Abdominal Trauma
Perspective
The management of abdominal trauma should be approached in an organized, vigilant, and knowledgeable manner. Reliance on key clinical features and the timely use of diagnostic procedures tremendously alter morbidity and mortality. Advancements in imaging have helped to decrease missed or delayed diagnoses, yet they remain the most serious pitfalls in the management of abdominal injuries.1
Penetrating Abdominal Trauma
Whether by accident or intention, penetrating trauma can result from a wide variety of weapons or instruments, and certain elements of therapy vary accordingly. The management of patients with penetrating trauma has changed dramatically since 1960, when Shaftan introduced the concept of selective laparotomy and serial observations.2 Before that time, surgery was mandatory. The careful integration of physical examination and certain diagnostic procedures, notably local wound exploration (LWE), ultrasonography, computed tomography (CT), laparoscopy, and in rare instances, diagnostic peritoneal lavage (DPL), now provides the emergency physician and trauma surgeon with an accurate means of determining whether laparotomy should be undertaken. The approach varies according to the clinical status of the patient, the instrument responsible for injury, and the site of penetration. Nonoperative management has gained favor predominantly for stab wounds, though also for carefully selected gunshot wounds (GSWs), with the intent to reduce the incidence of and morbidity from nontherapeutic laparotomies.3,4
Epidemiology
Penetrating Abdominal Trauma
Wounds from stabbing implements occur nearly three times more often than wounds from firearms, but the latter have a significantly greater mortality rate and are responsible for 90% of penetrating trauma mortality.5 The small intestine, colon, and liver are, successively, the most likely organs to sustain injury after penetrating trauma.5 The highest risk of death from penetrating abdominal injury occurs among African Americans in the 15- to 34-year-old age range, followed by Hispanic persons in that same age group. The rate for non-Hispanic whites is greatest at 75 years of age and older. The predominant intent is homicide among African Americans and suicide among non-Hispanic whites.6
The use of firearms in the United States contributes heavily to the morbidity and mortality of trauma. The current U.S. civilian population is the most heavily armed in history. Over 42 million U.S. households have firearms, and there are more than 57 million gun owners.7 The number of homicides committed with firearms exceeds the number of homicides resulting from all other forms of violence combined. More than 850,000 American civilians were killed by bullets in the 20th century, and mortality from GSWs accounts for 12 per 100,000 deaths in urban areas.8
Blunt Abdominal Trauma
The automobile is the major cause of blunt abdominal trauma (BAT). Motor vehicle collisions (MVCs) and auto-pedestrian crashes have been cited as causes in 50 to 75% of cases, blows to the abdomen in approximately 15% of cases, and falls in 6 to 9%.9
Pediatrics
Each year in this country, trauma results in approximately 22,000 deaths and accounts for $160 billion of health care expenditures for children to the age of 16 years. Nearly 13% of children admitted to pediatric trauma centers are proven to have abdominal injury, and this category follows only head, neck, and thoracic trauma as the cause of injury-related death.10 Blunt mechanism causes approximately 85% of pediatric injury, although penetrating violence is becoming a greater concern. As is true with adults, MVCs are responsible for most of the morbidity and mortality in cases of trauma in children.8 Auto-pedestrian accidents and falls out of cars cause a significant percentage of these injuries.
Principles of Disease
The abdominal cavity and its contents can be reached not only through the anterior abdominal wall and lower chest but also through the flank, back, and buttocks. Missiles can also lodge intraperitoneally after traversing proximal extremities. The anterior abdomen is defined as that region between the anterior axillary lines from the anterior costal margins to the groin creases. The low chest begins at the nipple line or fourth intercostal space anteriorly and the inferior scapular tip or seventh intercostal space posteriorly, and then extends down to the inferior costal margins. The flank is between the anterior and posterior axillary lines bilaterally from the inferior scapular tip to the iliac crest. The back is between the posterior axillary lines, beginning at the inferior scapular tip and extending down to the iliac crest. The intraperitoneal cavity is vulnerable when penetration occurs as high as the fourth intercostal space anteriorly and the sixth or seventh laterally and posteriorly because the diaphragm can ascend to this level during expiration. Likewise, simultaneous thoracic abdominal penetration has been found in 20 to 40% of cases of abdominal thoracic trauma.11 Scrutiny of entrance and exit sites, as well as wound tracts, is imperative.
Pathophysiology
The liver, followed by the small bowel, is the organ most often damaged by stab wounds, in keeping with the surface area each of these structures presents.4 The frequency of organ injury caused by GSWs is greatest for small bowel, followed by the colon and then the liver.5 Typically, multiple organ injuries are sustained, notably perforations to bowel. This same pattern is seen in the pediatric patient.
Stab Wounds.: Knives are not the sole implements used in stabbings. Ice picks, pens, coat hangers, screwdrivers, and broken bottles, to name a few, have been used by assailants. Stab wounds of the abdomen occur most commonly in the upper quadrants, the left more commonly than the right. They are multiple in 20% of cases and involve the chest in up to 10% of cases. Most stab wounds do not cause an intraperitoneal injury, and the incidence varies with the direction of entry into the peritoneal cavity. Anterior stab wounds penetrate the peritoneum in approximately 70% of cases but inflict a visceral injury in only half of these.4 Left lower chest wounds are associated with a 17% incidence of intraperitoneal damage in addition to the expected high rate of thoracic and diaphragmatic injuries. Right lower chest wounds have a much lower incidence of 0% to 4%.12 Abdominal entries from the flank and back have reported incidences of up to 44% and 15%, respectively.13,14 The organ injured cannot be well predicted by the site of entry in the abdominal wall. The liver and spleen are the viscera most commonly damaged in cases of back and flank wounds.
Gunshot Wounds—Ballistics.: The science of ballistics is complex, but a few basic principles are helpful in understanding the pathophysiologic processes of these injuries. The magnitude of the injury is proportional to the amount of kinetic energy imparted by the bullet to the victim, according to the following equation:
where E is the kinetic energy (in foot-pounds), m is the mass of the bullet, v is the velocity of the bullet (in ft/s), and g is gravitational acceleration (in ft/s). In other words, the degree of injury depends on the mass of the bullet and the square of its velocity.15 Additional factors that affect injury created by a missile include the resistance and viscoelastic properties of the tissue through which it passes, as well as the stability of the missile in this medium. Missile velocities are categorized as low (slower than 1100 ft/s), medium (1100-2000 ft/s), and high (faster than 2000-2500 ft/s); the impact velocity is the most important determinant of wounding capability. The impact velocity depends on the distance between the firearm and the victim, the muzzle velocity, and various characteristics of the missile. At medium and high velocities, the missile has an explosive effect and creates a temporary passage in the tissue along its course. The size of this passage is directly proportional to the specific gravity of the penetrated tissue. This sudden formation of a tract displaces nearby organs and vascular structures, and bone and viscera may be fractured or torn without being directly struck by the missile. Several cases of an intraperitoneal injury caused by a bullet that remained extraperitoneal throughout its entire course have been reported.16 Solid viscera, such as the liver and spleen, are more vulnerable to this effect.
High-Velocity Missiles.: Wounds from high-velocity missiles involve additional problems. First, external contaminants tend to be dragged into the wound. Second, the closure of the tract immediately after the bullet’s passage may lead to an underestimation of tissue damage. Finally, high-velocity bullets can fragment internally. In fact, a missile at any velocity can fragment after contact with bone and cause additional multiple trajectories and injuries. Civilian wounds have usually resulted from low-velocity handguns, but unfortunately a trend toward more destructive weapons, such as the .38 and .357, may be occurring.
Shotgun Wounds.: The shotgun was designed to strike a small, fast-moving target at close range. Because of the ballistic shape of the individual pellets, a rapid falloff in velocity occurs, making this weapon ineffective in producing severe wounds at long distances. An initial muzzle velocity of 1300 ft/s drops to 950 ft/s within 20 yards, a decrease of 25%. At close range (<15 yards), however, the shotgun is extremely lethal.
Shotgun wounds have been previously classified in three groups according to the range and pattern of distribution. More recently, classification has been according to the pattern of injury on the victim. Based on distance from the weapon to the victim, type I wounds involve a long range (>7 yards) and a penetration of subcutaneous tissue and deep fascia only. Type II wounds occur at a distance of 3 to 7 yards and may create a large number of perforated structures. Type III wounds occur at point-blank range (<3 yards) and involve a massive destruction of tissue. When categorized by pattern, type I wounds produce a spread greater than 25 cm in diameter; type II, 10 to 25 cm in diameter; and type III, less than 10 cm in diameter.17 The tissue damage is proportional to the specific gravity and inversely proportional to the elastic properties of the affected organ. Thus the liver is more vulnerable than the lungs to this injury. Close-range shotgun wounds, in addition to the shot, force external contaminants (e.g., clothing and parts of the shell wadding) into the wounds. Type III wounds carry a substantial mortality risk.
Blunt Abdominal Trauma
Seatbelt Injuries.: Unrestrained front and rear seat passengers are at unequivocally greater risk of intra-abdominal injury than their restrained counterparts.18 The three-point shoulder-lap belt is the most effective restraining system and is associated with the lowest incidence of abdominal injuries, compared with older systems. However, abdominal injuries are still ascribed to combined shoulder-lap and lap-belt systems. The shoulder belt component can lead to right-sided and left-sided rib fractures for the driver and front seat passenger, respectively, with potential for injury to underlying abdominal viscera. Improper underarm usage of the shoulder belt increases compressive forces to the upper abdomen, particularly in the event of a front-end crash.
Clinically, two symptom patterns emerge. Approximately one fourth of these patients develop evidence of a hemoperitoneum secondary to mesenteric lacerations. In the remainder, the intestinal injury most commonly involves the jejunum, and the initial signs and symptoms are often absent or considered insignificant. Subsequent delays in diagnosis of up to 8 weeks have rarely been reported. The “seatbelt sign,” contusion or abrasion across the lower abdomen, is found in less than one third of patients with abdominal injuries caused by lap belts. Its presence, however, is highly correlated with intraperitoneal pathologic lesions.19 Rupture of the diaphragm can also occur. Rare cases of acute abdominal aortic dissection with incomplete or complete occlusion have also been described, and injuries to the lumbar spine are not uncommon.20
Iatrogenic Injuries.: Although well intentioned, diagnostic and therapeutic efforts in patient care are not risk-free. Abdominal injuries may be sequelae of various medical procedures and in certain instances not only are extremely difficult to recognize but may contribute to or cause pronounced morbidity or death. Numerous procedures may cause an iatrogenic injury.
Artificial ventilation can lead to gastric distention, particularly in children. Besides compromising ventilation and increasing the risk of vomiting and aspiration, a significant distention may lead to an esophageal or gastric laceration and perforation. These may occur with bag-mask ventilations, an inadvertent esophageal intubation with a nasotracheal or endotracheal tube, or the mistaken connection of the nasogastric tube to oxygen rather than suction. Esophageal, gastroesophageal junction, and gastric lacerations are evidenced by bloody emesis or nasogastric return. If a gastric perforation occurs and positive-pressure breathing is maintained, a tension pneumoperitoneum or abdominal compartment syndrome may ensue with inferior vena cava compression and decreased cardiac output. External cardiac compressions have produced splenic, hepatic, and gastric injuries. Manual thrusts to clear an airway obstruction, as taught in basic life support courses, and the Heimlich maneuver have caused rib fractures with lacerations and the rupture of abdominal viscera. In cases of a cardiac arrest, these injuries may be occult but life-threatening. If hypotension occurs after cardiopulmonary resuscitation, an abdominal injury and hemorrhage are considered along with cardiogenic shock.21
A liver biopsy can lead to a hemoperitoneum or hemobilia. Endoscopic procedures of the bowel may cause a hollow viscus perforation and peritonitis, particularly when a biopsy is performed, although they can result from rapid retraction of the endoscope without biopsy, as well.22 Peritoneoscopy has been reported to cause small bowel perforations and iliac vessel lacerations. Barium enemas have an extremely low incidence of perforation but can be another cause of unexplained peritonitis and pneumoperitoneum.
Clinical Features
Penetrating Abdominal Trauma
Stab Wounds.: It is helpful to obtain information regarding the mode of injury from the patient, paramedic, or witnesses. The number of stabs inflicted, type and size of the instrument, posture of the victim relative to the direction of assault, estimated blood loss at the scene, time of injury, and response to fluids should be sought. However, a significant proportion of victims of stab wounds are found under the influence of alcohol or another drug. This state can make obtaining an accurate history a futile effort and further compromises the validity of symptoms and signs.
Gunshot Wounds.: As initial stabilization measures are instituted in the emergency department, the emergency physician can elicit certain facts that can contribute greatly to the evaluation of the patient. These include the weapon used, its distance from the victim when shot, the position of the victim in relationship to the weapon when fired, the suspected number of shots, the blood loss at the scene, the amount and type of field fluids administered, and the vital signs during the prehospital course.
