anterior facet (see Fig. 10-3A and B). Figure 10-3A shows the normal attachment of the minimus and Figure 10-3B shows the corresponding image demonstrating a gluteus minimus tear. The medius inserts on the lateral and posterosuperior facets (see Figs. 10-3C-F). Figures 10-3C and E show the normal insertional anatomy of the medius on the LF and PSF whereas Figures 10-3D and F show corresponding images demonstrating medius tendon tears at the respective facets. The posterior facet is covered by the trochanteric bursa (see Fig. 10-3G).
SURGICAL TECHNIQUE
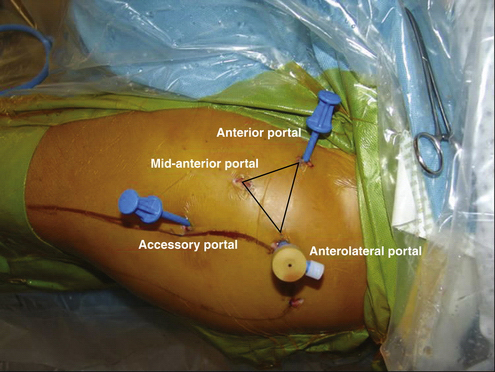
As with any arthroscopic procedure, portal placement is critical. The technique begins with accurate identification of the trochanter and anterior superior iliac spine. The anterior or midanterior portals can afford access into the peritrochanteric space. The anterior portal is placed 1 cm lateral to the anterosuperior iliac spine (ASIS) in the interval between the tensor fascia lata (TFL) and sartorius (Fig. 10-4). We prefer, however, to use a midanterior portal rather than a direct anterior portal. This is typically located 2 to 3 cm distal and 2 to 3 cm lateral to a standard anterior portal, and can be located by creating an equilateral triangle between the anterior and lateral portals.6 It lies directly anterior to the lateral prominence of the greater trochanter and provides the safest access to the joint by avoiding any potential injury to the more proximal gluteus medius musculature and the more distal vastus lateralis musculature. It also offers an improved angle of approach to the peritrochanteric space and minimizes risk of injury to the lateral femoral cutaneous nerve compared with a direct anterior portal. Care should be taken to avoid placing the midanterior portal too proximally or distally. A proximally misplaced portal will injure the gluteus medius belly, whereas a distally misplaced portal will injure the vastus lateralis. The use of fluoroscopic imaging can confirm placement of the portal directly over the lateral prominence of the greater trochanter and prevent inadvertent proximal or distal muscular injury.
The cannula is directed into the peritrochanteric space in an anterior to posterior direction, with the leg in full extension, held in 0 degrees of adduction, 10 degrees of flexion, and 15 degrees of internal rotation (see Fig. 10–4).6 Traction is released prior to entry into the lateral space to relax tension on the iliotibial band. Slight abduction may also be necessary to increase the space between the iliotibial band and greater trochanter. A gentle axial load may be applied if it is difficult to distinguish the muscular fibers of the gluteus medius from the overlying bursal tissue. The cannula is swept back and forth between the iliotibial band and trochanteric bursa, using a technique similar to that used for access into the subacromial space of the shoulder. The iliotibial band is analogous to the coracoacromial ligament of the shoulder.
When the appropriate plane is identified, a clear space between the iliotibial band and greater trochanter can be easily identified (Fig. 10-5A). Typically, bursal tissue is present in the space and can be easily cleared with a motorized shaver to define the lateral (iliotibial band) and medial (greater trochanter and vastus lateralis) borders of the space more clearly (see Fig. 10-5B). With the camera focus directed distally, a distal anterolateral accessory (DALA) portal in the peritrochanteric space is established with spinal needle guidance approximately 4 to 5 cm distally and in line with the anterolateral portal. This portal allows for further distal access for diagnostic and operative intervention and provides outflow (see Fig. 10-4).6 A standard anterolateral portal can also be useful as a third working or viewing portal placed just proximally to the anterolateral tip of the greater trochanter. This portal can improve distal visualization and facilitate suture management with abductor repair.
