Abdominal Sacral Colpopexy
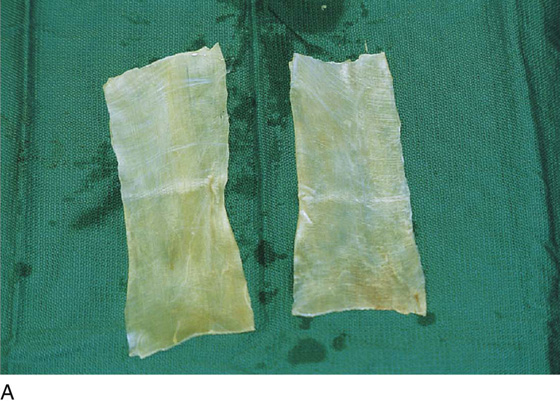
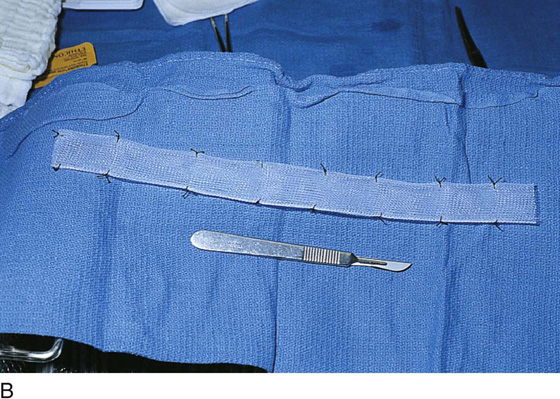
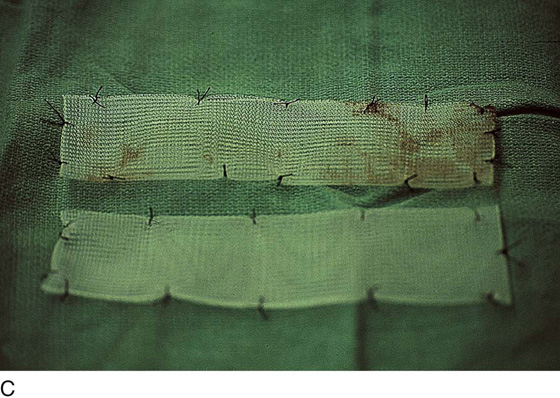
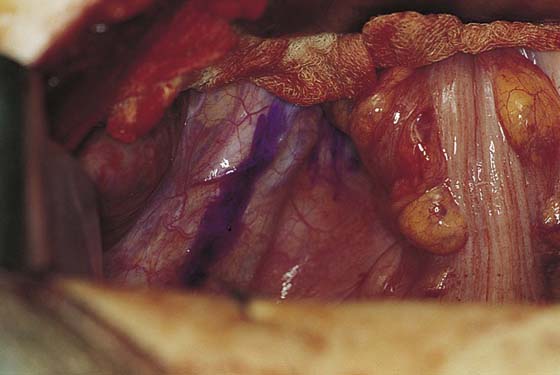
Suspension of the vagina to the sacral promontory by means of an abdominal approach has been shown to be an effective treatment for uterovaginal prolapse and vaginal vault prolapse. Although the exact indications for abdominal sacral colpopexy are controversial, the author prefers it to a vaginal repair when there is obvious failure of the compensatory support mechanisms of the pelvis, especially in the very young patient (Fig. 43–1), or when the vagina has been foreshortened as a result of previous repairs (Fig. 43–2). Many different graft materials have been used for abdominal sacral colpopexy. Natural materials include fascia lata, rectus fascia, and dura mater. Synthetic materials have included polypropylene mesh, polyester fiber mesh, polytetrafluoroethylene mesh, Mersilene mesh, Silastic silicone rubber, and Marlex mesh. Although homologous tissue in the form of cadaveric fascia lata and other xenografts have also been utilized for this operation (Fig. 43–3), at the present time the material of choice is polypropylene. The technique for abdominal sacral colpopexy with graft placement is as follows:
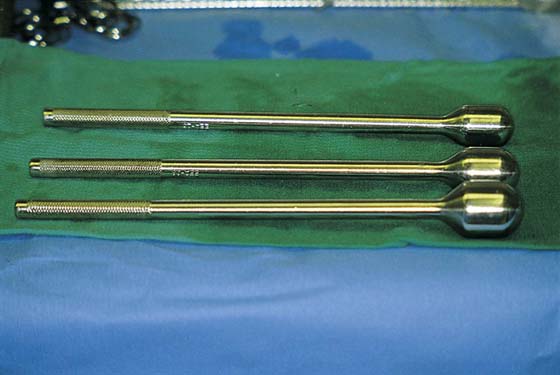