Physical Examination
Hypotension in the acute stage results from hemorrhage that is most often from a solid visceral or vascular injury. Traumatic pancreatitis may produce significant third-space fluid loss, but hours to days are usually required for this to appear, and shock is an uncommon presentation.23 When hypotension accompanies significant multiple blunt trauma and is unexplained, one should assume the presence of intraperitoneal hemorrhage until it is excluded. However, a known extra-abdominal source of hemorrhage does not mitigate the need to evaluate the peritoneal cavity. A head injury alone does not explain shock except in cases of profound head injury or in the very small infant, in whom traumatic intracranial or extracranial (e.g., cephalohematoma) blood loss may be proportionally substantial.24
Palpation elicits local or generalized tenderness in approximately 90% of alert patients with an intra-abdominal visceral injury. Local and generalized rebound tenderness and rigidity can be signs of peritoneal irritation and occur less commonly. These signs lack specificity, however, and can be found with lower rib fractures and contusions of the thoracoabdominal wall. These findings or, more important, their absence, are more reliable in alert patients. However, false-positive and false-negative abdominal manifestations have been well demonstrated even in conscious, responsive patients.25,26
A rectal examination rarely reveals blood or subcutaneous emphysema, but the presence of either is highly correlated with abdominal injuries. The rectal examination is now considered less helpful than clinical indicators such as blood at the meatus or scrotal hematoma in urethral injuries, or evidence of paralysis. The rectal examination can be eliminated or deferred in many patients, as the clinical indicators noted earlier appear to be more sensitive than the rectal examination.27–29 Notable exceptions may include suspected cauda equina syndrome or penetrating trauma to the perirectal area.
Penetrating Abdominal Trauma
Stab Wounds.: Serial physical examinations performed by the same observer are gaining acceptance in certain centers where these have been found useful, particularly with patients who are alert, communicative, and neurologically intact. The presence of intoxicants does not necessarily preclude reliance on examination but may undermine its value.30 In other series, patients with impressive physical findings after penetrating trauma to the abdomen have undergone exploratory laparotomy, with negative results in 14 to 28% of cases.31 Moreover, up to one third of patients with significant intra-abdominal injuries have no suggestive physical signs, particularly when a retroperitoneal injury has occurred.32 Therefore serial clinical evaluations typically involve physical examinations to include trending of vital signs, laboratory testing including serial hemoglobin measurement, and repeated focused assessment with sonography in trauma (FAST) examinations.
Gunshot Wounds.: As with blunt or other modes of penetrating trauma, there is dispute regarding the value of the physical examination of patients with abdominal GSWs. In various series, 20% of patients with a documented intraperitoneal injury had no peritoneal signs before exploration.32 Moreover, objective physical findings suggestive of intra-abdominal damage have been misleading and falsely positive in 15% of patients in whom laparotomy revealed no injury. Other authors contend that selective management can be undertaken safely when physical examination is the fundamental evaluative measure.30
Blunt Abdominal Trauma
Overall, the accuracy of the physical examination in patients with BAT is 55 to 65%.25 The initial presentation may be exceptionally benign in cases of blunt intra-abdominal injury. The most reliable symptoms and signs in alert patients are pain, tenderness, and peritoneal findings, particularly when risk factors for abdominal injury are present. When altered sensorium intercedes, the physical signs become less reliable. Frequent evaluations by the same examiner are indicated even in alert patients, but especially in sensorium-altered patients, particularly as their mental status and sensorium normalize.
Diagnostic Strategies
Hematologic and chemical values are of limited use in the management of the acutely traumatized patient.33 They should be considered adjuncts to diagnosis and not substitutes for clinical assessment.
Hematology
Hematocrit.: The hematocrit reflects baseline value, extent of and time from hemorrhage, exogenous fluid administration, and endogenous plasma refill. The last of these is a physiologic compensatory shift of extracellular fluid into the intravascular space, the intent of which is to restore the original blood volume. Based on a study of volunteers sustaining a 10 to 20% blood loss, this restoration proceeds at a rate of only 40 to 90 mL/hr for the first 10 hours and requires 30 to 40 hours for completion.34 However, patients evidencing hemorrhagic shock with a blood loss of at least 40% demonstrate much faster plasma refill rates, estimated as high as 1500 mL in the first 90 minutes after injury, with significant decreases in hematocrit within this period. Although the hematocrit is an easily acquired measure, it is often a conundrum when viewed in isolation, and serial determinations are more helpful.
White Blood Cell Count.: The white blood cell (WBC) count has little discriminatory value in cases of abdominal trauma, particularly its acute phase.33 The WBC count may be normal or may show a modest leukocytosis (12,000 to 20,000/mm3 with or without left shift), which can occur in the setting of multisystem trauma as a result of stress-induced demargination in the absence of any intra-abdominal process, or as a result of tissue injury, acute hemorrhage, or peritoneal irritation.
Chemical
Pancreatic Enzymes.: Neither serum amylase nor lipase is useful in the evaluation of acute abdominal trauma. Normal levels do not exclude a major pancreatic injury, and elevated values may be caused by any of an assortment of reasons in addition to an injured pancreas. The use of serum amylase isoenzymes has not appreciably improved accuracy. Nontraumatic causes of hyperamylasemia include several diseases and the use of alcohol, opioids, and various other drugs. Amylase or lipase may also be elevated with pancreatic ischemia produced by the systemic hypotension that often accompanies trauma. Clearly, these enzymes are neither highly specific nor sensitive for pancreatic injuries. Elevated or rising levels may indicate damage but in themselves are not conclusive.35 In these cases, clinical correlation and further investigation are indicated.
Base Deficit.: Metabolic acidosis in the setting of trauma can suggest the presence of hemorrhagic shock. This can be witnessed chemically as a decreased serum bicarbonate level, increased base deficit, or elevated serum lactate level. Although normal values do not exclude abdominal injury, substantive abnormalities, such as a base deficit greater than or equal to 6, may be predictive. These findings should be considered in clinical context, because the resolution of the laboratory findings will lag behind the clinical improvement of the patient.
Liver Function Tests.: Elevated serum transaminases can result from hepatic trauma but do not distinguish minor contusions from severe injury.36 Alternatively, these may be symptomatic of alcohol-induced liver damage. Elevated liver transaminase levels may be useful for screening pediatric patients for intentional trauma (see Chapter 38). They may also play a role in pediatric patients in combination with a FAST examination as a screening tool to decrease the use of CT scanning, although serial physical examination is still required.37
Toxicology Analysis.: Screens for ethanol and drugs are often used in trauma centers. Their utility in the management of abdominal trauma, per se, has not been established, particularly in patients with normal mental status.38 Positive study findings may prompt the emergency physician to interdict and the patient to decrease the recidivistic use of ethanol or drugs, and physician intervention during this “teaching moment” has been shown to be effective.
Radiology
Plain Radiographs
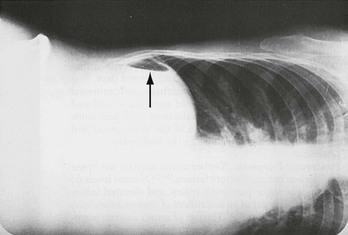
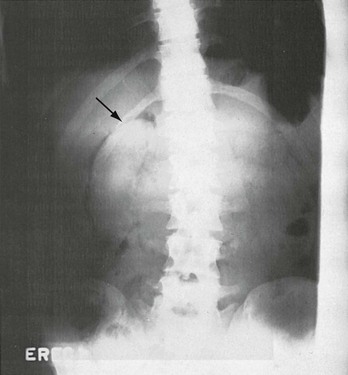
Very small quantities of readily detectable free intraperitoneal air are present in most patients with gastric, duodenal bulb, and colonic perforations but in fewer than one fourth of those with jejunal and ileal perforation. These are seen more readily on CT than plain films. Free intraperitoneal air uncommonly can be generated by mediastinal or pulmonary injury, as well as by barotrauma, and thus its presence is not pathognomonic of hollow viscus perforation. Intraperitoneal air is mobile, and to maximize visualization the patient should be kept in the appropriate upright or decubitus position for 10 to 15 minutes, if this is tolerable, before upright chest or decubitus abdominal radiographs are obtained. In upright films, air is located under the diaphragm or the central tendon of the diaphragm anteriorly. In supine films, air tracks under peritoneal attachments, such as the falciform ligament and urachus, up to the anterior abdominal wall. On films in which the patient is in a lateral decubitus position, air is located in the superior flank and outlines the lateral liver edge (Fig. 46-1). In cases of gastric perforations, air may be limited to the lesser sac. A rupture of a retroperitoneal hollow viscus can be detected by a stippling pattern outlining the duodenum, kidney, or psoas muscle (Fig. 46-2). Extraperitoneal colonic perforations may extravasate air, which outlines the psoas muscle and perinephric region. All of these injuries are much more readily identified and localized on abdominal CT.
Computed Tomography
Over the last 35 years, CT scanning has continued to advance its place among diagnostics for trauma. Evolution to higher multislice helical and spiral scanners has improved resolution and greatly decreased the time required for the scan itself.39
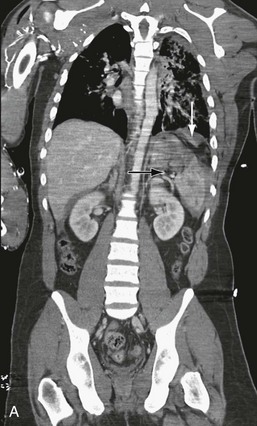
Advantages.: In most situations, CT scanning has supplanted DPL because of its higher predictive ability for operative lesions and because it is noninvasive. CT scanning can define the injured organ and the extent of the injury. It is most accurate for solid visceral lesions and accurately discerns the presence, source, and approximate quantity of intraperitoneal hemorrhage (Fig. 46-3). It can demonstrate active bleeding from the liver or spleen and can be used to determine whether therapeutic angiographic embolization is indicated.40 CT scanning also evaluates the retroperitoneum (Fig. 46-4), an area not sampled by DPL, as well as the vertebral column, and can be readily extended above or below the abdomen to visualize the thorax or pelvis.41 CT scanning also provides definitive evaluation for most possible injuries to the urinary tract, including renal artery injury.42 It can also detect other vascular hemorrhage and obviate the need for angiography in some patients.43 CT scanning is particularly helpful in guiding nonoperative management of solid organ damage.44,45 This includes as-needed follow-up studies of convalescing patients with these injuries. It has also proven effective when incorporated in delayed fashion for patients with decreasing hematocrit, increasing base deficit, or subtle examination changes. By minimizing the incidence of nontherapeutic laparotomies for self-limited injury to the liver or spleen, it decreases morbidity and cost attendant to this operation.46 Increasingly, trauma centers are using CT with intravenous contrast only, as it has been shown that little additional information is provided by the addition of oral contrast, which delays scanning and may pose an aspiration risk for the patient.47,48

Figure 46-3 Grade 4 splenic laceration.
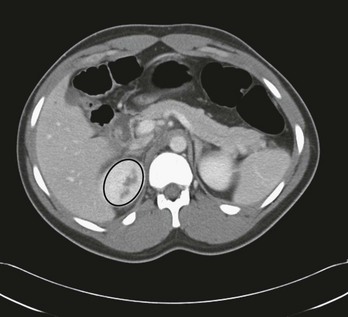
Figure 46-4 Grade 3 right renal laceration (encircled).
Disadvantages.: Disadvantages of CT scanning include relative insensitivity for injury of the pancreas, diaphragm, small bowel, and mesentery, although detection of these injuries is improving47,48 (Fig. 46-5). The last two are particularly worrisome because isolated coincidental hollow viscus injury in patients with blunt trauma, although uncommon, is not rare, and increased morbidity and death can ensue if diagnosis is missed or the condition goes undetected for a prolonged period. Findings on CT scans, including the suspected quantity of hemoperitoneum or the presence of isolated free fluid, are not able to forecast well the need for operative intervention.49 Complications can result from intravenous contrast administration or uncommonly from contrast material administered orally. Moreover, oral contrast delivery to opacify bowel is infrequently useful and typically omitted.47,50 Finally, patients must be temporarily removed from the resuscitation area for the study to be accomplished, which can put the patient at risk in the case of rapid clinical deterioration. However, CT scanning remains the cornerstone of diagnosis. In cases with equivocal CT scan results, such as more than physiologic fluid, or a worrisome history and physical examination findings, serial examinations or further diagnostic testing should be strongly considered, including DPL, particularly to evaluate for missed hollow viscus injury (Table 46-1).