Diagnostic arthroscopy is initiated with the 70-degree arthroscope in the midanterior portal. The first structure visualized is the gluteus maximus inserting on the femur just below the vastus lateralis. This is a reproducible landmark and no exploration should be performed posterior to the tendon, because the sciatic nerve lies within close proximity (2 to 4 cm) to this location. Inspection then proceeds in a counterclockwise direction, starting distally and posterior at the gluteus maximus insertion and then proceeding proximally and anterior toward the vastus lateralis and gluteus minimus (Fig. 10-6).6
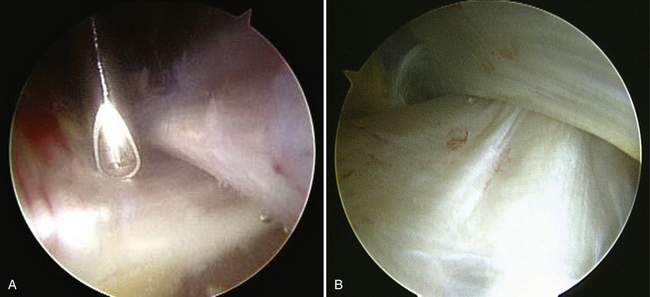
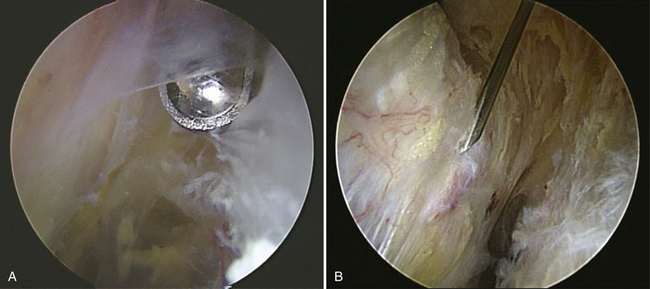
FIGURE 10-6 The initial view identifies the so-called sickle band, or insertion of the gluteus maximus running posterior to the vastus lateralis toward the iliotibial band and posterior femur. A, Viewed from the anterolateral portal looking distal, the maximus tendon insertion can be cleared of tissue and serves as a distal landmark. It is typically unnecessary to extend any surgical dissection distal to this tendon insertion. B, When viewed from the distal anterolateral accessory portal, the tendon insertion can be closely inspected. The sciatic nerve lies approximately 3 to 4 cm posterior to the maximus insertion. Instruments should not be placed posterior to the maximus insertion without direct visualization to make sure that the nerve is protected.
As the arthroscope is moved proximally, the longitudinal fibers of the vastus lateralis are identified and traced up to the vastus tubercle, looking immediately anterior to the lateral facet (Fig. 10-7).6 The gluteus medius tendon and muscle are best visualized at the lateral facet with the arthroscope in the proximal anterolateral portal, with the light source rotated to visualize anteriorly and superiorly (Fig. 10-8A). Visualization of the gluteus minimus can be difficult because it is usually covered by muscle tissue of the gluteus medius. By gently sweeping away medius muscle, the tendinous insertion of the minimus onto the anterior facet can be visualized (see Fig. 10-8B). Fibrous bands in this area will require excision. Hemostasis can be obtained with radiofrequency ablation or standard cautery. The fibers of the medius lie posterior to the minimus and should be carefully probed to inspect for a tear (see Fig. 10-8C). Finally, the arthroscope should be directed toward the iliotibial band. The posterior third of the iliotibial band may demonstrate abrasive changes if a symptomatic coxa saltans externus is present. An arthroscopic release can be performed if necessary (Fig. 10-9).15 The working instruments can be placed in the midanterior and distal anterolateral accessory portals if an abductor repair or iliotibial band release is necessary.
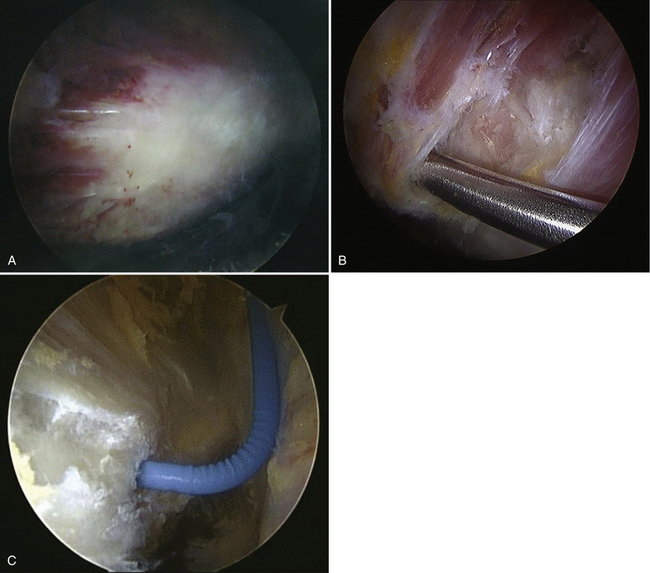
FIGURE 10-8 A, As the camera continues proximally, the gluteus medius insertion onto the lateral facet can be identified. The muscular fibers of the medius can be seen proximal to the tendon. B, To visualize the minimus tendon insertion onto the anterior facet, the gluteus medius muscle has to be elevated, because the tendon insertion is covered by the medius. C, When evaluating the tendon insertion, the entire lateral and anterior facets should be carefully probed. A partial tear typically occurs as an undersurface injury and may be difficult to visualize directly. Correlation with the MRI scan is important during this inspection process.
