CHAPTER 60 Abdomen and pelvis: overview and surface anatomy
GENERAL STRUCTURE AND FUNCTION OF THE ABDOMINOPELVIC CAVITY
MUSCULOSKELETAL FRAMEWORK OF THE ABDOMEN AND PELVIS
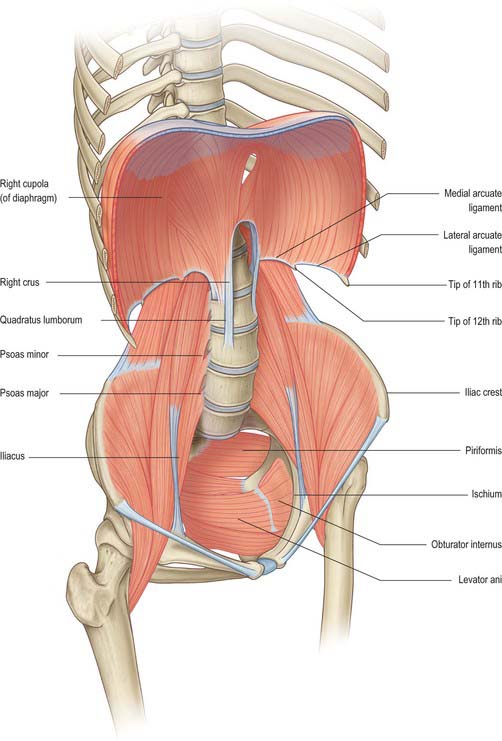
The walls of the abdominopelvic cavity consist of five lumbar vertebrae and their intervening intervertebral discs (lying in the posterior midline); three layers of skeletal muscles (transversus abdominis, internal oblique and external oblique) with associated fasciae and skin (lying lateral and anterolateral); a single muscular layer (rectus abdominis) with its associated fascial coverings (lying anterior); the bony ‘bowl’ formed by the walls of the true and false pelvis (ilium, ischium and pubis on each side); the muscles of the pelvic floor and perineum (lying inferiorly); the diaphragm (lying superiorly) (Fig. 60.1).
Thoracoabdominal interface
The thoracic and abdominal cavities interface with each other across the diaphragm. Six principle communications exist between the two cavities: the inferior vena cava, as it crosses between its short supra-hepatic portion and the intrathoracic portion below the right atrium, through the caval opening of the diaphragm (Ch. 62); the oesophagus passing inferiorly through the oesophageal opening of the diaphragm (Ch. 65); the aorta between the descending thoracic and abdominal portions, posterior to the median arcuate ligament of the diaphragm (Ch. 62); the lymphatics of the abdomen draining upwards to the thorax, mainly posterior to the median arcuate ligament via the thoracic duct lying posterolateral to the aorta, but also via peri-caval lymphatics and small vessels draining directly through and at the peripheral insertions of the diaphragm; the azygos and hemiazygos veins ascending behind the median arcuate ligament of the diaphragm into the thoracic azygos system (Ch. 62); the autonomic nervous system, both sympathetic and parasympathetic (see below) which cross between the two cavities behind the medial arcuate ligaments of the diaphragm, via the various diaphragmatic openings, and directly through the substance of the diaphragm itself (Ch. 54). Cutaneous neurovascular structures also cross between the thorax into the abdominal wall structures.