Table 46-1
Preferred Site of Diagnostic Peritoneal Lavage
| CLINICAL CIRCUMSTANCE | SITE | METHOD |
| Standard adult | Infraumbilical midline | C or SO |
| Standard pediatric | Infraumbilical midline | C or SO |
| Second- and third-trimester pregnancy | Suprauterine | FO |
| Midline scarring | Left lower quadrant | FO |
| Pelvic fracture | Supraumbilical | FO |
| Penetrating trauma | Infraumbilical midline* | C or SO |
C, closed (percutaneous Seldinger technique); FO, fully open; SO, semiopen.
*The stab wound or gunshot wound site should be avoided.
Adapted from Runyon, M, Marx JA: Peritoneal procedures. In Roberts JR, Hedges JR (eds): Clinical Procedures in Emergency Medicine, 5th ed. Philadelphia, WB Saunders, 2009.
Radiation Risk.: Increasingly, there is concern regarding the negative long-term effects from exposure to ionizing radiation resulting from medical imaging. Over 62 million CT scans are performed per year in the United States, including over 4 million in children,51 and the number of scans performed per patient after trauma is increasing.52 Based on data from survivors of the atomic bombs dropped on Japan and average radiation exposure from various types of CT scans, it has been estimated that 0.4% of all cancers in the United States have been caused by exposure to medical radiation, and that number may be increasing to 1 to 2%. Children are especially at risk, and even a single CT scan may increase the lifetime risk of cancer.51 Although direct evidence of increased cancer risk from CT scans has not yet been demonstrated, several methods are becoming available to reduce radiation exposure. Some groups have attempted to define decision rules to help avoid unnecessary CT scans in very low-risk patients, though their role in clinical practice has yet to be defined.37,53,54 For very low-risk, hemodynamically stable patients, special consideration should be given to patients with large numbers of negative CT scans in the past, and observation may be preferable to repeat radiation exposure. Adjustment of scanning techniques for children and body habitus on an institutional level through use of “as low as reasonably achievable” (ALARA) principles, developed in conjunction with the department of radiology, can decrease excessive radiation exposure if CT scanning is clinically indicated. If a patient is to be transferred to another facility, attempts should be made to convey hard copy or digital images to the accepting facility, as CT scans are not infrequently repeated at the receiving hospital.55 These repeat CT scans are unlikely to change management without a concurrent change in clinical picture.56 A balance between minimizing radiation exposure and simultaneously minimizing the number of missed injuries is a challenge for the emergency physician evaluating a patient with abdominal trauma.
Technique.: The technique for CT scanning is reasonably standardized, but certain conventions are debated. The studies should begin in the low chest and be taken through the pelvis. If chest scanning is also required, a single continuous scan is obtained from the root of the neck to the floor of the pelvis. “Quick look” but less thorough studies are problematic and should be avoided; preliminary reads from the CT control room do not have the added accuracy of reconstituted scans and may therefore miss subtle injuries, such as intimal tears of the thoracic aorta. Most centers perform enhanced (intravenous contrast) and nonenhanced scans because the latter alone may not demonstrate intraparenchymal hematomas well. Other practitioners believe that the noncontrast portion contributes little other than time to the procedure. In patients who undergo chest and abdominopelvic CTs, reconstituted images can be obtained of the thoracolumbar spine, sparing the need for additional studies and associated ionizing radiation. Except in certain unusual circumstances, single scans through the areas of interest with intravenous contrast only are recommended.
Contrast Studies
Contrast studies with a water-soluble medium (e.g., Gastrografin) can be helpful in cases of suspected gastric, duodenal, and rectal perforations (Fig. 46-6). Barium mixtures should be used to visualize intramural duodenal hematomas.57 However, a CT scan should be able to discern duodenal hematomas and can distinguish these from perforations.58
Therapeutic Angioembolization
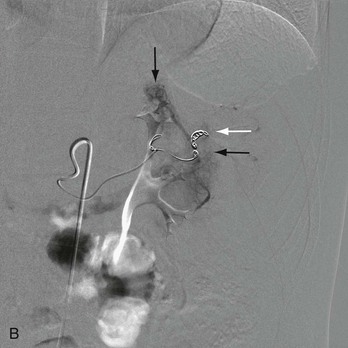
Therapeutic angiography, a time-consuming procedure, is usually reserved for the unstable patient with blunt trauma and pelvic fracture in whom it can be used to embolize bleeding vessels (Fig. 46-7). It can also be a means of staunching solid visceral hemorrhage from blunt trauma, notably of the spleen.40 Nonoperative management has become standard in management of splenic injuries but is associated with increasing failure rates with increasing grades of injury, up to 44% with the highest-grade injuries. Successful nonoperative management has been demonstrated to increase significantly with the use of angioembolization therapy,59 though higher-grade injuries are still more likely to fail nonoperative management than lower-grade injuries.60 Angioembolization also may have the added benefit over splenectomy of preserved splenic immunity in many cases, though further data are needed on the topic.59 The angioembolization catheter should be inserted as close as possible to the hemorrhaging lesion to minimize infarction of viable tissue. Finally, angioembolization also has been used rarely for intraperitoneal and retroperitoneal hemorrhage after trauma by a penetrating mechanism.
Bedside Procedures
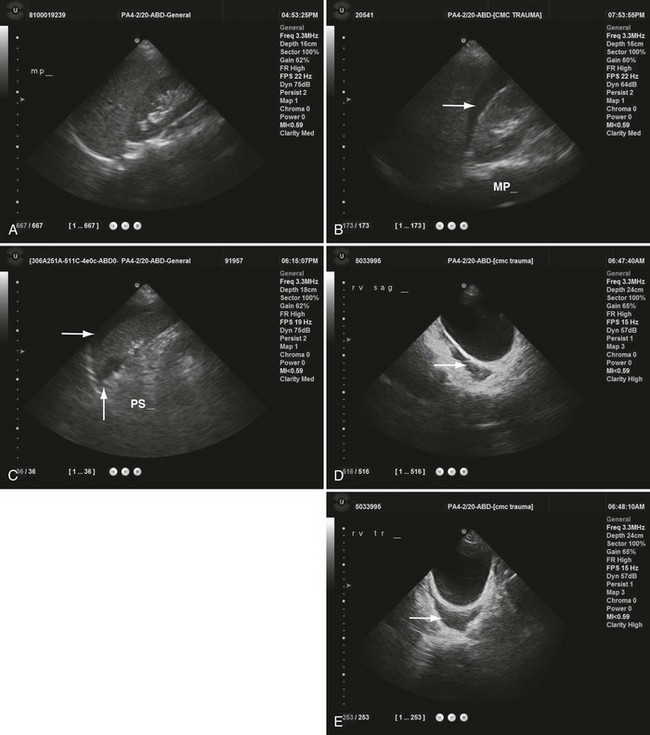
Ultrasonography’s primary role is detecting free intraperitoneal blood after blunt trauma. This is accomplished by a FAST ultrasound examination of Morrison’s pouch, the splenorenal recess, and the pouch of Douglas, which are dependent portions of the intraperitoneal cavity where blood is likely to accumulate (Fig. 46-8). Anechoic areas caused by the presence of blood are best visualized when contrasted against solid organs (e.g., liver, spleen, and kidneys). With penetrating mechanisms, an extended FAST (E-FAST) ultrasound adding visualization of the pleura and pericardial and intraperitoneal spaces can also detect pneumothorax, hemothorax, and pericardial tamponade.61
Advantages.: Ultrasonography carries a host of advantages. It is a portable instrument that can be brought to the bedside in the trauma resuscitation area. Studies of the pericardial, intraperitoneal, and thoracic spaces can be accomplished in less than 5 minutes. FAST ultrasound has a sensitivity in detecting as little as 100 mL and, more typically, 500 mL of intraperitoneal fluid that ranges from 60 to 95% in most recent studies, and specificity for hemoperitoneum is excellent.62 Therefore when time is precious in the patient in critical condition, the FAST can provide a rapid answer to the key question in the decision matrix, which is whether hemoperitoneum is present. Unlike DPL, the FAST can evaluate intrathoracic structures, is noninvasive, and can be performed serially and by multiple technicians. Unlike CT scanning, it is not a potential radiation hazard and does not require administration of contrast agents. Accuracy correlates with length of training and experience, but expertise can be readily achieved in emergency medicine and surgical training programs.63 Serially performed FAST increases its diagnostic accuracy for organ injury in patients with BAT.64,65 Furthermore, E-FAST adds thoracic windows to detect the presence of pneumothorax in patients who have sustained penetrating abdominal trauma (PAT) or BAT. These additional views detect pneumothorax with a sensitivity of almost 60% and a specificity of up to 99% when compared with CT, but more important, the E-FAST is three times as sensitive as a portable supine chest x-ray examination done in the trauma bay, which has a sensitivity of only 20%.66 Overall, ultrasonography can serve as an accurate, rapid, and less expensive diagnostic screening tool than DPL or CT.67–69
Disadvantages.: The FAST study does not image solid parenchymal damage, the retroperitoneum, or diaphragmatic defects well. It is technically compromised by the uncooperative, agitated patient, as well as by obesity, substantial bowel gas, and subcutaneous air. Indeterminate studies require follow-up attempts or alternative diagnostic tests.65 It is less sensitive and more operator dependent than DPL in revealing hemoperitoneum and cannot distinguish blood from ascites or uroperitoneum. For unclear reasons, ultrasound has a high (31%) false-negative rate in detecting hemoperitoneum in the presence of pelvic fracture.70 The FAST study, like DPL, will not detect the presence of solid parenchymal damage if free intraperitoneal blood is absent, as in subcapsular splenic injury.70,71 Finally, ultrasonography is poor at recognizing bowel injury in which hemorrhage tends to be inconsequential, and failure to diagnose hollow viscus perforation in a timely manner can have catastrophic results.72 Because of these limitations, reliance on a single negative FAST examination performed within minutes of the injury is ill-advised. Serial FAST examinations may help to determine progressive hemorrhage, however.
Diagnostic Peritoneal Lavage
Advantages.: In cases of blunt trauma, DPL’s primary remaining use is in the triage of the patient who is hemodynamically unstable and has multiple injuries with an equivocal FAST examination or in the patient in whom FAST cannot be obtained owing to the absence of equipment or competent personnel.73 In such complex scenarios, DPL can promptly reveal or exclude the presence of intraperitoneal hemorrhage and can serve as an indication for laparotomy. Rarely, DPL is used to discern potentially serious bowel perforations in patients who are poor candidates for serial clinical observations (e.g., coma) and for which other diagnostic methods can be unreliable.74
Disadvantages.: The morbidity associated with DPL occurs at a low rate and can be categorized as local or systemic infection, intraperitoneal injury, and technical failure. Wound complications, including hematoma and infection, occurred in 0.3% of cases in two large reviews.75 Technical failure can result in an inaccurate study and difficulty with fluid collection. In addition, DPL is exquisitely sensitive for hemoperitoneum and in a hemodynamically stable patient can lead to unnecessary laparotomy. False-negative interpretations can result from the failure to recover lavage fluid.
Results.: In cases of blunt trauma, the aspiration of 10 mL or more of blood has a positive predictive value of greater than 90% for intraperitoneal injury, predictably solid visceral or vascular, and is responsible for approximately 80% of true positive DPL findings in blunt trauma.75 The red blood cell (RBC) count of the lavage fluid is the next most widely used and accurate parameter (Table 46-2). In cases of blunt trauma, an RBC count exceeding 100,000/mm3 is considered positive and generally specific for injury. However, while sensitive to the presence of injury, it may detect self-limited pathology for which laparotomy is unnecessary.
Table 46-2
Diagnostic Peritoneal Lavage Red Blood Cell Criteria (per mm3)
| POSITIVE | INDETERMINATE | |
| Blunt trauma | 100,000* | 20,000-100,000 |
| Stab wound | ||
| Anterior abdomen | 100,000 | 20,000-100,000 |
| Flank | 100,000 | 20,000-100,000 |
| Back | 100,000 | 20,000-100,000 |
| Low chest | 5000-10,000 | 1000-5000 |
| Gunshot wound | 5000-10,000 | 1000-5000 |
*In a hemodynamically stable patient with pelvic fracture and positive or equivocal red blood cell count, computed tomography should be obtained to corroborate or refute intraperitoneal injury.
There is a well-known association between false-positive peritoneal lavage in the setting of retroperitoneal hematoma and pelvic fracture.76 CT scanning is the standard method by which pelvic fracture with possible retroperitoneal or intraperitoneal hemorrhage is evaluated.77
With anterior abdominal stab wounds, aspiration of 10 mL of gross blood or the return of lavage fluid with an RBC count greater than 100,000/mm3 carries a sensitivity exceeding 90% (see Table 46-2).78 It is recommended that patients with equivocal RBC counts be carefully observed for 12 to 24 hours.79 Most injuries associated with RBC counts less than 100,000/mm3 are to hollow viscera, and clinical manifestations of these should develop within this observation period. With lower chest stab wounds, a positive RBC count of 5000 to 10,000/mm3 should be considered to be evidence of diaphragmatic injury. Because of the more serious nature and greater likelihood of an injury with abdominal GSWs, RBC counts of 5000/mm3 are advocated as the cutoff, as these will signal peritoneal penetration, if not injury.75 However, laparoscopy has supplanted DPL for the purpose of identifying or excluding diaphragmatic injury in lower chest penetrating trauma.