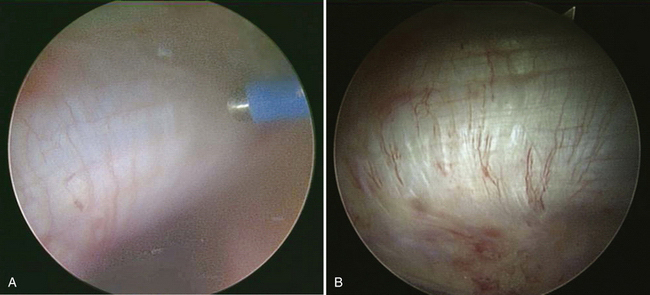
The technique for repairing a full-thickness tear of the abductor tendons is similar to that described for the rotator cuff. A thorough débridement of the trochanteric bursa is performed first to decompress the compartment and improve visualization (Fig. 10-10). The edges of the tear should be débrided, and clear margins around the tear should be demarcated (see Figs. 10-10C and D). Tears can be acute or chronic, and an assessment of reparability should be performed in an analogous fashion to that for rotator cuff tears by assessing the mobility of the torn edge and quality of the tissue (see Figs. 10-10E and F).
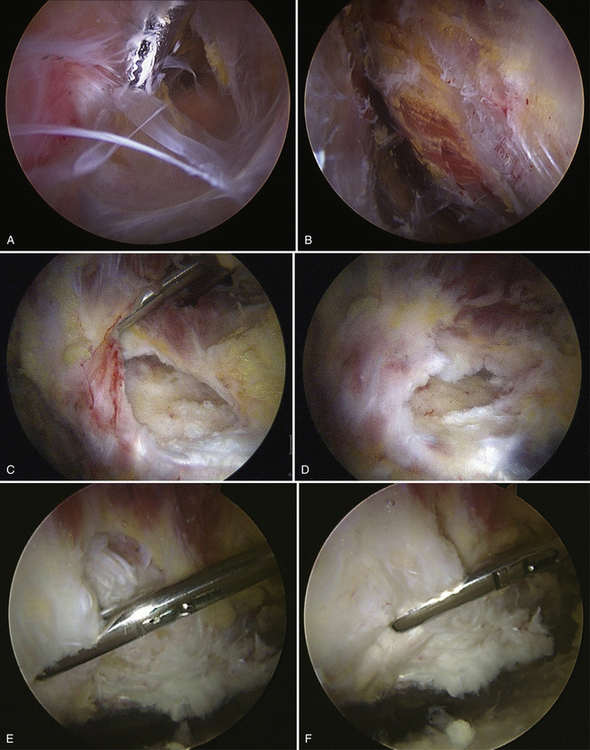
FIGURE 10-10 A, Thickened bursa is excised with the assistance of a motorized shaver to visualize and inspect the medius insertion fully. B, The gluteus medius muscle and tendon should be cleared of bursae. C, D, A full-thickness tear with retraction of the medius tendon is appreciated. E, F, The tear edges need to be demarcated clearly and the mobility of the tendon edge is tested.