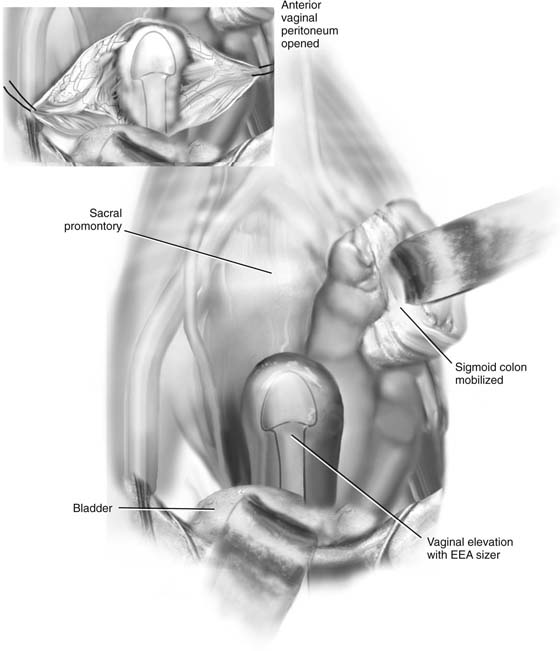
1. The patient should be placed in Allen stirrups or in a frogleg position so that the surgeon has easy access to the vaginal area during the operation. A sponge stick or an EEA (end-to-end anastomosis) sizer (Fig. 43–4) can be placed in the vagina for manipulation of the apex if desired. A Foley catheter with a large (30-mL) balloon is placed in the bladder for drainage. Prophylactic perioperative antibiotics are generally used during this procedure.
2. A laparotomy is performed through a low transverse or midline incision, and the small bowel is packed into the upper abdomen. The sigmoid colon is packed, as much as possible, into the left pelvis. The ureters are identified bilaterally. If the uterus is present, a hysterectomy should be performed and the vaginal cuff closed. The depth of the cul-de-sac and the length of the vagina when completely elevated are estimated.
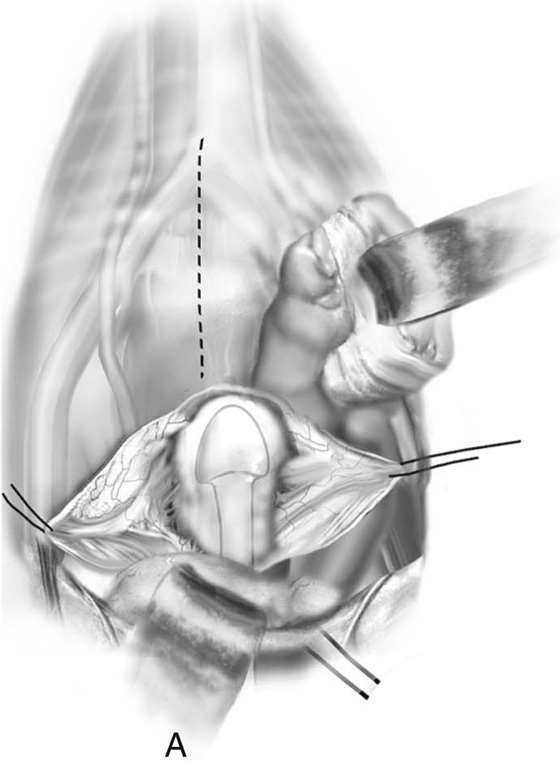
3. While the vagina is elevated cephalad using an EES sizer, the peritoneum over the vaginal apex is incised and the bladder dissected from the anterior vaginal wall (Figs. 43–5 and 43–6). The peritoneum over the posterior vaginal wall is incised into the cul-de-sac, longitudinally along the back of the vaginal wall (see Fig. 43–5). The vaginal apex then is elevated bilaterally with clamps or stay sutures.