Pelvis–lower limb interface
The pelvis forms an integral part of the bony structure of both the abdominopelvic cavity and the lower limb. It transmits the weight of the upright body from the femoral heads to the lumbar spine as well as providing a stable platform about which movement of the hip joint can occur. Its bony surfaces give rise to extensive muscular attachments for the muscles of the buttock and thigh (Ch. 67) as well as for the muscles of the pelvic floor and perineal diaphragm (Ch. 63). The pelvis also transmits or gives origin to the neuro-lympho-vascular structures which supply the lower limb. The principle structures are as follows. The venous drainage includes the common femoral vein passing under the inguinal ligament to become the external iliac vein; the obturator veins passing through the obturator foramen; the superior and inferior gluteal veins draining from the buttock into the internal iliac vein via the greater and lesser sciatic foramina; multiple smaller venous channels. The arterial supply includes the external iliac artery passing under the inguinal ligament to become the common femoral artery; the obturator artery passing into the thigh via the obturator foramen; the superior and inferior gluteal arteries from the posterior division of the internal iliac artery passing out of the pelvis via the greater and lesser sciatic foramina. The lymphatic drainage principally passes under the inguinal ligament, via the femoral and obturator canals and via the sciatic foramina, to drain into the pelvic lymphatic chains (Ch. 63). The somatic neural structures include the femoral, obturator and sciatic nerves and other minor branches of the lumbosacral plexus (Ch. 62). The autonomic neural structures include those running with the arterial supply and with the branches of the lumbosacral plexus. Cutaneous neurovascular structures also cross between the lower abdomen and pelvis into the skin and superficial tissues of the lower limb.
GENERAL ARRANGEMENT OF ABDOMINOPELVIC NEUROVASCULAR STRUCTURES
AUTONOMIC SUPPLY
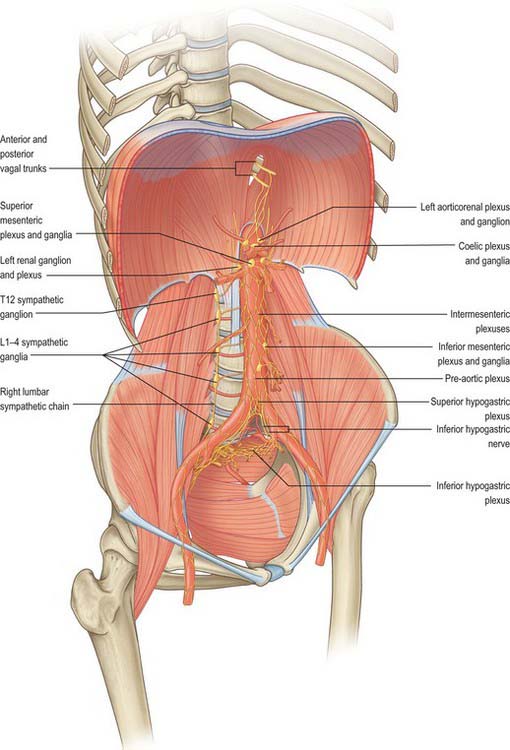
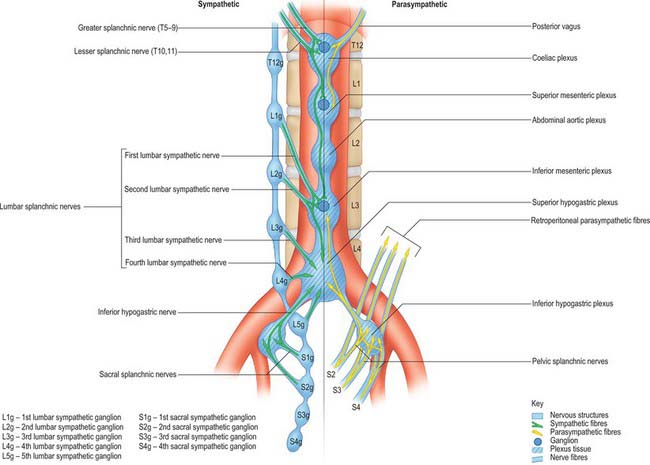
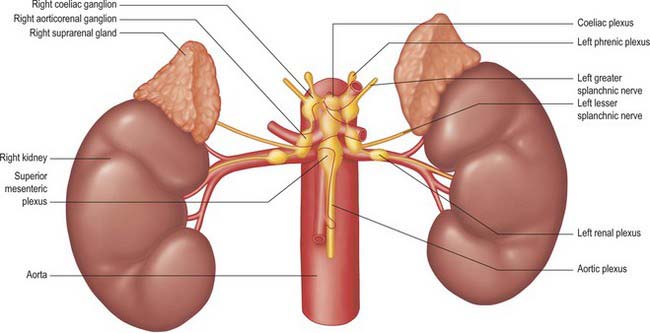
The autonomic supply to the abdominal and pelvic viscera is via the abdominopelvic part of the sympathetic chain and the greater, lesser and least splanchnic nerves (sympathetic), and the vagus and pelvic parasympathetic nerves (parasympathetic). Considerable ramification occurs between plexuses and ganglia, particularly in the major plexuses around the abdominal aorta, hence the descriptions tend to be simplifications based on the ‘main’ supply to each organ (Fig. 60.2). The details of the terminations of these fibres are given on page 1050.