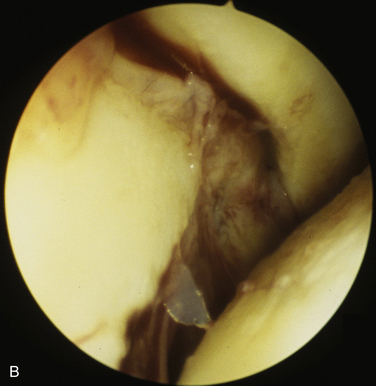
If the tear is repairable, the edges should be clearly identified and débrided to healthy viable tissue (Fig. 10-11A). Similarly, the anatomic footprint on the lateral facet should be cleared of soft tissue debris and decorticated to bleeding cancellous bone with a burr (see Figs. 10-11B and C). Suture anchors are then placed into the footprint using standard arthroscopic technique, typically through a small stab incision. A spinal needle or curved snap can be used to determine the ideal location and trajectory for anchor insertion, and confirmed with fluoroscopy (Fig. 10-12A). Placement of the anchor should be done under direct arthroscopic visualization (see Fig. 10-12B) and checked using fluoroscopy (see Fig. 10-12 C) to confirm an appropriate angle and location of insertion. Typically, two anchors will be sufficient to repair the anatomic footprint of a single tendon tear involving medius tears off the lateral facet. Adequate spacing of the anchors should allow for good bone stock between anchors (Fig. 10-13A and B). Metallic anchors are frequently used because the bone quality of the trochanter is often good, and their position can be confirmed with fluoroscopy.
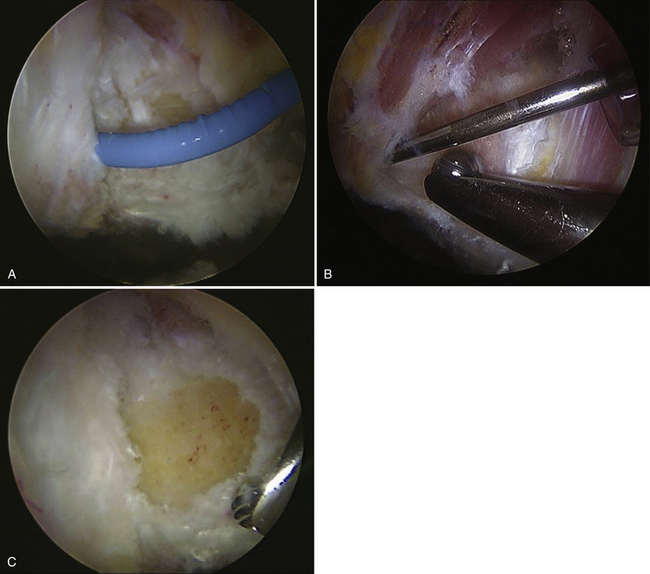
FIGURE 10-11 A, B, The tear footprint is visualized and prepared for arthroscopic repair by débridement of residual tissue using a motorized shaver and electrocautery. C, The bed is then débrided to bleeding cancellous bone in preparation for anchor insertion.
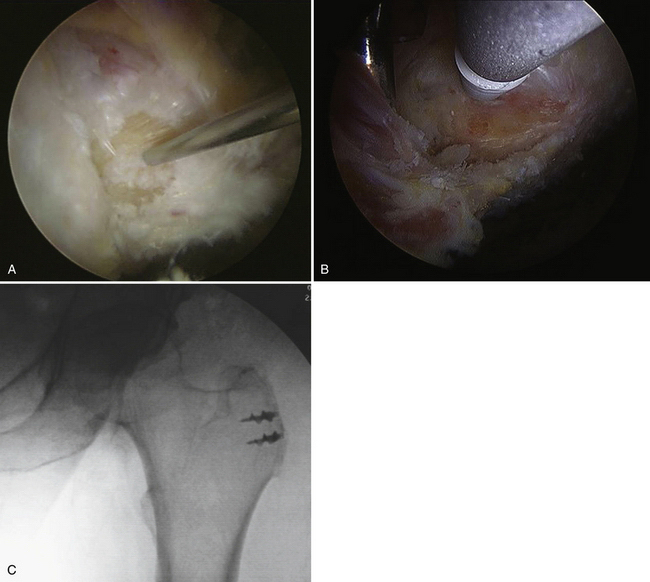
FIGURE 10-12 A, The ideal trajectory for anchor insertion is determined using percutaneous insertion of a spinal needle. B, The anchor is then placed through a small stab incision with this trajectory without difficulty. C, Anchor position along the facet can be confirmed with intraoperative fluoroscopy.
