Problem 13 Abdominal pain in a young woman
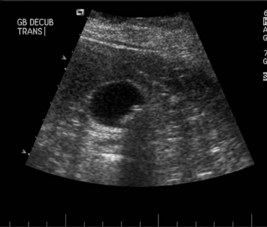
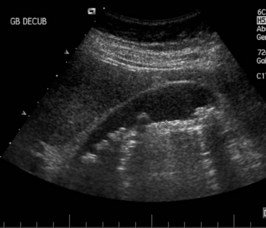
An ultrasound examination of the upper abdomen is performed (Figures 13.1 and 13.2).
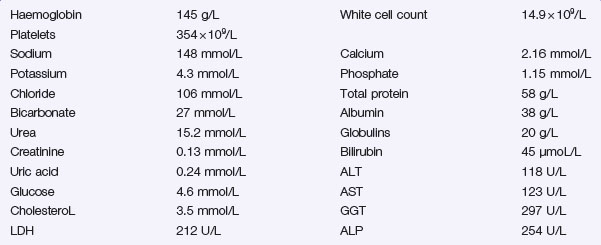
There is bilirubin + on urinalysis. Her serum biochemistry is shown below.
The day after admission the patient is feeling much better and is pain-free.
The ERCP is performed and the image shown in Figure 13.3 is obtained.
Answers
A.1 Further information must be sought on:
Other diagnoses to consider include:
A.2 The following investigations are required:
Revision Points
Gallstones
Types
Issues to Consider
, http://www.quackwatch.com/. One practitioner’s efforts to expose many of the fraudulent claims made by the proponents of alternative medicine. Search for ‘gallstones’
, http://www.gastro.org/patient-center/digestive-conditions/gallstones. Up-to-date information on gallstones with a patient slant, from the American Gastroenterological Society