Sympathetic innervation
Least splanchnic nerve
The least splanchnic nerve is derived from the medial, visceral branches of the 12th thoracic ganglia. It enters the abdomen running with the sympathetic chain under the medial arcuate ligament and runs inferiorly to enter the renal plexus. The trunk of the nerve enters the aorticorenal ganglion and may give branches to the lateral aspect of the coeliac ganglion. It is sometimes part of the lesser splanchnic nerve, when it forms a twig which enters the renal plexus just below the aorticorenal ganglion.
Lumbar sympathetic system
Vascular branches
Vascular branches from all the lumbar ganglia join the abdominal aortic plexus. Fibres of the lower lumbar splanchnic nerves pass to the common iliac arteries and form a plexus which extends along the internal and external iliac arteries. Many postganglionic fibres travel in the muscular, cutaneous and saphenous branches of the femoral nerve, supplying vasoconstrictor nerves to the femoral artery and its branches in the thigh. Other postganglionic fibres travel via the obturator nerve to the obturator artery. Considerable uncertainty persists regarding the exact path of the sympathetic nerve supply to the lower limb (Pick 1970). Sympathetic denervation of vessels in the lower limb can be effected by removing or ablating the upper three lumbar ganglia and the intervening parts of the sympathetic trunk; very rarely, this procedure is useful in treating vascular insufficiency of the lower limb.
Parasympathetic innervation
Pelvic splanchnic nerves
The pelvic splanchnic nerves are motor to the smooth muscle of the rectum, anus and bladder wall but inhibitory to the vesical sphincter. They supply vasodilator fibres to the erectile tissue of the penis and clitoris and are probably also vasodilator to the testes, ovaries, uterine tubes and uterus. They are visceromotor to the sigmoid and descending colon as far as the splenic flexure and distal transverse colon.
Abdominopelvic autonomic plexuses and ganglia
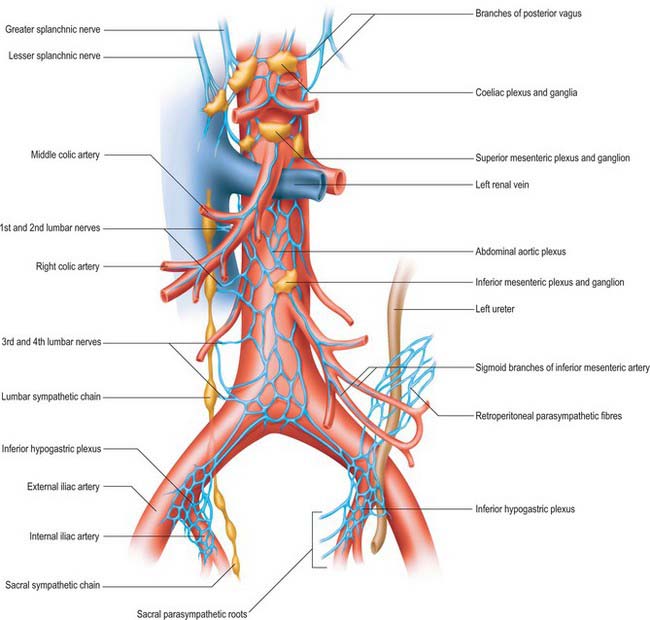
The abdominopelvic autonomic plexuses are somewhat variable and often fuse or are closely inter-related. The following descriptions recognize their main features (Figs 60.3, 60.4).