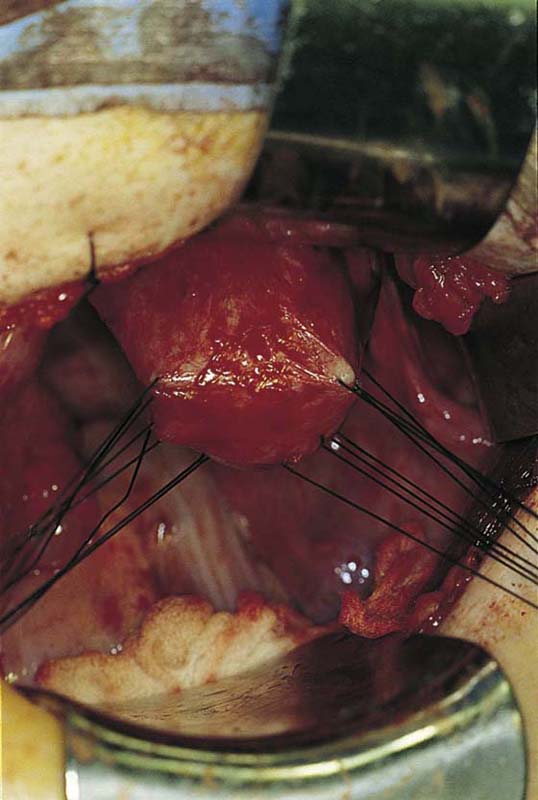
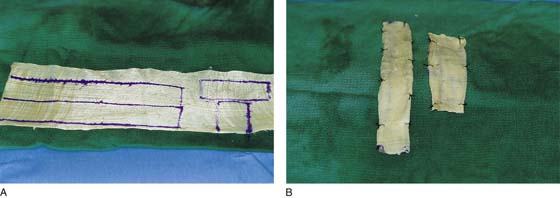
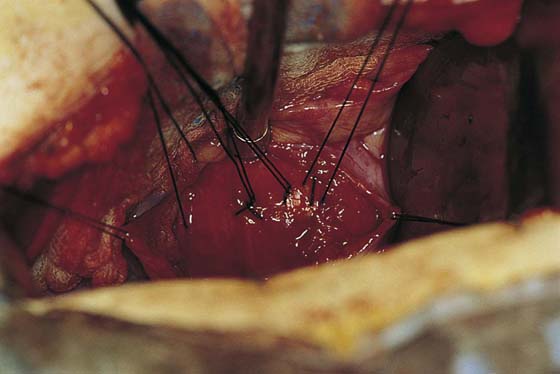
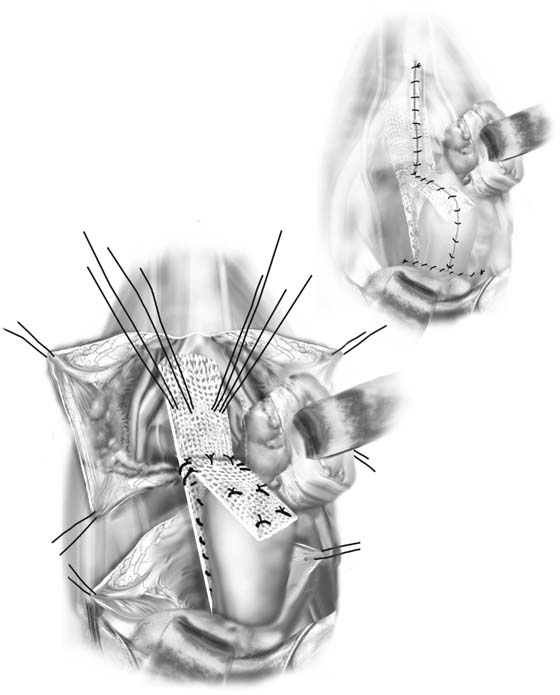
4. As was previously mentioned, many different graft materials have been used, and many different techniques for fixation of the graft to the vagina have been described. The technique we use involves placement of a series of nonabsorbable sutures (usually 0) transversely in the posterior vaginal wall 1 to 2 cm apart (Fig. 43–7). All sutures are placed through the full fibromuscular thickness of the vagina but not in the vaginal epithelium. Biologic or synthetic grafts are prepared as in Figures 43–3 and 43–8. Sutures then are fed through the graft in pairs and tied (Fig. 43–9). The graft should extend at least halfway down the length of the posterior vaginal wall. The author prefers to attach a second piece of mesh or fascia to the upper part of the anterior vaginal wall (Fig. 43–10). This piece of fascia then is sewn to the posterior piece of fascia, which will be attached to the sacrum (see Fig. 43–10), or both pieces are taken back to the sacrum.