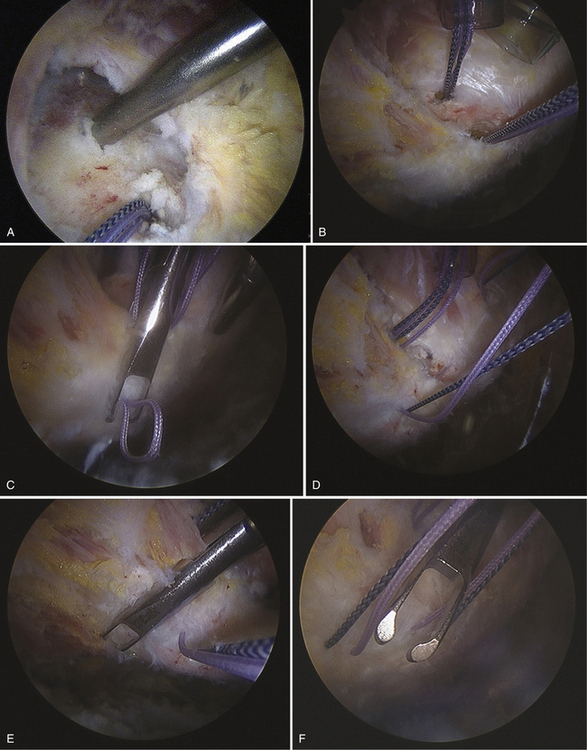
FIGURE 10-13 A, Two anchors have been placed in the lateral facet, each loaded with two sutures. B, Suture management is critical once the anchors are placed. All suture management and tying should be performed through cannulas to avoid tissue incarceration within the suture. C-G, After the free edge of the tear is mobilized, a suture-passing device is used to grasp the retracted tendon edge. Simple or mattress sutures can be placed, depending on the tear configuration.
Once the sutures have been passed and separated, sequential tying is performed using standard arthroscopic knot-tying technique (Fig. 10-14). Careful and complete evaluation of the tendon repair should be performed to confirm anatomic restoration of the tendon footprint and security of the repair.
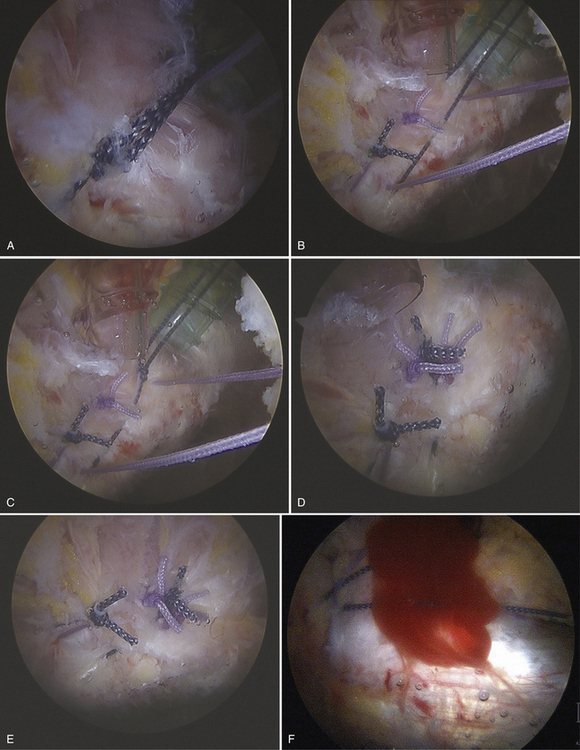
FIGURE 10-14 A-F, After sutures have been passed, arthroscopic knots are tied to repair the tendon to its footprint anatomically. Platelet-rich plasma can be delivered to the tendon-bone interface prior to knot tying for biologic augmentation of healing. The repair is probed to confirm excellent reduction and security.
Undersurface partial-thickness tears in the anterior medius tendon should be carefully assessed. If they are high-grade lesions, they may be converted into full-thickness tears with a full-radius shaver and repaired using the technique described earlier. Transtendon repairs may be performed in the setting of high-grade partial tears to avoid completion of the tear. Anchor placement and suture passage may be more difficult because visualization is impaired by the intact tendon.
PEARLS& PITFALLS
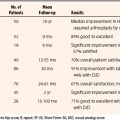
OUTCOMES
Voos and colleagues20 have recently reviewed the short-term clinical outcomes of endoscopic gluteus medius tendon tear repairs performed by the senior author (BTK). Of 482 consecutive hip arthroscopies, 10 patients with medius tendon tears had endoscopic repair, with an average follow-up of 25 months. The patients’ mean age was 50 years and all experienced persistent lateral hip discomfort and abductor weakness that was refractory to nonoperative measures. At final follow-up, all patients reported complete resolution of pain and had 5 of 5 abductor motor strength points on physical examination. Modified Harris hip scores at 1 year averaged 94 points and hip outcomes scores averaged 93 points.20
POSTOPERATIVE REHABILITATION
The general goals of early postoperative rehabilitation are a normalized gait pattern with crutches and the abduction orthosis. The hip is placed in an abduction brace postoperatively to protect the hip from active abduction and passive adduction past neutral. No active abduction and internal rotation or passive adduction and external rotation are permitted for at least 6 weeks to protect the structural integrity of the repair. Passive hip flexion to 90 degrees and passive abduction, however, is permitted as tolerated. Weight bearing is restricted to 20 pounds of foot-flat on the involved extremity for the first 6 weeks postoperatively. Continuous passive motion is initiated immediately for 4 hours, as well as stationary biking for 20 minutes daily. This is continued for the first 4 to 6 weeks postoperatively to avoid adhesions. Scar massage of the portals is initiated after initial healing at 10 to 14 days postoperatively.