Coeliac plexus
The coeliac plexus is the largest major autonomic plexus, sited at the level of the twelfth thoracic and first lumbar vertebrae. It is a dense network uniting two large coeliac ganglia and surrounds the coeliac artery and the root of the superior mesenteric artery. It is posterior to the stomach and lesser sac, anterior to the crura of the diaphragm and the beginning of the abdominal aorta, and lies between the suprarenal glands. The plexus and ganglia are joined by the greater and lesser splanchnic nerves and branches from the vagus and phrenic nerves. The plexus extends as numerous secondary plexuses along adjacent arteries. The coeliac plexus is connected to, or gives rise to, the phrenic, splenic, hepatic, superior mesenteric, suprarenal, renal and gonadal plexuses (Fig. 60.5).
Abdominal aortic plexus (intermesenteric plexus)
The abdominal aortic plexus lies on the sides and front of the aorta, between the origins of the superior and inferior mesenteric arteries. It consists of 4–12 intermesenteric nerves, connected by oblique branches. It is continuous above with the superior mesenteric plexus and below with the superior hypogastric plexus, and is formed by parasympathetic and sympathetic branches from the coeliac plexus. It receives rami from the first and second lumbar splanchnic nerves (which contain sympathetic fibres). The abdominal aortic plexus is connected to the gonadal, inferior mesenteric, iliac and superior hypogastric plexuses.
Para-aortic bodies
The para-aortic bodies are condensations of chromaffin tissue which are found in close relation to the aortic autonomic plexuses and lumbar sympathetic chains. They are largest in the fetus, become relatively smaller in childhood and have largely disappeared by adulthood. They are most commonly found as a pair of bodies lying anterolateral to the aorta in the region of the intermesenteric, inferior mesenteric and superior hypogastric plexuses. They may lie as high as the coeliac plexus, as low as the inferior hypogastric plexus in the pelvis, or may be closely applied to the sympathetic ganglia of the lumbar chain. Scattered cells which persist into adulthood may, rarely, be the sites of development of a tumour of chromaffin tissue (phaeochromocytoma); these are much more commonly found arising from the cells of the suprarenal medulla. The wide variation in the site of persistent para-aortic body tissue accounts for the range of locations of such tumours.
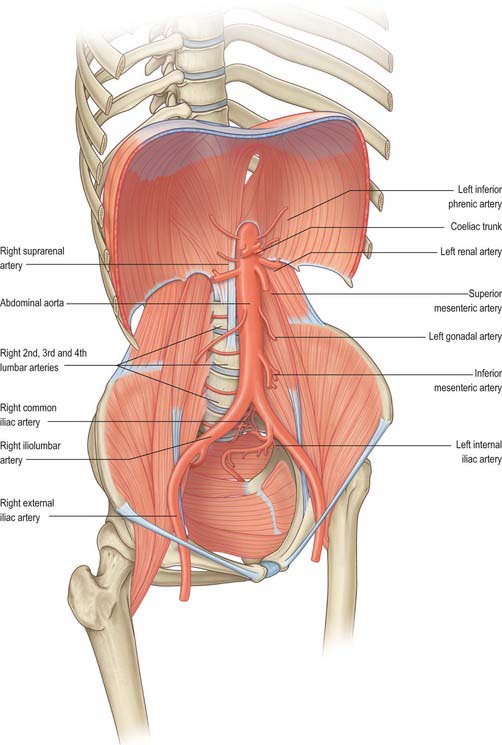
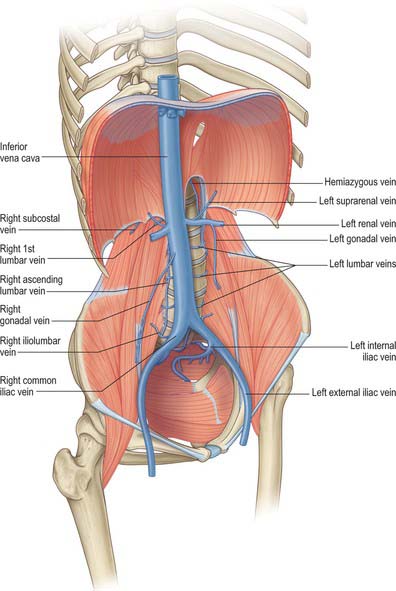
MAJOR ABDOMINOPELVIC ARTERIAL AND VENOUS ARRANGEMENTS
The major vessels which occupy the abdomen and pelvis not only supply the viscera, retroperitoneal structures and much of the bony and soft tissue walls of the cavities, they also course through the cavities en route to supply the lower limbs. Both the arterial and systemic venous trees of the abdomen and pelvis lie predominantly posteriorly in the abdomen and postero-laterally in the pelvis; from the caval and aortic orifices in the diaphragm and the other points where smaller vessels cross the abdominothoracic interface, they follow the general parabolic shape of the lumbar spine. The pelvic divisions follow the contours of the brim and side wall of the true pelvis (Figs 60.6, 60.7). The individual parts of the aorto-iliac and iliocaval systems are described in the appropriate chapters.