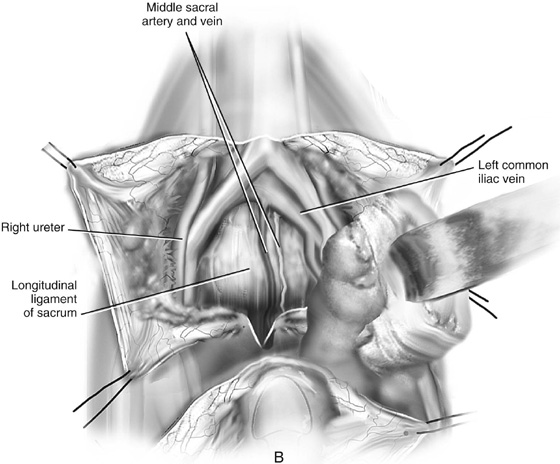
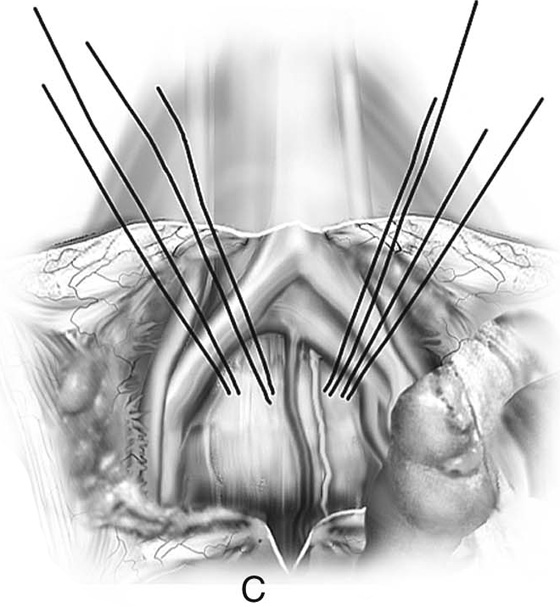
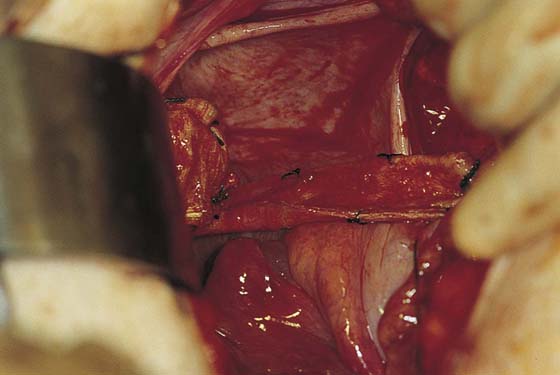
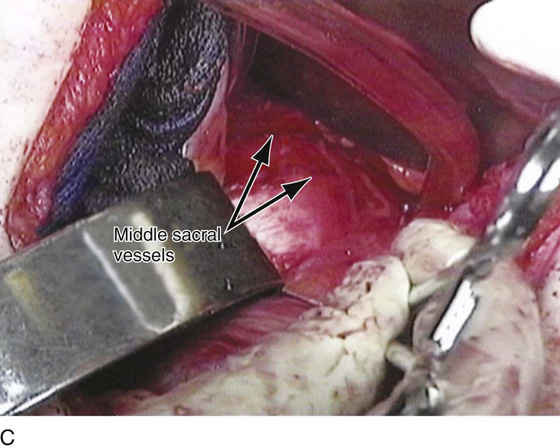
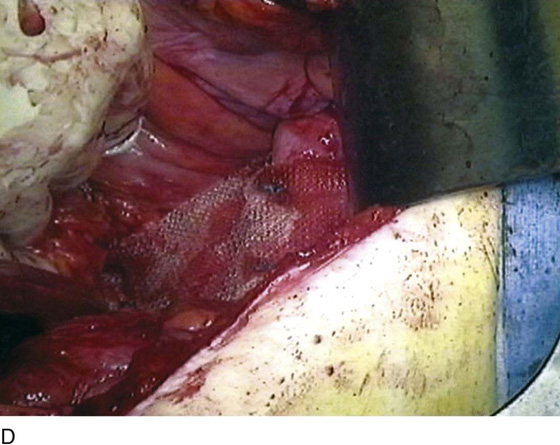
5. A longitudinal incision then is made over the peritoneum of the sacral promontory. The landmarks for this incision should be the right ureter and the medial edge of the sigmoid colon (Fig. 43–11). Very gentle dissection of the areolar tissue underneath the peritoneum is performed, usually in a blunt fashion, with a suction tip or a swab mounted on a curved forceps. The surgeon should be careful to palpate the aortic bifurcation and the common and internal iliac vessels and to mobilize the sigmoid colon to the left and the right ureter to the right, so that these structures can be avoided. The left common iliac vein is medial to the left common iliac artery and is particularly vulnerable to damage during this procedure. Very gentle dissection is performed down onto the sacral promontory to allow identification of the longitudinal ligament of the sacrum. The middle sacral vessels should also be easily visualized (Figs. 43–12 and 43–13). These vessels should be completely avoided. Ligation or cauterization should never be performed in the hope of preventing vascular injuries, as these vessels will retract into bone and create bleeding that is very difficult to control. If bleeding is encountered in this area, pressure should be applied on the bleeding vessels with a sponge stick. If this approach is unsuccessful, consideration can be given to the use of bone wax or the placement of sterile thumbtacks. The bony sacral promontory and the anterior longitudinal ligaments are directly visualized for approximately 4 cm with the use of blunt and sharp dissection through the subperitoneal fat. As dissection is carried caudad, special care should be taken to avoid the delicate plexus of presacral veins that is often present. With a stiff but small curved tapered needle, two to four 0 nonabsorbable sutures are placed through the anterior sacral longitudinal ligament over the sacral promontory (see Figs. 43–12 and 43–14). As few as one or two sutures can be placed, depending on the vasculature and exposure of the area. The graft should be trimmed to the appropriate length. The sutures then are fed through the graft and are paired and tied (Figs. 43–15 and 43–16). The appropriate amount of vaginal elevation should provide minimal tension and avoid undue traction on the vagina.