Local Wound Exploration
Because stab wounds do not reach the peritoneum in a significant number of cases, LWE is useful in determining the depth of penetration. The wound should be infiltrated with a local anesthetic containing epinephrine and thoroughly prepared for exploration. The stab wound may be extended if required and then carefully visualized through each successive layer of tissue. Blind probing with digits, instruments, or cotton-tipped swabs is inaccurate, unless the peritoneal cavity is obviously freely entered. Blind probing of chest injuries adds no potential additional information and may be hazardous. If LWE indicates that the peritoneum is violated, further diagnostics are indicated. Likewise, when the end of the wound tract cannot be determined clearly, peritoneal entry is presumed. When the stab wound is documented to be superficial to the abdominal cavity, the patient can be safely discharged home after appropriate wound care.80
LWE is generally advocated in cases of anterior abdominal stab wounds, but in other areas the decision is less clear. Abdominal, flank, and back wounds have been evaluated with this method, particularly when the entry is more superficial.13,14,81 The flesh of obese or heavily muscled patients in particular can present technical problems and decrease the reliability of exploration while increasing its risk. Wound explorations in patients with multiple entrances are not economical and require extensive effort, and it may be wiser to assume peritoneal penetration. Deep exploration over the thoracic cage is precluded by attendant complications to neurovascular structures and pleura. However, careful inspection of superficial chest wounds (e.g., slash wound) is safe and can provide valuable data. CT, laparoscopy, or thoracoscopy is occasionally used in lieu of LWE.
Special Procedures
Laparoscopy is increasingly finding a role in some trauma centers. General anesthesia in an operating suite is required. Laparoscopy has been most useful in assessing penetrating trauma, especially for injury to the diaphragm and intrathoracic abdominal organs.82 It has a reported sensitivity of 87.5% and specificity of 100% for detection of diaphragmatic injury after PAT, with a positive predictive value of 100% and negative predictive value of almost 97%.83 Organs repaired via the laparoscope include the diaphragm, solid intraperitoneal viscera, stomach, and small bowel. Wound tracts have been assessed as accurately as by LWE. Very little experience in blunt trauma has been documented thus far.
Drawbacks of laparoscopy include poor sensitivity for hollow visceral injury, notably to the small bowel, and difficulty in assessing the retroperitoneum and extent of damage to the liver and spleen.83 Complications can result from trocar misplacement. If the diaphragm has been violated by the original trauma, pneumothorax or tension pneumothorax can occur during the insufflation phase. At this time the greatest value of laparoscopy is in the evaluation and management of equivocal penetrating wounds to the thoracoabdominal region of stable patients. This approach can realize a reduced incidence of nontherapeutic laparotomy.84,85
Differential Considerations
Management
Prehospital
The field approach to multiple or serious trauma focuses on rapid transportation to a capable receiving emergency department. The initial measures taken vary with the need for active airway management, the presence of concomitant injuries, and the skills of the prehospital personnel. Hemorrhage is the major life threat in cases of PAT or BAT, and two large-bore intravenous lines should be inserted in transit when possible,86 though delay at the scene for insertion of intravenous lines should not occur unless extrication is prolonged. Penetrating wounds and eviscerations in particular should be covered with sterile dressings. Contact should be made with the base-station physician to communicate pertinent matters of the history, vital signs, treatment measures and their effects, and estimated time of arrival. Certain authors advocate for direct transport to high-level trauma centers unless airway management is a concern.87
Emergency Department
The general principles of trauma care apply (see Chapter 36). The use of diagnostic aids for abdominal trauma should be carefully restricted according to the patient’s stability and the usefulness of the information sought in guiding management. Patients who do not require immediate laparotomy will likely undergo one or more diagnostic procedures to determine whether abdominal injury exists and, if so, whether operative intervention is necessary.
Thoracotomy.: Thoracotomy and subsequent cross-clamping of the descending aorta have been used to stabilize patients with thoracoabdominal injuries and profound hypovolemic shock. However, it is rarely lifesaving in the emergency department (see Chapter 45).
Antibiotics.: An intestinal perforation and spillage can occur after blunt or, more commonly, penetrating trauma to the abdomen. Anaerobes and coliforms are the predominant organisms found. Antibiotics given prophylactically have been demonstrated to be effective in decreasing the incidence of intra-abdominal sepsis and should be given as soon as such an injury is suspected. A single preoperative dose of a broad-spectrum antibiotic or combination of antibiotics that covers both aerobic and anaerobic organisms, such as piperacillin-tazobactam 3.375 g intravenously, is recommended.88
Penetrating Abdominal Trauma: Stab Wounds
Management
Selective management of abdominal stab wounds is now well accepted because of the relatively low incidence of intraperitoneal injuries coupled with the success of various diagnostic strategies.89,90 The appropriateness of these strategies is predicated on the site of penetration, the clinical status of the patient, and the experience and preference of an institution and its personnel. Formerly, the goal of mandatory exploration of all stab wounds was to eliminate missed injuries. Currently, selective management has resulted in a tremendous reduction in unnecessary laparotomies and their associated morbidity, with minimal and acceptable loss in sensitivity for significant intraperitoneal injury.90 Although certain authors promote the relative safety of nontherapeutic operations, others cite considerable immediate and delayed hazards, as well as increased cost.80 It is generally preferred that the nondiagnostic laparotomy rate be less than 15%.
Anterior Abdomen.: In approaching the management of stab wounds to the anterior abdomen, the clinician is faced with three fundamental tasks. The first and most important is to determine whether clinical indications exist for laparotomy. The presence of one or more of these indications, particularly in the context of an unstable patient, sets the course to exigent operation. If none is found, however, the clinician may address the second issue of whether the peritoneal cavity has been violated. If it can be definitively demonstrated that it has not, no further diagnostic evaluation is required, and the patient can be discharged after appropriate wound care. If the cavity has been violated, or if it cannot be determined that the cavity has not been violated, the third question is pursued: does injury exist and, if so, is laparotomy required? One general approach to abdominal stab wounds founded on these three queries is summarized in Figure 46-9. This algorithm is largely based on clinical indicators of injury, LWE, CT, and other radiologic modalities. In centers without such resources, diagnostic peritoneal aspiration and lavage may still have a limited role. Other strategies rely more heavily on other techniques, such as serial abdominal examinations or laparoscopy.91–94
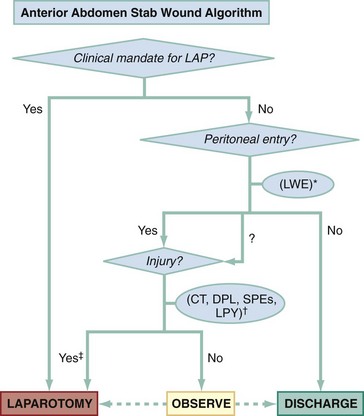
Figure 46-9 Anterior abdomen stab wound algorithm. LAP, laparotomy; LWE, local wound exploration.
*Plain films, focused assessment with sonography in trauma (FAST), laparoscopy (LPY), and computed tomography (CT) can also assess peritoneal entry.
†CT, diagnostic peritoneal lavage (DPL), serial physical examinations (SPEs), or LPY can be used in singular or complementary fashion, depending on the clinical scenario.
‡Expectant management of injuries is infrequently attempted.
Step I: Clinical Indications for Laparotomy.: Seven clinical determinants are used to predict the need for laparotomy after stab wounds to the abdomen (Table 46-3). Although there is general consensus regarding the reliability of some of these, each has suboptimal predictive value.
Table 46-3
Clinical Indications for Laparotomy Following Penetrating Trauma
| Manifestation | Premise | Pitfall |
| Hemodynamic instability | Major solid visceral or vascular injury | Thorax or mediastinum, causal or contributory |
| Peritoneal signs | Intraperitoneal injury | Unreliable, especially immediately postinjury |
| Evisceration | Additional bowel, other injury | No injury in one fourth to one third of stab wound cases |
| Diaphragmatic injury | Diaphragm | Rare clinical, radiographic findings |
| Gastrointestinal hemorrhage | Proximal gut | Uncommon, unknown accuracy |
| Implement in situ | Vascular impalement | Comorbid disease or pregnancy creates high operative risk |
| Intraperitoneal air | Hollow viscus perforation | Insensitive; may be caused by intraperitoneal entry only or may have cardiopulmonary source |
Modified from Marx JA: Diagnostic peritoneal lavage. In Ivatury RR, Cayten CG (eds): The Textbook of Penetrating Trauma. Baltimore, Williams & Wilkins, 1996.
1. Hemodynamic compromise. This is the preeminent indication of the need for laparotomy and is the most likely reason that a patient will be taken urgently to the operating room without preliminary diagnostic studies. This is typically an appropriate approach after middle and lower abdominal penetration.94–96 However, stab wounds to the upper abdomen and lower chest may produce hemodynamic instability because of intrathoracic hemorrhage, pneumothorax, or pericardial tamponade.
2. Peritoneal signs. There is considerable debate over the reliability of peritoneal signs, particularly in the early postinjury period. Among physical examination findings, unequivocal peritoneal signs have the highest positive predictive value, whereas an entirely normal examination even in the presence of mild to moderate intoxication has the greatest negative predictive value for therapeutic laparotomy.95,96
3. Evisceration. With isolated omental evisceration, both a selective and a mandatory operating approach have been espoused. Omentum has been successfully ligated, excised, and restored to the peritoneal cavity.94,95 However, patients with viscus or omental evisceration sustain up to an 80% incidence of major intraperitoneal injury, rendering laparotomy a reasonable next step in management.12
4. Left-sided diaphragmatic injury. In contradistinction to blunt mechanisms, penetrating trauma to the diaphragm produces small tears and evanescent clinical clues to their presence. Thus clinical examination and plain chest films are rarely diagnostic of injury. Left-sided tears in the diaphragm can lead to herniation of bowel into the thorax weeks to decades later, leading to obstruction, strangulation, infarction, perforation, and death. For right-sided diaphragmatic injury, the liver affords considerable protection against herniation. Other diagnostic measures, such as DPL or laparoscopy, or a mandatory laparotomy approach are necessary to determine whether the diaphragm has been violated.97
5. Gastrointestinal hemorrhage. Recovery of blood via a nasogastric tube or emesis may reflect a violation of the stomach or duodenum but is an unusual occurrence.80,94,96 Likewise, examination of the rectum or vagina may reveal hemorrhage that is the result of intraperitoneal or retroperitoneal trauma, but there are often external signs of hemorrhage. Care should be taken in performing a vaginal examination in a woman with pelvic fractures to avoid injury to the examiner’s hand.
6. Implements in situ. The conservative and widely held maxim is to remove implements in situ of the torso in the operating room. This is to ensure expeditious control of hemorrhage should the implement reside within a vascular space or highly vascularized organ. Although implements in situ are most safely removed in the operating room, exceptions to this practice exist. These include situations in which emergency department resuscitation is impeded by the presence of the implement or the patient is at high risk of significant morbidity from nontherapeutic laparotomy because of severe comorbid conditions or pregnancy, for example.
7. Intraperitoneal air. The presence of free intraperitoneal air is often not sought because of the insensitivity and nonspecificity of this finding. Free intraperitoneal air can impute communication of the knife with the intraperitoneal space or the presence of pulmonary or mediastinal injury. Therefore it does not necessarily indicate hollow visceral perforation and should not be used in isolation as an indicator for operation.
Step II: Peritoneal Violation.: If clinical indications for laparotomy are absent, a logical next step is assessing the wound tract itself. The presence of peritoneal violation can be determined by a variety of means. There is great value in establishing that a wound tract is superficial to the peritoneal, retroperitoneal, intrathoracic, and pericardial cavities. In this event, the patient can be discharged from the emergency department after receiving appropriate wound care.91,95 If a study is inconclusive, it should be assumed that one or more of these cavities has been violated and further means of assessment are required. The five methods of assessing the intactness of the peritoneum are as follows:
1. Evisceration. Evisceration of bowel or omentum is clear evidence of peritoneal entry. These situations are usually handled by mandatory laparotomy. In certain centers, however, these eviscerations are reduced in the emergency department and further diagnostics pursued.61,96
2. Intraperitoneal air. A finding of intraperitoneal free air on an upright chest or a lateral decubitus abdominal radiograph generally establishes that the knife has entered the peritoneal cavity and drawn air in with it, has disrupted a hollow viscus, or both. Rarely, a false-positive determination of peritoneal entry can be made when the actual source of intraperitoneal free air is the pulmonary tract.