Arterial supply to the gastrointestinal tract
The arterial supply to the gastrointestinal tract is derived from the anterior midline visceral branches of the aorta. There are usually three anterior branches, the coeliac trunk and the superior and inferior mesenteric arteries. Variants in the origin of the arteries are very rare. The most common is a joint origin of the upper two branches as either a coeliacomesenteric trunk or a lienohepaticomesenteric trunk with a separate left gastric artery. Accessory or replaced branches to the upper abdominal viscera are more common (see Chs 65, 66, 67 and 68). Accessory anastomotic vessels between the origin of the coeliac trunk and superior mesenteric artery are rare. The inferior mesenteric artery always arises separately, however, replaced, accessory or anastomotic vessels occasionally arise from the proximal superior mesenteric artery or its branches and contribute to the arterial supply to the proximal territory of the inferior mesenteric artery.
The coeliac trunk and its branches supplies the gastrointestinal tract from the distal third of the oesophagus to the mid part of the duodenum and all derived adenexae (liver, biliary tree, spleen, dorsal pancreas, greater omentum and lesser omentum). The superior mesenteric artery supplies the tract from the mid second part of the duodenum to the distal third of the transverse colon (jejunum, ileum, caecum, appendix, ascending colon and ileal mesentery). The inferior mesenteric artery supplies the tract from the distal transverse colon to the upper anal canal. Other than accessory arteries, numerous medium calibre arteries form anastomoses between the vascular territories. The most profuse occurs around the head of the pancreas and the duodenum, where anastomoses form between the anterior and posterior superior pancreaticoduodenal arteries and the inferior pancreaticoduodenal arteries; the posterior superior pancreaticoduodenal artery and jejunal arteries; the greater pancreatic artery and jejunal arteries. The anastomoses between the territories of the superior and inferior mesenteric arteries are less pronounced and more variable: the most reliable is the pericolic marginal artery, which runs along the transverse colon. Additional anastomotic arcades may exist in the colic mesentery between the transverse and descending colon.
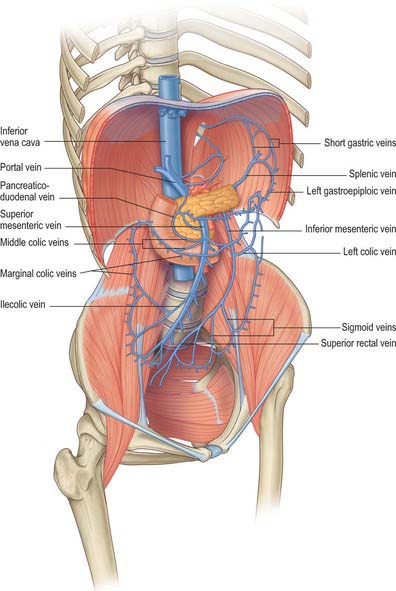
Portal venous system
Portal vein
The portal vein begins at the level of the second lumbar vertebra and is formed from the convergence of the superior mesenteric and splenic veins (see Fig. 70.8). It is approximately 8 cm long and lies anterior to the inferior vena cava, posterior to the neck of the pancreas (Fig. 60.8) and obliquely to the right. It ascends behind the first part of the duodenum, the common bile duct and gastroduodenal artery. At this point it is directly anterior to the inferior vena cava. It enters the right border of the lesser omentum, ascends anterior to the epiploic foramen to reach the right end of the porta hepatis, and then divides into right and left main branches which accompany the corresponding branches of the hepatic artery into the liver. In the lesser omentum it lies posterior to both the common bile duct and hepatic artery. The portal vein is surrounded by the hepatic nerve plexus and accompanied by many lymph vessels and some lymph nodes.