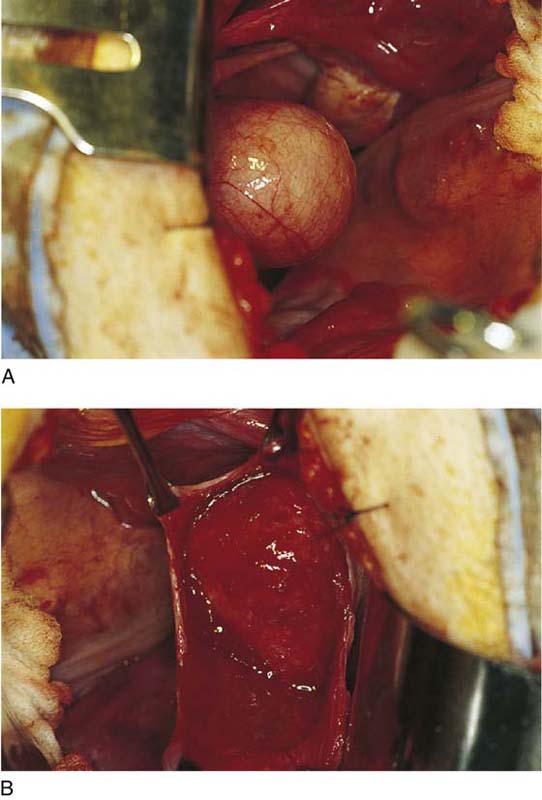
FIGURE 43–1 This patient has very obvious weak pelvic connective tissue as indicated by urethral prolapse, uterine prolapse, and rectal prolapse. In the author’s opinion, this patient would be an excellent candidate for abdominal sacral colpopexy.
FIGURE 43–2 This patient has had two previous anterior and posterior repairs. She now presents with a foreshortened vagina with an enterocele and vault prolapse. A properly performed abdominal sacral colpopexy will preserve her vaginal length and provide a durable repair.
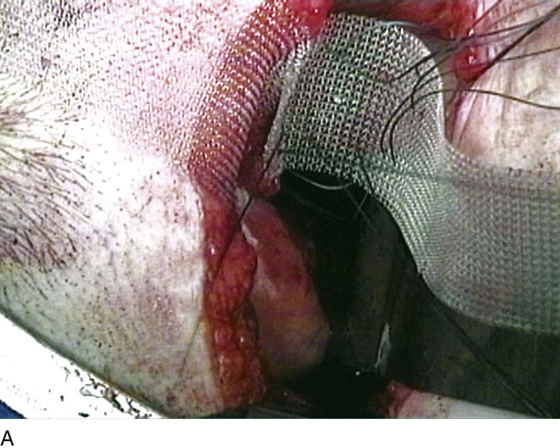
FIGURE 43–3 Many different materials have been used for a graft to bridge the vagina to the sacrum. A. Fascia lata. B. Marlex mesh. C. Prolene mesh. D. Mersilene mesh, which has been removed transvaginally secondary to erosion.
FIGURE 43–4 EES sizers, used to elevate the vagina. They also can be placed in the rectum to assist in dissection of the vagina at the anterior rectal wall.
FIGURE 43–5 A. Elevated vagina, abdominal view. An EES sizer is used to elevate the vagina. B. The peritoneum over the vagina has been opened, exposing the vaginal cuff and anterior and posterior vaginal walls.
FIGURE 43–6 The vagina is elevated with an EEA sizer. The peritoneum over the vagina is opened, exposing the muscular portion of the vaginal wall (inset).
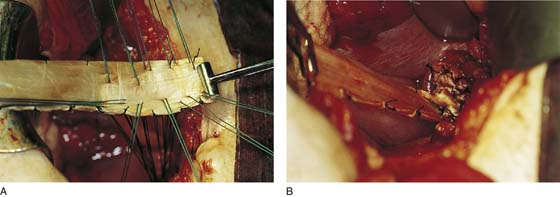
FIGURE 43–7 A series of permanent sutures are taken through the full thickness of the posterior vaginal wall (excluding epithelium), starting at the apex.
