Problem 36 A young woman with jaundice
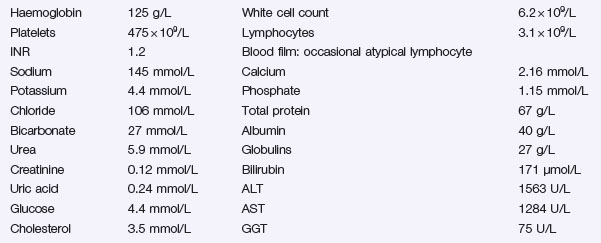
The results of some initial investigations are as follows:
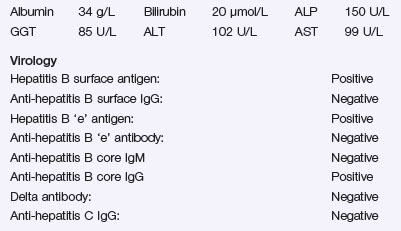
The following results become available:
Investigation 36.2 Ultrasound of liver
Investigation 36.3 Department of virology
| Anti-hepatitis A IgM: | Negative |
| Hepatitis B surface antigen: | Positive |
| Anti-hepatitis B core IgM: | Positive |
| Anti-hepatitis C IgG: | Negative |
| Hepatitis C antibody: | Positive |
| Hepatitis C viral PCR: | Negative |
| HIV antibody: | Negative |
Liver synthetic function remains normal. She remains nauseated and finds it difficult to eat.
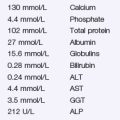
Investigation 36.5 Son’s test results
| Virology | |
| Hepatitis B surface antigen: | Negative |
| Anti-hepatitis B surface IgG: | Negative |
| Anti-hepatitis B core IgG: | Negative |
| Anti-hepatitis C IgG: | Negative |
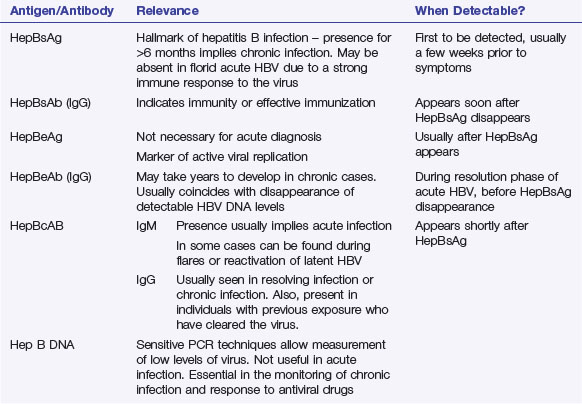
Answers
A.1 The history is extremely important. It is essential in making the final diagnosis. Her Intravenous drug use (IDU) is a major risk factor in acquiring a blood-borne hepatitis virus (B, C, D). Ascertain if she has shared needles, and when, for clues as to the likelihood and possible length of infection. HBV is more readily transmitted by sex than HCV. Risk of blood transfusion transmission is now rare since blood in developed countries is screened for blood-borne viruses. Tattoos are low risk if done professionally. She could have a faeco-orally transmitted viral hepatitis (hepatitis A or E), but HBV or HCV seem more likely. However, other possibilities should not be dismissed (Table 36.1).
Table 36.1 Risk factors for hepatitis in the acutely jaundiced patient
| Diagnosis | Important Points in History |
|---|---|
| Hepatitis A | Contacts, foreign travel, recent diarrhoeal illness, dietary risk factors, e.g. shellfish ingestion, recreational risk factors, e.g. swimming and surfing, esp. urban beaches |
| Hepatitis B | Close contacts, sexual history, blood transfusion, IDU, foreign travel, tattoos, body piercing |
| Hepatitis E | As for hepatitis A |
| Other viruses, e.g. EBV | Contacts, sore throat, age |
| Drug-induced hepatitis | Recent medications, although do not get caught out as can be as long as 1–2 months since offending drug was taken – detailed drug history is important; frequently antibiotics, especially flucloxacillin and co-amoxiclav; over-the-counter drugs (especially NSAIDs); complimentary therapies; Chinese medicines; recreational drugs; Ecstasy use |
| Alcohol-related hepatitis | Alcohol history |
| Autoimmune hepatitis | Age, female sex, history of other autoimmune disease, e.g. thyroid |
Consent should be sought to test for HIV.
Revision Points