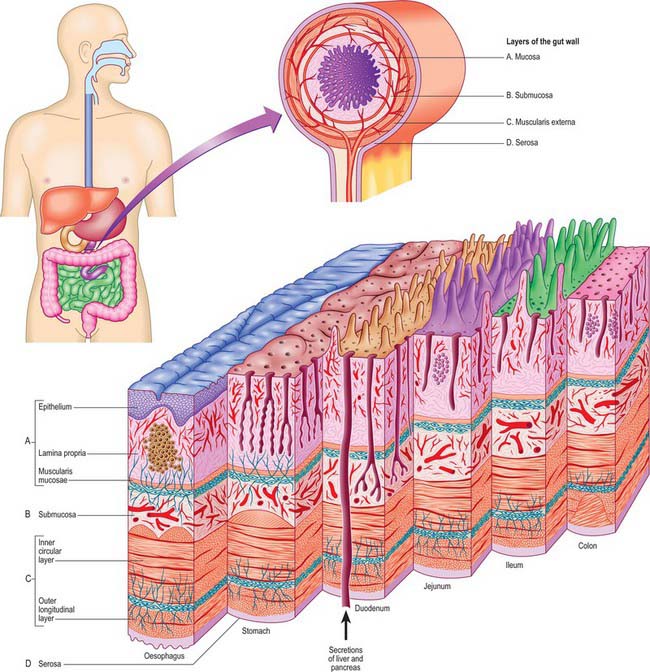
GENERAL MICROSTRUCTURE OF THE GUT WALL
The gut wall displays a common structural plan which is modified regionally to take account of local functional differences. The general microstructure is best appreciated by reference to the development of the gut (Ch. 73). Much of the alimentary canal originates as a tube of endoderm enclosed in splanchnopleuric mesoderm. Its external surface faces the embryonic coelom, and the endodermal lining forms the epithelium of the canal and also the secretory and ductal cells of various glands which secrete into the lumen, including the pancreas and liver. The splanchnopleuric mesoderm forms the connective tissue, muscle layers, blood vessels and lymphatics of the wall, and its external surface becomes the visceral mesothelium or serosa. There is no serosa surrounding the cervical and thoracic portions of the gut, or where the hindgut traverses the pelvic floor: in these sites the gut tube is surrounded by a connective tissue adventitia. Neural elements invade the gut from neural crest tissue (Ch. 24). The smooth muscle of the muscularis externa layers of the alimentary canal is supplemented with striated muscle both cranially (from the branchial arches) and caudally. The mature gut wall has four main layers, namely mucosa, submucosa, muscularis externa and serosa (Fig. 60.9). The mucosa (mucous membrane) is the innermost layer and is subdivided into a lining epithelium, an underlying lamina propria (a layer of loose connective tissue, where many of the glands are also found) and a thin layer of smooth muscle, the muscularis mucosae. The submucosa is a strong and highly vascularized layer of connective tissue. The muscularis externa consists of inner circular and outer longitudinal layers which are present throughout the gut wall: a partial oblique layer is present only in the stomach. The external surface is bounded by a serosa or adventitia, depending on its position within the body.
Mucosa
Epithelium
The barrier function and selectivity of absorption depend on tight junctions over the entire epithelium. The surface area of the lumen available for secretion or absorption is increased by the presence of mucosal folds, pits, crypts, villi and glands (Fig. 60.9). Microvilli on the surfaces of individual absorptive cells amplify the area of apical plasma membrane in contact with the contents of the gut. Some glands lie in the lamina propria, some in the submucosa, and others (the liver and pancreas) are totally external to the wall of the gut. All of these glands drain into the lumen of the gut through individual ducts. The epithelium also contains scattered neuroendocrine (enteroendocrine) cells.