FIGURE 43–8 A. A large piece of cadaveric fascia lata. The marking pencil depicts how the fascia will be cut to prepare two pieces for colpopexy. B. The fascia has been cut and the pieces sutured to each other. A longer piece will extend from the posterior vaginal wall to the sacrum, and a shorter piece will attach to the anterior vaginal wall and the distal end of the longer piece.
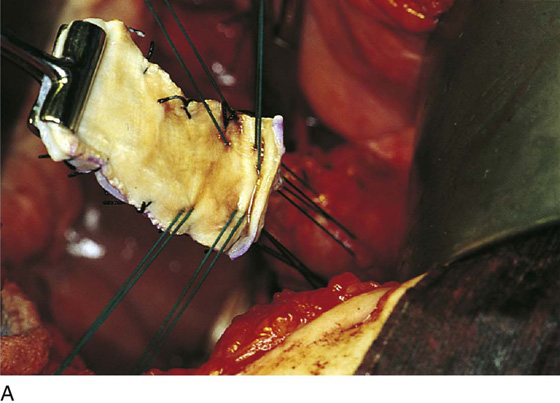
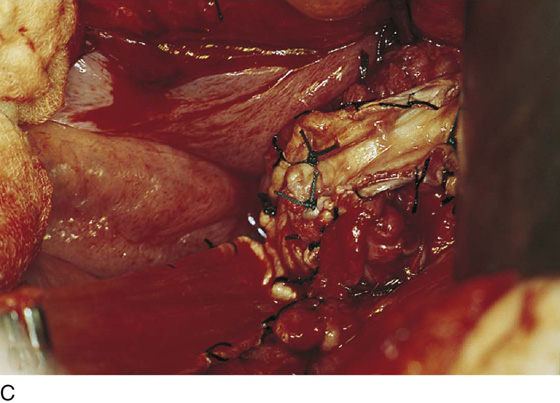
FIGURE 43–9 A. Passage of vaginal sutures through the cadaveric fascia lata. B. Sutures have been tied down, fixing the longer piece of fascia to the posterior vaginal wall.
FIGURE 43–10 A. Sutures have been passed through the upper portion of the anterior vaginal wall and are brought up through the smaller piece of fascia. B. Sutures have been tied down and are being connected to the other piece of fascia. C. The two pieces of fascia lata have been attached to the upper part of the anterior vaginal wall and the posterior vaginal wall.
FIGURE 43–11 An area of the sacral promontory is identified. The incision in the peritoneum should be well inside of the right ureter (marked with purple marking pencil) and the medial edge of the sigmoid colon.
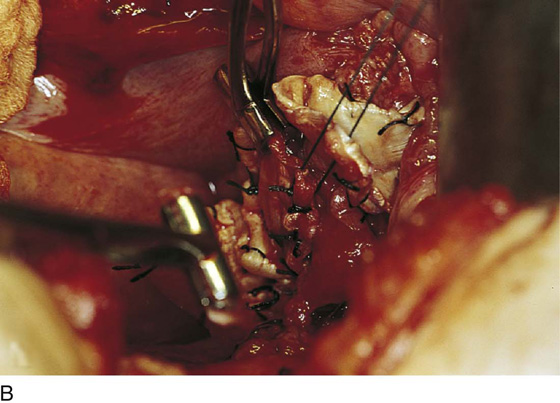
FIGURE 43–12 Anatomy of the sacral promontory. A. Incision into the peritoneum. B. Dissection to the longitudinal ligament of the promontory. Note the vascularity of this area. C. Placement of permanent sutures through the longitudinal ligament of sacrum.
FIGURE 43–13 Whitish-appearing periosteum of the sacral promontory.
FIGURE 43–14 Passage of permanent sutures through the longitudinal ligament of the sacrum.
FIGURE 43–15 Attachment of the mesh to the sacrum utilizing two pieces of mesh. Note that the anterior piece of mesh is fixed to the upper part of the anterior and extends much farther down the posterior vaginal wall. Both pieces are brought together and fixed to the sacral promontory. Closure of the peritoneum over the mesh is shown in the inset.
FIGURE 43–16 Fascia lata has been attached to the sacrum. Note that the fascia should lay in the cul-de-sac under minimal tension.
6. If necessary, a Moschcowitz or Halban procedure can be performed to obliterate the lower cul-de-sac, or the peritoneum over the cul-de-sac may be excised. Whatever technique is utilized, ultimately the graft must be extraperitonealized; thus the edges of the openings from the vagina to the sacrum are closed with a running delayed absorbable suture (Fig. 43–17).
7. When appropriate, retropubic urethropexy or paravaginal repair may be performed in conjunction with this procedure. Also, posterior colporrhaphy and perineoplasty usually need to be performed to treat the remaining rectocele and perineal defect. A transvaginal midline repair of a cystocele may also be necessary.
