Abdominal pain & abdominal trauma
The AXR—its usefulness
A patient with abdominal trauma does not require a plain abdominal radiograph (AXR). The AXR will not contribute to the clinical diagnosis and should be avoided.
The AXR is of limited value as a diagnostic tool in the evaluation of many patients presenting with an acute abdomen. This is largely because the abdominal contents are composed of soft tissue. Plain film radiography does not provide adequate soft tissue contrast discrimination to detect and differentiate between many of the numerous inflammatory and neoplastic intra-abdominal soft tissue pathologies. The AXR is not the right tool for the job. Consequently, it has been superseded by ultrasound and CT scanning which are highly accurate in terms of evaluating the various intra-abdominal soft tissues.
In present day clinical practice, the AXR is in the main limited to confirming a clinical suspicion of large or small bowel obstruction (as illustrated below), and demonstrating dangerous swallowed foreign bodies. Even so, CT will be selected as the first line imaging test in many cases of suspected intestinal obstruction, and also as the preferred and only imaging examination when renal colic is suspected.
What if the preferrred imaging investigations are not immediately available? Is there any point in requesting an AXR as a substitute imaging test? On the whole, no. You risk obtaining false reassurance from a seemingly normal AXR appearance. It is safer to rely on a detailed clinical history and a careful physical examination. Furthermore, an experienced pair of examining hands from a member of the surgical team will recognise the emergency case that needs to go to theatre.
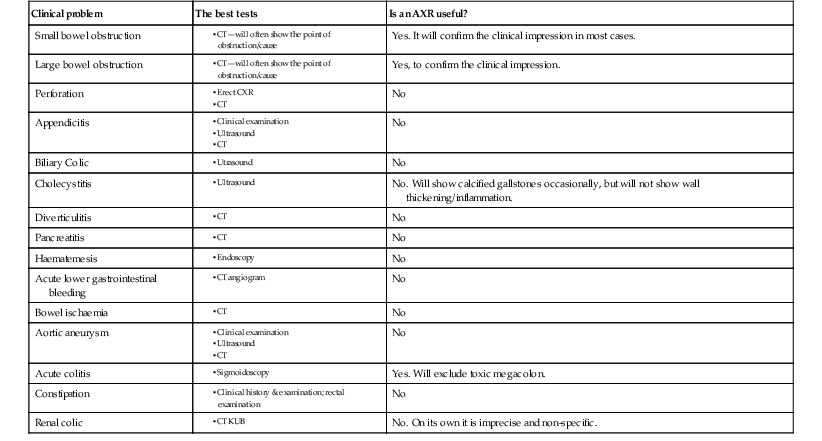
The table on the right indicates the relatively few occasions when an AXR can be useful.
▪ CT
▪ CT
▪ CT
▪ CT KUB
Analysis: plain film checklists
Erect CXR
In the context of a patient attending the Emergency Department with abdominal pain there are just two questions to ask of the CXR:
Supine AXR
When analysing an AXR some normal features can be listed:
The common problems1–10
Both the likelihood of a particular diagnosis and the level of clinical concern will determine the specific radiological investigation that is selected. In some instances no imaging will be requested. The local availability of equipment or particular skills may also influence the choice of the first line test.
The following descriptions refer solely to plain film radiography; ie when a supine AXR or a CXR is obtained in the Emergency Department.
Non-specific abdominal pain
An erect CXR is primarily obtained in order to exclude a basal pneumonia or free air under the diaphragm. A supine AXR is not a useful test, because:
▪ A normal AXR does not exclude serious pathology.
▪ A good clinical history and physical examination are more useful than an AXR.
Following clinical examination the most useful imaging tests are CT or ultrasound. In the absence of these facilities, an AXR is unlikely to be better than the clinical examination performed by an experienced member of the surgical team.
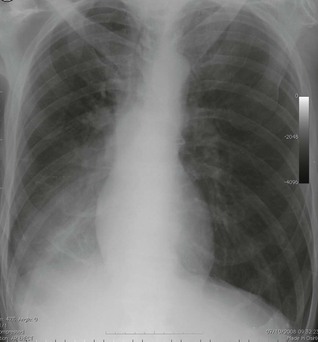
Suspected perforation
The most useful radiograph is a well-penetrated erect CXR. An erect AXR is not indicated as the CXR is much more reliable in detecting free air. Very small quantities (as little as 1.0 ml) of free air can be demonstrated on an erect CXR2.