3. LWE. This has been demonstrated to be an effective tool in determining the depth of the stab wound tract.
4. Ultrasonography. Ultrasonography demonstrating hemoperitoneum, pneumoperitoneum, or pericardial effusion identifies peritoneal penetration or cardiac injury.98 However, its reliability as a sole indicator for injury is not as dependable as that in BAT, and it carries a 15% negative laparotomy rate when used as such. In addition, a negative FAST does not rule out peritoneal violation.99 Ultrasonography may also be used as an adjuvant to LWE to determine intactness of fascia. Although a small study demonstrated that it can positively rule in fascial penetration, it is unreliable to rule this out.81 Experience with ultrasonography for this purpose has been successful but very limited.
5. Laparoscopy. This has compared favorably with LWE in assessing the wound tract but requires far more expertise and carries a far greater risk of complications. It is the most invasive and costly means of evaluating the integrity of the peritoneum. However, laparoscopy may also discover and serve as the mode of repair of certain diaphragmatic or organ injuries or both,12,83,84 and some postulate that its use in experienced centers actually decreases length of stay and therefore cost.94
Step III: Injury Requiring Laparotomy.: In this algorithm, patients requiring an operation on clinical grounds have proceeded to laparotomy, and those in whom peritoneal, retroperitoneal, intrathoracic, and pericardial cavity violations have been excluded are discharged home. The patients remaining have presumed or known peritoneal violation. The next consideration is whether injury exists that dictates operative repair, because organ injury is present in only just over 60% of patients with peritoneal violation.4,92 In any case, patients who reach this stage of evaluation should be observed for at least 12 to 24 hours.75
Historically, the diagnostic standard to address the issue of intraperitoneal injury was DPL. Its role was especially valuable as a rapid means of determining hemoperitoneum in the patient in critical condition and for the discovery of occult hollow viscus perforation and isolated diaphragmatic injury.97,100 However, it is invasive, and thus the vast majority of centers advocate other, less invasive adjuvant testing coupled with serial physical examinations as the next step in management.
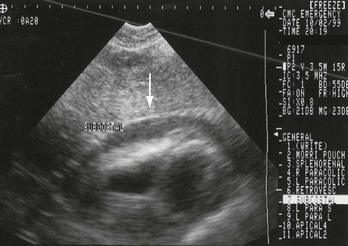
Ultrasonography may be somewhat less accurate than DPL in establishing the presence or absence of hemoperitoneum, but it can simultaneously ascertain hemopericardium (Fig. 46-10). In most centers ultrasonography can be accomplished as quickly or more quickly than peritoneal aspiration. Emphasis on serial examinations with selective use of other studies on an as-needed basis can be successful when an adequate number of experienced clinicians are available.98,101,102
CT has been particularly useful for potential colorectal trauma or further assessment of patients submitted to serial examination alone. However, some centers routinely perform CT in these cases and not simply for possible colorectal trauma.103 Most use triple contrast (oral, rectal, and intravenous), although some newer studies cite equal accuracy with intravenous contrast only.104 Hollow viscus and occult diaphragmatic injuries remain the most frequently missed injuries on CT (even with use of triple contrast), although with the advent of multidetector CT scanners this is decreasing.11,83
Laparoscopy works best in experienced hands for restricted indications. However, its routine use is gaining favor in some institutions. Benefits include the ability to detect organ injury (including diaphragmatic injury) and simultaneously repair some injuries, thus decreasing negative and nontherapeutic laparotomy rates.11,81,84
Thoracoabdominal.: Even a single stab wound to the low chest can violate the mediastinum, thoracic cavity, diaphragm, peritoneal cavity, and retroperitoneum. The risk of diaphragmatic penetration from a left thoracoabdominal stab wound has been measured at 17%.12 When all thoracoabdominal wounds are considered, the risk of occult injury is 7%.105 Ultrasonography can be extremely useful by permitting quick assessment for hemopericardium and hemoperitoneum in the marginally stable patient, if thoracotomy or laparotomy is not already clinically indicated.75 LWE of slash-type wounds may obviate the need for further evaluation. However, the depth of investigation cannot be taken beyond the anterior rib margin to maximize safety and accuracy. Further assessment for intraperitoneal and diaphragmatic injury can be made by DPL. The RBC criterion is lowered to 5000 to 10,000/mm3 to optimize sensitivity for isolated diaphragmatic injury.104 Laparoscopy or thoracoscopy can visualize and potentially be used to repair the diaphragm and other organs. Newer multidetector CT scanning and MRI show promise in excluding diaphragmatic injury. CT has a sensitivity of 94% and specificity of almost 96% for detecting diaphragmatic injury. However, equivocal scans should be followed up with more definitive management, such as DPL, exploratory laparotomy, or laparoscopy.13 A very conservative approach to the left lower chest stab wound, in particular, is mandatory exploration. This approach avoids any opportunity for missed diaphragmatic rents and their delayed consequences but results in an exceptionally high incidence of nontherapeutic operation. Rapid slice helical CT and MRI may provide a solution to this vexing concern, but data are limited to date.
Flank and Back.: The incidence of retroperitoneal injuries after stab wounds to the flank and back is greater than with injury to the anterior wall. However, risk of intraperitoneal organ injury is significant, ranging from 15 to 40%.14 Again, LWE can be a useful first step. However, the paraspinal muscles are quite thick, rendering the procedure more difficult. Triple-contrast CT scan is becoming the preferred method of evaluation in hemodynamically stable patients and coupled with observation may safely allow nonoperative management of these patients.32,97
Implement in Situ.: It is routinely advised that foreign bodies in situ of the torso be removed under operating conditions. This is considered safest in the event that the implement is intravascular or in a highly vascularized organ. Plain films are generally all that is required. A CT scan may be indicated in stable patients if plain films suggest impalement of major vascular structures. Angiography may also be necessary. For pregnant patients or those with severe comorbid illness in whom unnecessary laparotomy is preferably avoided, a CT scan may be able to discern the depth of entry and extent of injury, though the risk of radiation to the fetus must be weighed against the risk of operative intervention. In these cases the foreign body may be removed safely outside of the operating room.
Penetrating Abdominal Trauma: Gunshot Wounds
Management
Abdominal GSWs enter the peritoneal cavity in approximately 80% of cases, and in more than 90% of those involving penetration, there is intraperitoneal damage.30 These statistics significantly exceed the figures for stab wounds, and most trauma surgeons adjust their management to a conservative bent accordingly. We promote the principle that although selective management is widely accepted for stab wounds, its application in the management of GSWs is more limited, and therefore conservative clinical criteria for mandatory laparotomy should be applied. Other authors argue, however, that although peritoneal penetration and intraperitoneal injury are far more likely to result from GSWs, damage requiring operative repair should be the instrumental concern, and this may be less common than previously stated. More recent series report intra-abdominal injury in only 70 to 80% of cases, supporting the contention that nonoperative management could be appropriate for a substantial percentage of patients.3,30,103
A prudent approach to GSWs to the abdomen can follow the same sequential three-step algorithm as for stab wounds (Fig. 46-11). First and foremost, are there clinical grounds for operation? Second, if none exists, has peritoneal violation occurred? Third, does injury requiring laparotomy exist? Centers that adhere to the tenet that known or suspected peritoneal violation imputes high likelihood of intraperitoneal injury will proceed to laparotomy if the second question is answered affirmatively. Those in which it is believed that there is a lower incidence of significant organ damage use other diagnostic agents, including serial physical examination, irrespective of whether the peritoneal cavity has been violated.
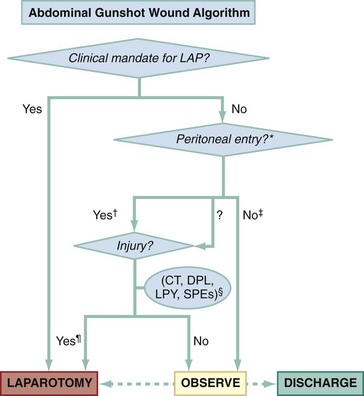
Figure 46-11 Abdominal gunshot wound algorithm. LAP, laparotomy.
*Can be assessed by missile path, plain films, local wound exploration, ultrasonography, and laparoscopy.
†Most centers proceed to laparotomy if peritoneal entry is suspected.
‡Patients with documented superficial and low-velocity injuries can be discharged; unknown-depth or high-velocity injuries require further tests or observation.
§Computed tomography (CT), diagnostic peritoneal lavage (DPL), laparoscopy (LPY), or serial physical examinations (SPEs) can be used in singular or complementary fashion, depending on the clinical scenario.
¶Expectant management of injuries caused by gunshot wounds is rarely attempted.
Step I: Clinical Indications for Laparotomy.: These clinical demands are similar to those proposed for stab wounds (see Table 46-3).
Step II: Peritoneal Violation.: Six methods are used to determine whether the missile has entered or traversed the peritoneal cavity. This question is most germane for centers that perform laparotomy based on peritoneal violation alone.
1. Missile path. Clear entrance and exit wounds allow for a reasonably reliable estimate of the missile path. However, many GSWs ricochet. Even a single GSW can ricochet, and the tendency of low-velocity missiles to follow fascial planes of lower resistance can render this approach misleading.
2. Plain radiographs. An anteroposterior and lateral projection of the abdomen can assist in placing the missile in the peritoneal cavity, but such estimations are imprecise and are largely unhelpful in patients with through-and-through or multiple GSWs.
3. LWE. Because GSWs produce considerably more tissue damage than stab wounds, LWE is a less useful tool for GSWs of the abdomen, flank, and back. Its role should likely be restricted to low-velocity projectiles with suspected superficial entry. Because of the much greater technical difficulty and hazard in visualizing these extensive missile tracts, there is a tendency to underestimate the degree of damage.30
4. Ultrasonography. The experience with ultrasonography in coincidentally assessing wound tracts and the mediastinum for low chest and upper abdominal penetration has been successful but very limited.
5. Laparoscopy. Laparoscopy is the most invasive and costly means of evaluating the integrity of the peritoneum. However, it may also discover and serve as the mode for repair of certain diaphragmatic or organ injuries or both.82,84,102
6. CT. CT has been helpful when trajectory is indeterminate and has shown a sensitivity and specificity of 90.5% and 96%, respectively, for identifying intra-abdominal injury. It can also identify the wound track and indicate vascular structures at risk for injury, although this is more useful in neck wounds.30,103
Step III: Injury Requiring Laparotomy.: In most institutions, the algorithm terminates after the second step, in which determination or strong suspicion of peritoneal violation presupposes the need for laparotomy. At more liberal centers, these facts are deemed insufficient, and additional diagnostics are undertaken.
1. Serial examinations. Patients with normal examination findings or localized wound tenderness can be observed only if clinical circumstances and institutional policy allow. Physical examination may be more reliable than previously suspected in the presence of alcohol or illicit drug intoxication.75
2. DPL. DPL has been highly successful in determining or excluding intraperitoneal injury. When DPL is used, all criteria for positivity remain the same with the exception of the RBC count, which is lowered to 5000 to 10,000 RBCs/mm3 to maximize sensitivity.30,103
3. CT. Higher-resolution scanners may augment the ability of CT to identify hollow visceral damage in addition to solid organ and vascular pathologic lesions.30
4. Laparoscopy. The greatest use for laparoscopy is in the evaluation of the diaphragm in patients with left thoracoabdominal GSWs who do not have indications for standard operative intervention.89
Thoracoabdominal.: Patients with GSWs to the low chest have intraperitoneal injuries reported in 45% of cases. Clinical indications for laparotomy are unchanged. DPL is particularly helpful in these cases to discern diaphragm injury, and the RBC threshold of 5000 to 10,000/mm3 produces excellent sensitivity, but a combination of CT scanning and serial examinations is more commonly used.
Flank and Back.: In the past, operative exploration was generally recommended because of the increased likelihood of a serious injury and the greater fallibility of both the physical examination and DPL in cases of retroperitoneal injuries. However, as multidetector CT scanners have evolved, an intravenous contrast CT scan to delineate retroperitoneal pathologic lesions is typically the initial diagnostic test of choice in a stable patient.95,102 As with stab wounds, laparoscopy or observation alone can be attempted in selected circumstances.106
Shotgun Wounds.: Type I injuries can be effectively managed by reserving laparotomy for patients with clear peritoneal signs or progressive abdominal tenderness. Certain authors advocate an expectant approach to type II injuries, stating that small punctures of the bowel cause no wound eversion and no peritoneal leakage and will spontaneously close.107 A more prudent approach is to perform laparotomy in cases of these penetrating wounds, especially if there are signs of peritonitis. Reconstruction of abdominal wall defects may be required. Type III injuries are commonly associated with multiple organ injuries, shock, and pronounced tissue destruction, requiring hemostasis and extensive débridement.