Figure 43–18 reviews the entire procedure, utilizing synthetic mesh (Prolene mesh).
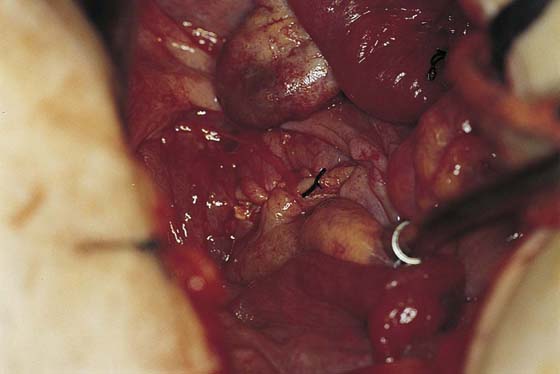
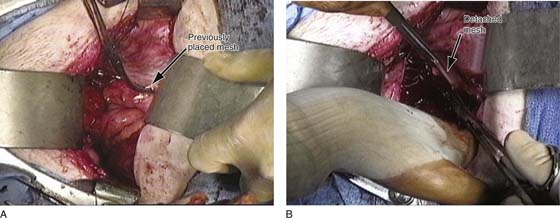
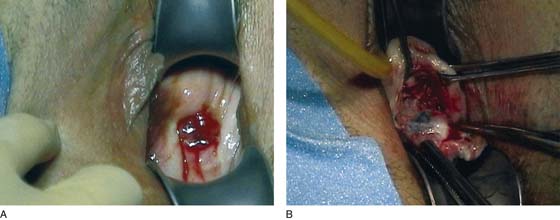
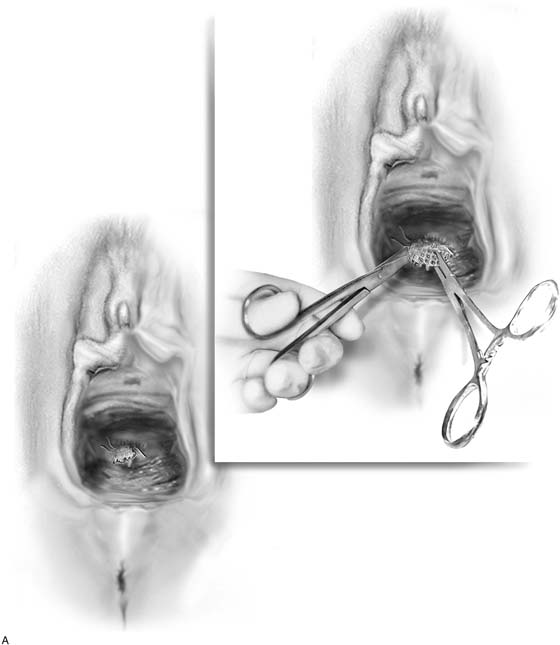
When these procedures fail and patients present with recurrent prolapse, most of the failures are due to inadequate attachment of the mesh to the vagina. For this reason, as was previously stated, it is very important to make sure that the mesh extends well down the posterior vaginal wall; we prefer to also attach a piece of mesh on the upper portion of the anterior vaginal wall. Figure 43–19 shows a patient who presented with recurrent vaginal vault prolapse after a previous abdominal sacral colpopexy performed with permanent mesh. On re-exploration, the previously placed mesh is found completely detached from the vagina (see Fig. 43–19). In this setting, the mesh was dissected away from the peritoneum and excised up to the level of the sacrum and then removed (Fig. 43–19B). The procedure was then repeated with a new synthetic mesh with a more aggressive fixation performed at the level of the vagina. Approximately 3% to 5% of patients who have undergone an abdominal sacral colpopexy with synthetic mesh will present with an erosion of the mesh into the vagina. Usually these patients will present with vaginal bleeding and a persistent malodorous vaginal discharge (Fig. 43–20). It has been our experience that most of these cases can be managed transvaginally by dissecting the mesh away from the vagina and utilizing aggressive downward traction on the mesh to assist in sharply dissecting it off the various tissues. The goal is to mobilize as much of the mesh as possible and then eventually cut the mesh as high up as possible. It is not necessary to remove the entire mesh. If a piece of mesh remains attached to the level of the sacrum and the distance between the distal end of that mesh and the closed vagina is sufficient, the potential for recurrent mesh erosion should be very low (Fig. 43–21).
FIGURE 43–17 The peritoneum has been closed over the mesh, thus placing the fascia retroperitoneally.