Innervation
The gut is densely innervated by the autonomic and enteric nervous systems, and is under extrinsic and intrinsic neuronal control. Neuronal cell bodies of the enteric nervous system lie between the circular and longitudinal components of the muscularis externa (myenteric plexus) and within the submucosa (submucosal plexus). They provide the intrinsic sensory and motor supply of the gut wall and connect with extrinsic sensory, motor and sensorimotor nerves of cranial or spinal origin.
Extrinsic innervation
The extrinsic innervation is derived from neurones outside the gut, and contains functional components from the sympathetic, parasympathetic and visceral sensory divisions of the peripheral nervous system (see p. 1041). Visceral sensory endings respond to excessive muscular contraction or distension: their cell bodies are situated in the nodose ganglion of the vagus nerve and in thoracic and lumbar spinal or dorsal root ganglia. The cell bodies of parasympathetic efferent axons lie in the vagal dorsal motor nucleus in the medulla oblongata. Sympathetic efferent fibres arise from the thoracic and lumbar spinal cord and relay in prevertebral sympathetic ganglia (coeliac, mesenteric and pelvic).
SURFACE AND DIAGNOSTIC ANATOMY OF THE ABDOMEN AND PELVIS
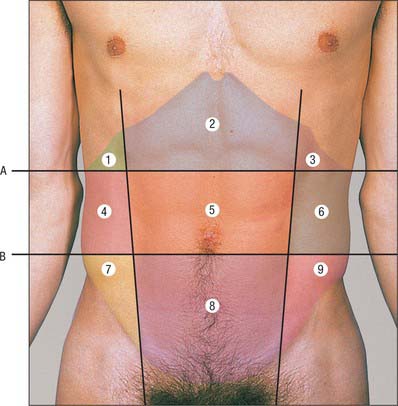
ABDOMINAL PLANES AND REGIONS
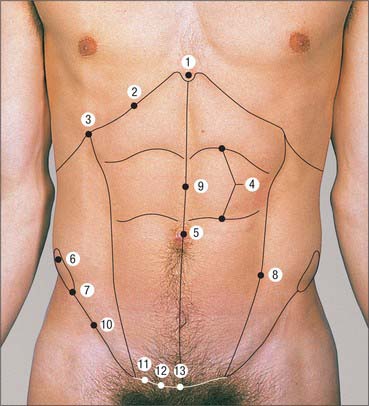
ANTERIOR ABDOMINAL WALL
Skeletal landmarks
The superior boundary of the anterior abdominal wall is formed by several clear landmarks (Fig. 60.11). In the midline superiorly lies the xiphoid process. From this point, the costal margins extend to either side from the seventh costal cartilage at the xiphisternal joint to the tip of the twelfth rib (the latter is often difficult to feel in the obese or if it is short). The lowest part of the costal margin lies in the midaxillary line and is formed by the inferior margin of the tenth costal cartilage. The tip of the lower border of the ninth costal cartilage can usually be defined as a distinct ‘step’ along the costal margin.
The posterolateral boundary is defined by the midaxillary line.
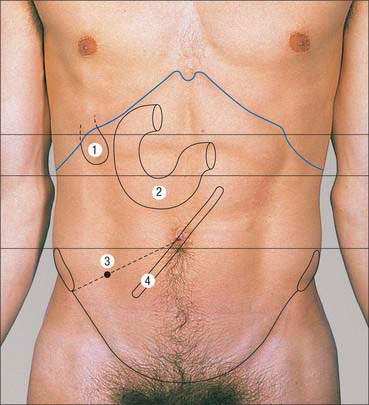
INTRA-ABDOMINAL VISCERA
The surface markings of the intra-abdominal viscera are variable and depend on age, body habitus, nutritional state, phase of ventilation and body position. The use of radiological imaging of the abdominal viscera means that the location of viscera by surface markings is almost obsolete in modern clinical practice. The following descriptions are at best regarded as the most common or approximate markings in a healthy supine individual (Fig. 60.12).