Blunt Abdominal Trauma
Most centers assimilate physical examination, bedside ultrasonography, CT, and, in rare instances, DPL into a clinical algorithm.25 Other tests, such as angiography, may be indicated. To reiterate, a clinical assessment of an alert patient that depends on abdominal findings alone is reasonably accurate but is accompanied by both false-positive and false-negative errors.67,108–110 Such an assessment is more hazardous for a patient who is under the influence of a variety of toxins or whose examination is compromised by a head injury, spinal injury, or difficulty in communication resulting from developmental delay, psychiatric illness, a language barrier, or age.
The purpose of diagnostic studies in patients with BAT is twofold (Table 46-4): to discern or eliminate the presence of hemoperitoneum in the patient whose condition is critical and unstable to properly sequence management and, in less urgent circumstances, to demonstrate organ injury that requires operative repair.
Table 46-4
Diagnostic Studies in Blunt Abdominal Trauma
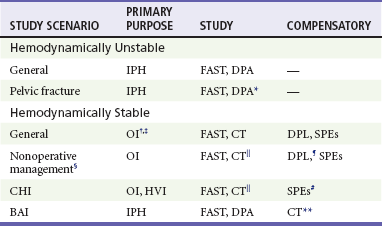
*Positive peritoneal aspirate necessitates laparotomy, positive red blood cell count only, and warrants attention to pelvic fracture.
†To discover fluid or blood suggesting injury.
‡FAST for OI much less reliable than for IPH.
§Institutional capability should be carefully considered.
 CT less reliable for HVI than for solid visceral injury.
CT less reliable for HVI than for solid visceral injury.
¶Complementary to CT if HVI suspected.
#SPEs are unreliable in the patient with CHI.
**May be more appropriate if helical CT is primary study for blunt abdominal injury or can be rapidly acquired.
FAST Ultrasonography.: The FAST examination has a safety advantage in that it can be performed rapidly and conducted in the resuscitation suite in the emergency department. In contradistinction to DPL, the FAST is hazard-free, and serial examinations can be undertaken with ease in any patient. In hypotensive patients the FAST has excellent sensitivity for hemoperitoneum requiring surgical intervention, and most centers proceed to exploratory laparotomy in these patients.107,111 However, in those with a negative FAST, intra-abdominal injury requiring operative repair cannot be excluded.112,113
Diagnostic Peritoneal Lavage.: DPL is exceptionally sensitive in discovering hemoperitoneum, with a false-negative rate of less than 2%. This procedure can be performed in virtually any patient by varying the site and technical method. Aspiration of the peritoneum generally requires less than 5 minutes. Given advances in other diagnostic modalities, however, its role is now predominantly at centers without access to ultrasound in hemodynamically unstable patients.
Computed Tomography.: Although a CT scan can both visualize and estimate the quantity of hemoperitoneum, the time required to accomplish the procedure, including transport of the patient and setup, can be problematic, depending in part on the location of the scanner. Moreover, the ability to carry out CT scanning in a safe manner depends on the availability and expertise of personnel to monitor the patient while he or she is in the CT scanner.
Demonstrating Organ Injury That Requires Laparotomy.: Indications for the respective studies will vary with clinical need and with the experience, resources, and attitudes of individual institutions.
Ultrasonography and Diagnostic Peritoneal Lavage.: Prompt FAST (or, less commonly, DPL) is clearly warranted in the acutely injured and unstable patient with multiple trauma.
Computed Tomography.: A CT scan alone is sufficient and appropriate in the patient who is hemodynamically stable and has no obfuscating clinical factors. The great advantage of the CT scan is its ability to distinguish intraperitoneal organ injury and simultaneously evaluate the retroperitoneum. It is the most capable instrument in diagnosing liver and spleen pathologic lesions, and it allows visualization and semiquantitation of hemoperitoneum.
Management
In cases of blunt trauma, it is the exception when a patient undergoes laparotomy based on clinical grounds alone. Far more typically, one or a complementary battery of diagnostic tests are performed. The choice of these tests is influenced by the patient’s hemodynamic status, the clinical scenario, and the institution’s resources and preferences (Fig. 46-12).
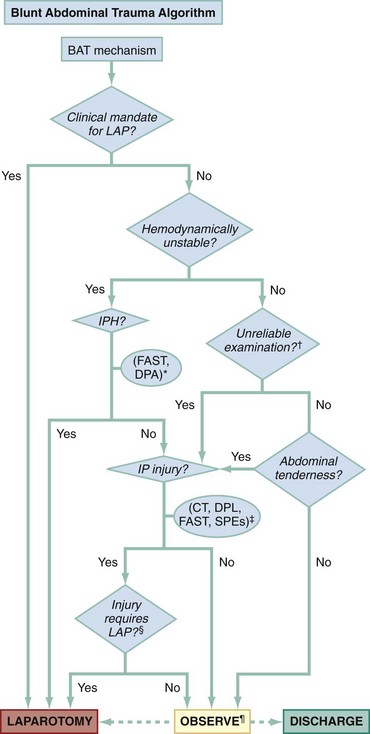
Figure 46-12 Blunt abdominal trauma (BAT) algorithm. CT, computed tomography; DPL, diagnostic peritoneal lavage; FAST, focused assessment with sonography in trauma; IP, intraperitoneal; IPH, intraperitoneal hemorrhage; LAP, laparotomy; SPEs, serial physical examinations.
*Determined by unequivocal free intraperitoneal fluid on FAST or positive aspiration of blood on diagnostic peritoneal aspiration (DPA).
†Can be unreliable because of closed head injury, intoxicants, distracting injury, or spinal cord injury.
‡One or more studies may be indicated.
§Need for laparotomy is based on clinical scenario, diagnostic studies, and institutional resources.
¶Duration of observation should be 6 to 24 hours depending on whether diagnostic tests have been performed, the results of the tests, and clinical circumstances, including the absence of factors rendering the examination unreliable.
Clinical Indications for Laparotomy.: The decision to perform immediate laparotomy after injury from a blunt mechanism is rarely determined solely by clinical parameters. Potential indications are any of the following (Table 46-5):
Table 46-5
Clinical Indications for Laparotomy after Blunt Trauma
| MANIFESTATION | PITFALL |
| Unstable vital signs with strongly suspected abdominal injury | Alternate sources of shock |
| Unequivocal peritoneal irritation | Potentially unreliable |
| Pneumoperitoneum | Insensitive; may be caused by cardiopulmonary source or invasive procedures (diagnostic peritoneal lavage, laparoscopy) |
| Evidence of diaphragmatic injury | Nonspecific and insensitive, especially in penetrating trauma |
| Significant gastrointestinal bleeding | Uncommon, unknown accuracy |
1. Unexplained signs of blood loss or hypotension in a patient who cannot be stabilized and in whom intra-abdominal injury is very strongly suspected
2. Clear and persistent signs of peritoneal irritation
3. Radiologic evidence of pneumoperitoneum consistent with a viscus rupture
4. Evidence of a diaphragmatic rupture
5. Persistent, significant gastrointestinal bleeding seen in the nasogastric return or in vomitus
Hemodynamically Unstable Patients.: In the patient with multiple blunt injuries who is threatened by shock, three cavities are immediately targeted. Chest and pelvic radiographs seek blood loss in the thoracic and retroperitoneal spaces, respectively. FAST or peritoneal aspiration is undertaken to reveal or exclude the presence of blood in the peritoneal cavity. Hemoperitoneum in a clinically unstable patient necessitates laparotomy.
Hemodynamically Stable Patients.: In patients who are hemodynamically stable, CT scanning is the widely preferred diagnostic modality because of its ability to specify organ pathology, semiquantitate hemoperitoneum, and study nonabdominal body regions. Its potential drawbacks in certain clinical circumstances must be understood, however. Ultrasonography, DPL, and, very uncommonly, laparoscopy can be used in a complementary or primary mode.
Operative versus Nonoperative Management.: Patientswith certain intraperitoneal injuries can be watched expectantly and need not be subjected to laparotomy. Specifically, this has been successful with even moderate- to high-grade liver or spleen trauma. Failures, including deaths, have occurred with this approach. Thus, although it is preferable to avoid unnecessary laparotomy, it is imperative to prevent significant morbidity or mortality by waiting too long. The patient with normal sensorium and minor to intermediate severity of mechanism is a superior candidate for expectant management. It is critical that an institution appraise its ability to manage such patients. This includes having experienced nursing staff, trauma surgeons, adequate blood resources, and radiologists and the ability to take a patient to undergo laparotomy urgently if the need arises.
Several pitfalls in the expectant approach are noteworthy. First, multiple injuries of intraperitoneal organs, including hollow viscera, are common.72 Operative management of hollow visceral injury is necessary, and delay can have severe consequences.114 The ability of the CT scan to detect coincident injury to these structures is discussed earlier. The patient with multisystem injury and, specifically, closed head trauma is most vulnerable to having delayed diagnosis of perforated intestinal injury.72,74 Second, expectant management may lead to increased use of blood products. Finally, this management approach will fail in those patients whose hemorrhage is not amenable to therapeutic angiography and embolization and will not abate because of misperceived injury of solid organs. In such cases, the lag time from injury to operation may increase morbidity and mortality.115
Pelvic Fracture.: In the setting of pelvic fracture, the clinical triage determinant is the presence or absence of hemoperitoneum (Fig. 46-13). Although the sensitivity of FAST in patients with pelvic fractures is decreased, it still serves as a tool to triage the patient to the next intervention. In an unstable patient, a negative FAST is followed by a supraumbilical peritoneal aspirate, to avoid potential false positives caused by retroperitoneal blood moving to the anterior infraumbilical space. If this reveals 10 mL or more of blood, then the patient should expeditiously be moved to laparotomy. If instead urine or other fluid is aspirated, then the patient should undergo pelvic angiography before laparotomy. If the FAST is negative, then the patient should proceed to therapeutic angiography with the presumed diagnosis of a life-threatening retroperitoneal bleed. In stable patients, early mechanical pelvic stabilization is advised (see Chapter 55), and CT scan followed by pelvic angiography and embolization are undertaken as early as possible in the context of the multiple injuries.
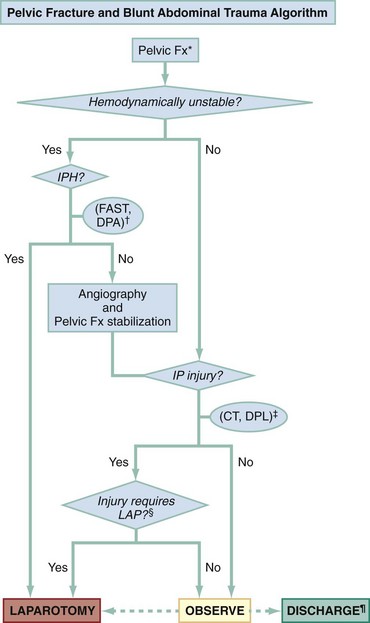
Figure 46-13 Pelvic fracture (Fx) and blunt abdominal trauma algorithm. CT, computed tomography; DPL, diagnostic peritoneal lavage; FAST, focused assessment with sonography in trauma; IP, intraperitoneal; IPH, intraperitoneal hemorrhage; LAP, laparotomy.
*Certain pelvic fractures are more likely to cause pelvic vascular disruption and subsequent retroperitoneal hemorrhage.
†Determined by unequivocal free intraperitoneal fluid on focused assessment with sonography in trauma (FAST) or positive peritoneal aspiration on diagnostic peritoneal aspiration (DPA).
‡One or more studies may be indicated. Serial physical examinations are generally considered unreliable owing to the presence of pelvic fracture.
§Need for laparotomy is based on clinical scenario, diagnostic studies, and institutional resources.
¶Discharge from the perspective of need for further consideration for laparotomy.
Multiple System Injury.: Management of the abdominal trauma patient with more than one life-threatening injury cannot be dogmatic. It is not unusual to confront intraperitoneal hemorrhage in a patient with apparent closed head injury or suspected blunt aortic disruption or both. Repair of the abdomen is said to take precedence over that of the head and chest. However, these situations are highly complex, and decision-making is influenced by numerous and dynamic variables. The key tenet is that a patient with known hemoperitoneum whose vital signs cannot be stabilized should undergo laparotomy or face imminent exsanguination.
Closed head Injury.: In general, patients with coincident severe closed head injury but without frank coma or lateralizing signs do not have intracranial lesions that require craniotomy. When lateralizing features do exist, the clinician must choose between a rapid prelaparotomy CT scan of the head or preemptive burr holes at laparotomy. This judgment rests mostly on the clinical state of the patient with particular regard to his or her response to resuscitative measures and the timely availability of CT.116 An approach to this scenario is presented in Figure 46-14.