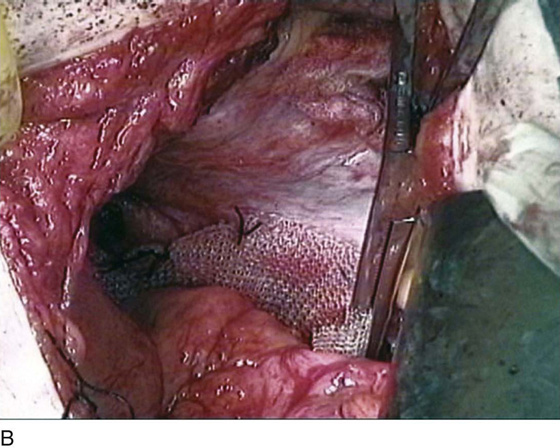
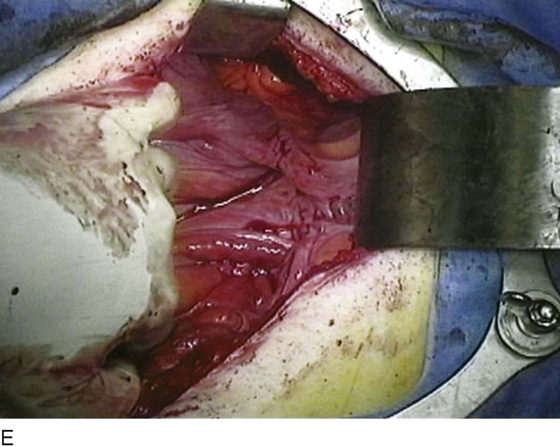
FIGURE 43–18 Technique of abdominal sacral colpopexy performed with polypropylene mesh. A. A piece of polypropylene mesh is being attached with numerous permanent sutures to the anterior vaginal wall. B. A second piece of mesh has been attached down the posterior vaginal wall; the two meshes have been brought together in a Y fashion and will be attached to the sacral promontory. A Kelly clamp is used to determine the appropriate tension of the repair. In general, there should be little tension on the mesh, and it should sit very loosely in the cul-de-sac between the vagina and the sacral promontory. C. The area where the mesh will be attached at the level of the sacrum has been exposed. Again, this is at the level of the sacral promontory, and the sutures will be taken through the longitudinal ligament of the sacrum. Note that the middle sacral vessels are easily visualized at this level. D. The Prolene mesh has been attached at the level of the vagina and at the level of the sacrum. E. The peritoneum has been closed over the mesh, thus making the mesh an extraperitoneal structure. Note that with reperitonealization, most of the cul-de-sac is obliterated, as can be seen in this photograph.
FIGURE 43–19 A patient with recurrent prolapse who has previously undergone an abdominal sacral colpopexy. A. With re-exploration, the previously placed mesh is identified. As noted in this photograph, it is completely detached from the vagina. B. The detached mesh is dissected away from the tissue to be completely excised.
FIGURE 43–20 A patient with an erosion of a synthetic mesh after a previous abdominal sacral colpopexy. A. Note that the mesh appears at the apex of the vagina. B. With sharp downward traction on the mesh, it is dissected away from the vaginal tissue, with the goal of completely dissecting the distal portion of the mesh and with aggressive downward traction excising it as high up as possible.
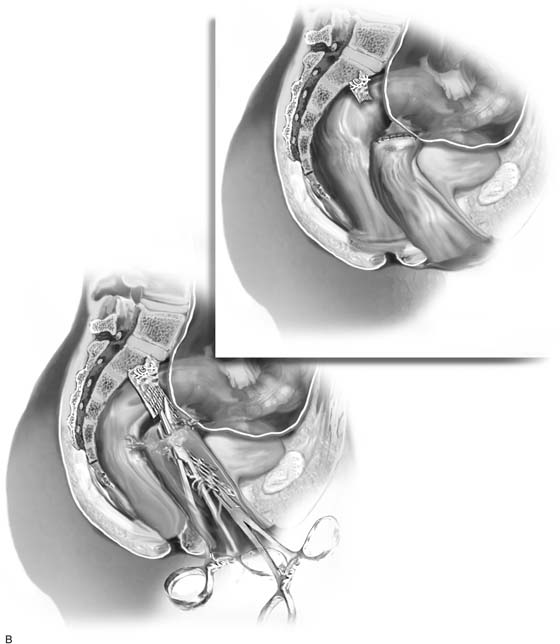
FIGURE 43–21 The technique of vaginal removal of an eroded synthetic mesh after abdominal sacral colpopexy. A. Note that the mesh is identified and grasped (usually with Kocher-type clamps), with aggressive downward traction applied on the mesh. B. The mesh is sharply dissected away from the vaginal tissue and any other tissue that it is adherent to, and, again with aggressive downward traction, it is excised as high up as possible. The goal is to create as much distance as possible between the closed vaginal cuff and the cut edge of the mesh (see inset).