1. Bunker TD, Esler CN, Leach WJ. Rotator cuff tears of the hip. J Bone Joint Surg Br. 1997;79:618-620.
2. Kagan A2nd. Rotator cuff tears of the hip. Clin Orthop Relat Res. 1999;368:135-140.
3. Howell GE, Biggs RE, Bourne RB. Prevalence of abductor mechanism tears of the hips in patients with osteoarthritis. J Arthroplasty. 2001;16:121-123.
4. Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis Rheum. 2001;44:2138-2145.
5. Beck M, Sledge JB, Gautier E, et al. The anatomy and function of the gluteus minimus muscle. J Bone Joint Surg Br. 2000;82:358-363.
6. Voos JE, Rudzki JR, Shindle MK, et al. Arthroscopic anatomy and surgical techniques for peritrochanteric space disorders in the hip. Arthroscopy. 2007;23:1246.
7. Robertson WJ, Gardner MJ, Barker JU, et al. Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy. 2008;24:130-136.
8. Dwek J, Pfirrman C, Stanley A, et al. MR imaging of the hip abductors: normal anatomy and commonly encountered pathology at the greater trochanter. Magn Reson Imaging Clin North Am. 2005;13:691-704.
9. Blankenbaker DG, Ullrick SR, Davis KW, et al. Correlation of MRI findings with clinical findings of trochanteric pain syndrome. Skeletal Radiol. 2008;37:903-909.
10. Cvitanic O, Henzie G, Skezas N, et al. MRI diagnosis of tears of the hip abductor tendons (gluteus medius and gluteus minimus). AJR Am J Roentgenol. 2004;182:137-143.
11. Lequesne M, Djian P, Vuillemin V, Mathieu P. Prospective study of refractory greater trochanter pain syndrome. MRI findings of gluteal tendon tears seen at surgery. Clinical and MRI results of tendon repair. Joint Bone Spine. 2008;75:458-464.
12. Craig RA, Jones DP, Oakley AP, Dunbar JD. Iliotibial band Z-lengthening for refractory trochanteric bursitis (greater trochanteric pain syndrome). ANZ J Surg. 2007;77:996-998.
13. Cormier G, Berthelot JM, Maugars Y, SRO (Société de Rhumatologie de l’Ouest). Gluteus tendon rupture is underrecognized by French orthopedic surgeons: results of a mail survey. Joint Bone Spine. 2006;73:411-413.
14. Ozçakar L, Erol O, Kaymak B, Aydemir N. An underdiagnosed hip pathology: apropos of two cases with gluteus medius tendon tears. Clin Rheumatol. 2004;23:464-466.
15. Connell DA, Bass C, Sykes CA, et al. Sonographic evaluation of gluteus medius and minimus tendinopathy. Eur Radiol. 2003;13:1339-1347.
16. Walsh G, Archibald CG. MRI in greater trochanter pain syndrome. Australas Radiol. 2003;47:85-87.
17. Lonner JH, Van Kleunen JP. Spontaneous rupture of the gluteus medius and minimus tendons, Oct;31. Am J Orthop. 2002; 579-581.
18. Kingzett-Taylor A, Tirman PF, Feller J, et al. Tendinosis and tears of gluteus medius and minimus muscles as a cause of hip pain: MR imaging findings. AJR Am J Roentgenol. 1999;173:1123-1126.
19. Chung CB, Robertson JE, Cho GJ, et al. Gluteus medius tendon tears and avulsive injuries in elderly women: imaging findings in six patients. AJR Am J Roentgenol. 1999;173:351-353.
20. Voos JE, Shindle MK, Pruett A, et al. Endoscopic repair of gluteus medius tendon tears of the hip. Am J Sports Med. 2009;37:743-747.