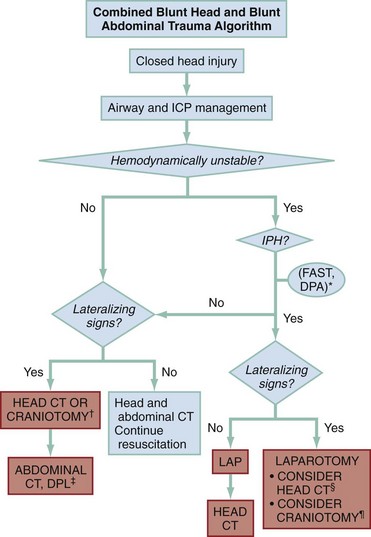
Figure 46-14 Combined blunt head and blunt abdominal trauma algorithm. CT, computed tomography; ICP, intracranial pressure; IPH, intraperitoneal hemorrhage.
*Determined by unequivocal free intraperitoneal fluid on focused assessment with sonography in trauma (FAST) or positive peritoneal aspiration on diagnostic peritoneal aspiration (DPA).
†Craniotomy or burr holes based on clinical picture and unavailability of computed tomography (CT).
‡Diagnostic peritoneal lavage (DPL) can be complementary to CT in determining hollow viscus injury.
§Consider prelaparotomy (LAP) head CT based on clinical picture and availability of CT.
¶Consider craniotomy or burr holes simultaneous with laparotomy.
Blunt Aortic Injury.: Clinical or radiographic features that portend great vessel injury, notably a widened mediastinum on a supine anteroposterior chest radiograph, have variable sensitivity and specificity. In addition, although the course of any single aortic lesion is unpredictable, there is more likely than not a lag of at least several hours before rupture. Therefore exigent laparotomy should precede great vessel diagnostics. Should the patient’s condition precipitously deteriorate, left lateral thoracotomy allows aortic cross-clamp with its circulatory benefits and, in general, affords access to the injured portion of the vessel (Fig. 46-15).
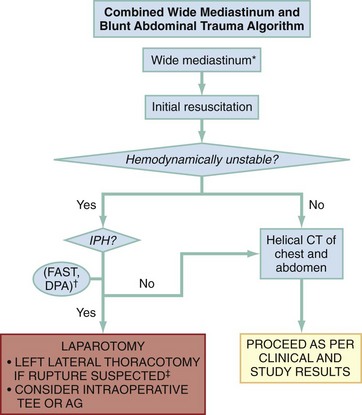
Figure 46-15 Combined wide mediastinum and blunt abdominal trauma algorithm. AG, aortogram; CT, computed tomography; FAST, focused assessment with sonography in trauma; IPH, intraperitoneal hemorrhage; TEE, transesophageal echocardiogram.
*Preferably based on upright posteroanterior film and mechanism of injury; other radiographic signs or mechanism alone may signal need for evaluation.
†Determined by unequivocal free intraperitoneal fluid on FAST or positive finding on diagnostic peritoneal aspiration (DPA).
‡Allows surgical access to majority of aortic disruption sites.
Pediatrics.: Children are prone to aerophagia, and decompressive nasogastric tubes are particularly important to help prevent compromised lung function and aid in the abdominal examination. Care is taken in fluid resuscitation and drug administration, with attention being paid to the patient’s size and with surface area or body weight used as a guide. Because of their size and relatively larger surface area, children are more susceptible to hypothermia resulting from the administration of unwarmed fluids and blood products. The use of overhead heat lamps, blood warmers, and prewarmed intravenous fluids helps obviate this condition.
For physiologic reasons, the expectant management of blunt hepatic or splenic injury has better success in the child than in the adult patient.117–119 If stability exists, nonoperative management can ensue if capable personnel and resources are present.120 CT scanning is the primary diagnostic agent in both the initial and the convalescent periods to define and grade solid organ injury. As for adults, this modality is insensitive for the discovery of hollow viscus and, to a lesser degree, pancreatic pathologic conditions.71
FAST has been found to be useful for the detection of free fluid and can be used in triage to send the unstable child with visualized hemoperitoneum for laparotomy.121 However, FAST appears to have less sensitivity when compared with the adult experience. DPL, specifically peritoneal aspiration, can also uncover hemoperitoneum in the initial management of the critically, multiply injured child. Reliance on cell count alone has prompted significant nontherapeutic laparotomy rates.
References
1. Lawson, CM, Daley, BJ, Ormsby, CB, Enderson, B. Missed injuries in the era of the trauma scan. J Trauma. 2011;70:452.
2. Shaftan, GW. Indications for operation in abdominal trauma. Am J Surg. 1960;99:657.
3. Velmahos, GC, et al. Selective nonoperative management in 1,856 patients with abdominal gunshot wounds: Should routine laparotomy still be the standard of care? Ann Emerg Med. 2001;234:395.
4. Biffl, W, Moore, EE. Management guidelines for penetrating abdominal trauma. Curr Opin Crit Care. 2010;16:609.
5. Nicholas, JM, et al. Changing patterns in the management of penetrating abdominal trauma: The more things change, the more they stay the same. J Trauma. 2003;55:1095.
6. Bernard, SJ, Paulozzi, LJ, Wallace, DL, Centers for Disease Control and Prevention (CDC). Fatal injuries among children by race and ethnicity—United States, 1999-2002. MMWR Surveill Summ. 2007;56:1.
7. Hepburn, L, Miller, M, Azrael, D, Hemenway, D. The U.S. gun stock: Results from the 2004 national firearms survey. Inj Prev. 2007;13:15.
8. Centers for Disease Control and Prevention (CDC). About Compressed Mortality, 1999-2007. http://wonder.cdc.gov/cmf-icd10.html.
9. Demetriades, D, et al. High-level falls: Type and severity of injuries and survival outcome according to age. J Trauma. 2005;58:342.
10. Nance ML, ed. National Trauma Data Bank 2011: Pediatric Report. American College of Surgeons: 2011. www.facs.org/trauma/ntdb/pdf/ntdbpediatricreport2011.pdf.
11. Friese, RS, Coln, E, Gentilello, LM. Laparoscopy is sufficient to exclude occult diaphragm injury after penetrating abdominal wounds. J Trauma. 2005;58:789.
12. Leppäniemi, A, Haapiainen, R. Occult diaphragmatic injuries caused by stab wounds. J Trauma. 2003;55:646.
13. McCarthy, MC, Lowdermilk, GA, Canal, DF, Broadie, TA. Prediction of injury caused by penetrating wounds to the abdomen, flank and back. Arch Surg. 1991;128:926.
14. Boyle, EM, Jr., et al. Diagnosis of injuries after stab wounds to the back and flank. J Trauma. 1997;42:260.
15. DeMuth, WE, Jr. Bullet velocity and design as determinants of wounding capability: An experimental study. J Trauma. 1966;6:222.
16. Velitchkov, NG, et al. Delayed small bowel injury as a result of penetrating extraperitoneal high-velocity ballistic trauma to the abdomen. J Trauma. 2000;48:169.
17. Cairns, BA, et al. Management and outcome of abdominal shotgun wounds trauma score and the role of exploratory laparotomy. Ann Surg. 1995;221:272.
18. Rivara, FP, Koepsell, TD, Grossman, DC, Mock, C. Effectiveness of automatic shoulder belt systems in motor vehicle crashes. JAMA. 2000;283:2826.
19. Velmahos, GC, Tatevossian, R, Demetriades, D. The “seat belt mark” sign: A call for increased vigilance among physicians treating victims of motor vehicle accidents. Am Surg. 1999;65:181.
20. Prince, JS, LoSasso, BE, Senac, MO, Jr. Unusual seat-belt injuries in children. J Trauma. 2004;56:420.
21. Spoormans, I, Van Hoorenbeeck, K, Balliu, L, Jorens, PG. Gastric perforation after cardiopulmonary resuscitation: Review of the literature. Resuscitation. 2010;81:272.
22. Ko, CW, Dominitz, JA. Complications of colonoscopy: Magnitude and management. Gastrointest Endosc Clin N Am. 2010;20:659.
23. Lin, BC, et al. Management of blunt major pancreatic injury. J Trauma. 2004;56:774.
24. Mahoney, EJ, Biffl, WL, Harrington, DT, Cioffi, WG. Isolated brain injury as a cause of hypotension in the blunt trauma patient. J Trauma. 2003;55:1065.
25. Brown, CK, Dunn, KA, Wilson, K. Diagnostic evaluation of patients with blunt abdominal trauma: A decision analysis. Acad Emerg Med. 2000;7:385.
26. Gonzalez, RP, Dziurzynski, K, Maunu, M. Emergent extra-abdominal trauma surgery: Is abdominal screening necessary? J Trauma. 2000;49:195.
27. Shlamovitz, GZ, et al. Poor test characteristics for the digital rectal examination in trauma patients. Ann Emerg Med. 2007;50:25.
28. Esposito, TJ, et al. Reasons to omit digital rectal exam in trauma patients: No fingers, no rectum, no useful additional information. J Trauma. 2005;59:1314.
29. Ball, CG, et al. Traumatic urethral injuries: Does the digital rectal examination really help us? Injury. 2009;40:984.
30. Pryor, JP, Reilly, PM, Dabrowski, GP, Grossman, MD, Schwab, CW. Nonoperative management of abdominal gunshot wounds. Ann Emerg Med. 2004;43:344.
31. Thal, ER. Evaluation of peritoneal lavage and local exploration in lower chest and abdominal stab wounds. J Trauma. 1977;17:642.
32. Moore, EE, Marx, JA. Penetrating abdominal wounds. Rationale for exploratory laparotomy. JAMA. 1985;253:2705.
33. Asimos, AW, et al. Value of point-of-care blood testing in emergent trauma management. J Trauma. 2000;48:1101.
34. Moore, FD. The effects of hemorrhage on body composition. N Engl J Med. 1965;273:567.
35. Herman, R, Guire, KE, Burd, RS, Mooney, DP, Ehlrich, PF. Utility of amylase and lipase as predictors of grade of injury or outcomes in pediatric patients with pancreatic trauma. J Pediatr Surg. 2011;46:923.
36. Holmes, JF, et al. Identification of children with intra-abdominal injuries after blunt trauma. Ann Emerg Med. 2002;39:500.
37. Sola, JE, et al. Pediatric FAST and elevated liver transaminases: An effective screening tool in blunt abdominal trauma. J Surg Res. 2009;157:103.
38. Langdorf, MI, et al. Decision rule and utility of routine urine toxicology screening of trauma patients. Eur J Emerg Med. 2002;9:115.
39. Miller, LA, Shanmuganathan, K. Multidetector CT evaluation of abdominal trauma. Radiol Clin North Am. 2005;43:1079.
40. Haan, JM, et al. Splenic embolization revisited: A multicenter review. J Trauma. 2004;56:542.
41. Hauser, CJ, et al. Prospective Validation of computed tomographic screening of the thoracolumbar spine in trauma. J Trauma. 2003;55:228.
42. Charbit, J, et al. What are the specific computed tomography scan criteria that can predict or exclude the need for renal angioembolization after high-grade renal trauma in a conservation management strategy? J Trauma. 2011;70:1219.
43. Maturen, KE, et al. Contrast-enhanced CT accurately detects hemorrhage in torso trauma: Direct comparison with angiography. J Trauma. 2007;62:740.
44. Lee, SK, Carrillo, EH. Advances and changes in the management of liver injuries. Am Surg. 2007;73:201.
45. Harbrecht, BG, et al. Evaluation of a 15-year experience with splenic injuries in a state trauma system. Surgery. 2007;141:229.
46. Weninger, P, et al. Emergency room management of patients with blunt major trauma: Evaluation of the multislice computed tomography protocol exemplified by an urban trauma center. J Trauma. 2007;62:584.
47. Elton, C, et al. Accuracy of computed tomography in the detection of blunt bowel and mesenteric injuries. Br J Surg. 2005;92:1024.
48. Stuhlfaut, JW, et al. Blunt abdominal trauma: Performance of CT without oral contrast material. Radiology. 2004;233:689.
49. Marx, JA. So what’s a little free fluid? Acad Emerg Med. 2000;7:383.
50. Stuhlfaut, JW, Lucey, BC, Varghese, JC, Soto, JA. Blunt abdominal trauma: Utility of 5-minute delayed CT with a reduced radiation dose. Radiology. 2006;238:473.
51. Brenner, DJ, Hall, EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med. 2007;357:2277.
52. Salottolo, K, et al. Current utilization and radiation dose from computed tomography in patients with trauma. Crit Care Med. 2009;37:1336.
53. Holmes, JF, Wisner, DH, McGahan, JP, Mower, WR, Kuppermann, N. Clinical prediction rules for identifying adults at very low risk for intra-abdominal injuries after blunt trauma. Ann Emerg Med. 2009;54:575.