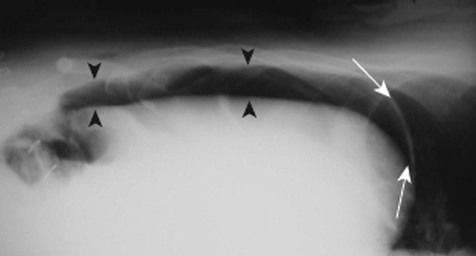
If a patient is unable to sit up for an erect CXR then an alternative technique is employed: the patient reclines in the left-side-down decubitus position and a cross table AXR is obtained using a horizontal X-ray beam.
Other options:
▪ In a few centres sonography is utilized for the detection of free intraperitoneal air3. Practitioners tend to follow a step by step protocol. As follows: plain radiography first; then ultrasound only in those in whom the plain radiograph (usually an erect CXR) is normal. CT is thus reserved for those occasions when ultrasonograhy still fails to make the diagnosis6.
Suspected intestinal obstruction
The options:
1. CT.
CT is highly accurate in demonstrating or excluding obstruction4,5. In addition, the precise site and probable cause of the obstruction can usually be defined. In an individual patient, the surgical team may well prefer CT as the first line imaging test, because of the excellent detail and additional information that will be provided.
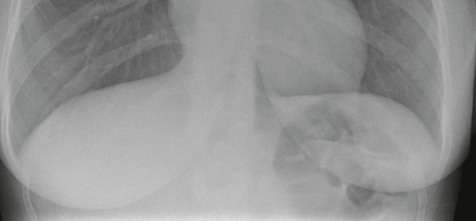
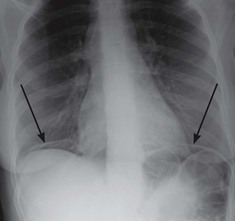
2. Supine AXR.
Some basic features will assist with diagnosis.
Suspected constipation
The plain AXR is rarely of help in reaching a diagnosis of constipation as being the likely cause of abdominal pain. Because:
Suspected renal colic
The options:
1. Unenhanced multidetector CT, often referred to as a CT KUB.
The CT KUB is now established as the preferred imaging test when renal colic is suspected5–9. It is an accurate and quick examination and there is no need for intravenous contrast medium injection.
2. Sonography.
A case has been made that in female patients presenting with flank pain and suspected renal colic, sonography should be the initial examination in order to detect the presence of hydronephrosis6. This alternative approach is (a) based on consideration of the CT radiation dose to the ovaries and (b) because sonography is so good at detecting other pathologies deep in the female pelvis that may account for the patient’s symptoms.
3. AXR plus sonography.
Others have suggested that patients should have an AXR and ultrasound as a combination examination and if negative that CT should be reserved for the patient who does not subsequently improve on conservative management10. The addition of the AXR has been found to improve the accuracy of diagnosis of renal colic,ie when compared with ultrasound as the solitary examination10.
4. Limited intravenous urography.
Carried out as a two film examination: A plain AXR will be diagnostic when there is an obvious opaque calculus in the line of the renal tract. It is less helpful if the film (image) appears normal. A calculus might be obscured by superimposed bone, or confused with a pelvic phlebolith, or might simply be insufficiently radio-opaque to be seen. Although 90% of renal calculi contain calcium, less than 50% are visible on an AXR. Consequently, a single additional AXR at 10 minutes after the intravenous injection of contrast medium will be highly accurate in confirming or excluding the presence of a ureteric calculus. Normal excretion of the contrast medium together with undilated calyces and ureter will exclude the diagnosis of renal colic; delay in excretion on the painful side and/or calyceal/ureteric dilatation will confirm the diagnosis of renal colic.
Suspected acute biliary disease
Sonography is the first line imaging procedure whenever the suspicion is that of biliary colic or gall bladder disease.
Suspected abdominal aortic aneurysm/rupture
Sonography is the first line investigation.
Suspected foreign body ingestion
The important roles of the CXR, the AXR and hand held metal detector scanning are described in Chapter 21 (Swallowed Foreign Bodies).
Infrequent but important problems
Blunt trauma to the abdomen
In patients who have sustained abdominal or pelvic trauma the rapid assessment of the injury is critical. Delay increases mortality and morbidity11.
Penetrating injury to the abdomen