54. Holmes, JF, et al. Validation of a prediction rule for the identification of children with intra-abdominal injuries after blunt torso trauma. Ann Emerg Med. 2009;54:528.
55. Gupta, R, Greer, SE, Martin, ED. Inefficiencies in a rural trauma system: The burden of repeat imaging in interfacility transfers. J Trauma. 2010;69:253.
56. Cook, SH, Fielding, JR, Phillips, JD. Repeat abdominal computed tomography scans after pediatric blunt abdominal trauma: Missed injuries, extra costs, and unnecessary radiation exposure. J Pediatr Surg. 2010;45:2019.
57. Timaran, CH, Daley, BJ, Enderson, BL. Role of blunt abdominal trauma in the diagnosis of blunt duodenal injury. J Trauma. 2001;51:648.
58. Antoniou, D, Zarifi, M, Gentimi, F, Christopoulos-Geroulanos, G. Sonographic diagnosis and monitoring of an intramural duodenal hematoma following upper endoscopic biopsy in a child. J Clin Ultrasound. 2009;37:534.
59. Raikhlin, A, Baerlocher, MO, Asch, MR, Myers, A. Imaging and transcatheter arterial embolization for traumatic splenic injuries: Review of the literature. Can J Surg. 2008;51:464.
60. Duchesne, JC, Simmons, JD, Schmieg, RE, Jr., McSwain, NE, Jr., Bellows, CF. Proximal splenic angioembolization does not improve outcomes in treating blunt splenic injuries compared with splenectomy: A cohort analysis. J Trauma. 2008;65:1346.
61. Boulanger, BR, Kearney, PA, Tsuei, B, Ochoa, JB. The routine use of sonography in penetrating torso injury is beneficial. J Trauma. 2001;51:320.
62. Dolich, MO, et al. 2576 ultrasounds for blunt abdominal trauma. J Trauma. 2001;50:108.
63. Hyacinthe, AC, et al. Diagnostic accuracy of ultrasonography in the acute assessment of common thoracic lesions after trauma. Chest. 2012;141:1177–1183.
64. Blackbourne, LH, et al. Secondary ultrasound examination increases the sensitivity of the FAST exam in blunt trauma. J Trauma. 2004;57:934.
65. Henderson, SO, Sung, J, Mandavia, D. Serial abdominal ultrasound in the setting of trauma. J Emerg Med. 2000;18:79.
66. Kirkpatrick, AW, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: The extended focused assessment with sonography for trauma (E-FAST). J Trauma. 2004;57:288.
67. Ollerton, JE, et al. Prospective study to evaluate the influence of FAST on trauma patient management. J Trauma. 2006;60:785.
68. Melniker, LA, et al. Randomized controlled clinical trial of point-of-care, limited ultrasonography for trauma in the emergency department: The first sonography outcomes assessment program trial. Ann Emerg Med. 2006;48:227.
69. Lee, BC, Ormsby, EL, McGahan, JP, Melendres, GM, Richards, JR. The utility of sonography for the triage of blunt abdominal trauma patients to exploratory laparotomy. AJR Am J Roentgenol. 2007;188:415.
70. Miller, MT, Pasquale, MD, Bromberg, WJ, Wasser, TE, Cox, J. Not so FAST. J Trauma. 2003;54:52.
71. Goodwin, H, Holmes, JF, Wisner, DH. Abdominal ultrasound examination in pregnant blunt trauma patients. J Trauma. 2001;50:689.
72. Fakhry, SM, Brownstein, M, Watts, DD, Baker, CC, Oller, D. Relatively short diagnostic delays (<8 hours) produce morbidity and mortality in blunt small bowel injury: An analysis of time to operative intervention in 198 patients from a multicenter experience. J Trauma. 2000;48:408.
73. Cha, JY, et al. Diagnostic peritoneal lavage remains a valuable adjunct to modern imaging techniques. J Trauma. 2009;67:330.
74. Williams, MD, Watts, D, Fakhry, S. Colon injury after blunt abdominal trauma: Results of the EAST Multi-Institutional Hollow Viscus Injury Study. J Trauma. 2003;55:906.
75. Nagy, KK, et al. Experience with over 2500 diagnostic peritoneal lavages. Injury. 2000;31:479.
76. Henneman, PL, Marx, JA, Moore, EE, Cantrill, SV, Ammons, LA. Diagnostic peritoneal lavage: Accuracy in predicting necessary laparotomy following blunt and penetrating trauma. J Trauma. 1990;30:1345.
77. Smith, CB, et al. Prediction of blunt traumatic injury in high-acuity patients: Bedside examination vs computed tomography. Am J Emerg Med. 2011;29:1.
78. Thacker, LK, Parks, J, Thal, ER. Diagnostic peritoneal lavage: Is 100,000 RBCs a valid figure for penetrating abdominal trauma? J Trauma. 2007;62:853.
79. Gonzalez, RP, Turk, B, Falimirski, ME, Holevar, MR. Abdominal stab wounds: Diagnostic peritoneal lavage criteria for emergency room discharge. J Trauma. 2001;51:939.
80. Sugrue, M, et al. Guidelines for the management of haemodynamically stable patients with stab wounds to the anterior abdomen. ANZ J Surg. 2007;77:614.
81. Leppäniemi, A, Haapiainen, R. Diagnostic laparoscopy in abdominal stab wounds: A prospective, randomized study. J Trauma. 2003;55:636.
82. Kawahara, NT, Alster, C, Fujimura, I, et al. Standard examination system for laparoscopy in penetrating abdominal trauma. J Trauma. 2009;67:589–595.
83. Simon, RJ, Rabin, J, Kuhls, D. Impact of increased use of laparoscopy on negative laparotomy rates after penetrating trauma. J Trauma. 2002;53:297.
84. Ahmed, N, Whelan, J, Brownlee, J, Chari, V, Chung, R. The contribution of laparoscopy in evaluation of penetrating abdominal wounds. J Am Coll Surg. 2005;201:213.
85. Cotton, BA, et al. Guidelines for prehospital fluid resuscitation in the injured patient. J Trauma. 2009;67:389.
86. Cudnik, MT, Newgard, CD, Sayre, MR, Steinberg, SM. Level I versus Level II trauma centers: An outcomes-based assessment. J Trauma. 2009;66:1321.
87. Luchette, FA, et al. Practice management guidelines for prophylactic antibiotic use in penetrating abdominal trauma: The EAST Practice Management Guidelines Work Group. J Trauma. 2000;48:508.
88. Gilbert, DN, et al. The Sanford Guide to Antimicrobial Therapy. Sperryville, VA: Antimicrobial Therapy Inc.; 2008.
89. Conrad, MF, Patton, JH, Jr., Parikshak, M, Kralovich, KA. Selective management of penetrating truncal injuries: Is emergency department discharge a reasonable goal? Am Surg. 2003;69:266.
90. Plackett, TP, Fleurat, J, Putty, B, Demetriades, D, Plurad, D. Selective nonoperative management of anterior abdominal stab wounds: 1992-2008. J Trauma. 2011;70:408.
91. Mitra, B, Gocentas, R, O’Reilly, G, Cameron, PA, Atkin, C. Management of haemodynamically stable patients with abdominal stab wounds. Emerg Med Australas. 2007;19:269.
92. Alzamel, HA, Cohn, SM. When is it safe to discharge asymptomatic patients with abdominal stab wounds? J Trauma. 2005;58:523.
93. Demetriades, D, et al. Selective nonoperative management of penetrating abdominal solid organ injuries. Ann Surg. 2006;244:620.
94. Leppäniemi, AK, Voutilainen, PE, Haapiainen, RK. Indications for early mandatory laparotomy in abdominal stab wounds. Br J Surg. 1999;86:76.
95. Nagy, K, Roberts, R, Joseph, K, An, G, Barrett, J. Evisceration after abdominal stab wounds: Is laparotomy required? J Trauma. 1999;47:622.
96. Arikan, S, Kocakusak, A, Yucel, AF, Adas, G. A prospective comparison of the selective observation and routine exploration methods for penetrating abdominal stab wounds with organ or omentum evisceration. J Trauma. 2005;58:526.
97. Ertekin, C, Yanar, H, Taviloglu, K, Güloglu, R, Alimoglu, O. Unnecessary laparotomy by using physical examination and different diagnostic modalities for penetrating abdominal stab wounds. Emerg Med J. 2005;22:790.
98. Udobi, KF, Rodriguez, A, Chiu, WC, Scalea, TM. Role of ultrasonography in penetrating abdominal trauma: A prospective clinical study. J Trauma. 2001;50:475.
99. Murphy, JT, Hall, J, Provost, D. Fascial ultrasound for evaluation of anterior abdominal stab wound injury. J Trauma. 2005;59:843.
100. Sriussadaporn, S, et al. Clinical uses of diagnostic peritoneal lavage in stab wounds of the anterior abdomen: A prospective study. Eur J Surg. 2002;168:490.
101. Shanmuganathan, K, et al. Penetrating torso trauma: Triple-contrast helical CT in peritoneal violation and organ injury—a prospective study in 200 patients. Radiology. 2004;231:775.
102. Chiu, WC, Shanmuganathan, K, Mirvis, SE, Scalea, TM. Determining the need for laparotomy in penetrating torso trauma: A prospective study using triple contrast enhanced abdominopelvic computed tomography. J Trauma. 2001;51:860.
103. Velmahos, GC, et al. Abdominal computed tomographic scan for patients with gunshot wounds to the abdomen selected for nonoperative management. J Trauma. 2005;59:1155.
104. Stein, DM, et al. Accuracy of computed tomography (CT) scan in the detection of penetrating diaphragm injury. J Trauma. 2007;63:538.
105. Tayal, VS, Beatty, MA, Marx, JA, Tomaszewski, CA, Thomason, MH. FAST accurate for cardiac and intraperitoneal injury in penetrating chest trauma. Acad Emerg Med. 2000;7:493.
106. Brakenridge, SC, et al. Detection of intra-abdominal injury using diagnostic peritoneal lavage after shotgun wound to abdomen. J Trauma. 2003;54:329.
107. Bode, PJ, Edwards, MJ, Kruit, MC, van Vugt, AB. Sonography in clinical algorithm for early evaluation of 1671 patients with blunt abdominal trauma. AJR Am J Roentgenol. 1999;172:905.
108. Salim, A, et al. Whole body imaging in blunt multisystem trauma patients without obvious signs of injury: Results of a prospective study. Arch Surg. 2006;141:468.
109. Poletti, PA, et al. Blunt abdominal trauma patients: Can organ injury be excluded without performing computed tomography? J Trauma. 2004;57:1072.
110. Gonzalez, RP, Han, M, Turk, B, Luterman, A. Screening for abdominal injury prior to emergent extra-abdominal trauma surgery: A prospective study. J Trauma. 2004;57:739.
111. Farahmand, N, et al. Hypotensive patients with blunt abdominal trauma: Performance of screening US. Radiology. 2005;235:436.
112. Runyon, M, Marx, JA. Peritoneal procedures. In Roberts JR, Hedges JR, eds.: Clinical Procedures in Emergency Medicine, 5th ed, Philadelphia: WB Saunders, 2009.
113. Holmes, JF, Harris, D, Battistella, FD. Performance of abdominal ultrasonography in blunt trauma patients with out of hospital or emergency department hypotension. Ann Emerg Med. 2004;43:354.
114. Rathore, MA, Andrabi, SI, Najfi, SM, Chaudhry, Z, Chaudhry, AM. Injuries to the duodenum—prognosis correlates with body Injury Severity Score: A prospective study. Int J Surg. 2007;5:388.
115. Tayal, VS, et al. Accuracy of trauma ultrasound in major pelvic injury. J Trauma. 2006;61:1453.
116. Nwomeh, BC, et al. Contrast extravasation predicts the need for operative intervention in children with blunt splenic trauma. J Trauma. 2004;56:537.
117. St Peter, SD, Keckler, SJ, Spilde, TL, Holcomb, GW, 3rd., Ostlie, DJ. Justification for an abbreviated protocol in the management of blunt spleen and liver injury in children. J Pediatr Surg. 2008;43:191.
118. Davis, DH, Localio, AR, Stafford, PW, Helfaer, MA, Durbin, DR. Trends in operative management of pediatric splenic injury in a regional trauma system. Pediatrics. 2005;115:89.
119. Eppich, WJ, Zonfrillo, MR. Emergency department evaluation and management of blunt abdominal trauma in children. Curr Opin Pediatr. 2007;19:265.
120. Mattix, KD, et al. Pediatric pancreatic trauma: Predictors of nonoperative management failure and associated outcomes. J Pediatr Surg. 2007;42:340.
121. Weinberg, JA, et al. Trauma laparotomy in a rural setting before transfer to a regional center: Does it save lives? J Trauma. 2003;54:823.