Problem 7 A young woman with abnormal vaginal bleeding
A 32-year-old woman attends a general practice because she has had some irregular vaginal bleeding for the last 8 days. Her last normal menstrual period occurred 6 weeks ago. Her usual cycle length is between 4 and 6 weeks. She has been trying to conceive for the last 3 years, but has not managed to do so.
The results of the tests you arranged were as follows:
Investigation 7.1 Summary of results
| Haemoglobin | 42 g/L |
| White cell count | 8.5 × 109/L |
| Platelets | 160 × 109/L |
| Urinary pregnancy test | positive |
| Serum beta hCG | 1200 U/L |
| Cervical PAP smear | no abnormal cells detected; endocervical cells identified |
| Cervical swab | no evidence of chlamydial infection |
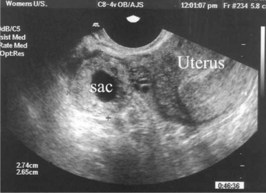
On the basis of the positive pregnancy test a pelvic ultrasound examination is arranged (Figure 7.1).
Answers
• Is she pregnant and does she have a pregnancy complication? In someone with cycles of variable length, pregnancy is possible so symptoms of pregnancy need to be sought. In someone who has had difficulty conceiving, when a pregnancy is achieved the chance of it being in an ectopic position is increased. You need to ask whether her last menstrual period was of normal volume and duration as it is not uncommon for a ‘period’ to occur in someone who has conceived although the amount of bleeding at the time of the ‘period’ is usually less than normally occurs. If she is pregnant the current 8 days of bleeding could be an indication of the pregnancy being in the Fallopian tube, and not the uterus (an ectopic pregnancy), or that one of the various forms of abortion are occurring (threatened, incomplete, complete or missed abortion).
• If she is not pregnant, the most likely causes are a problem at the level of the cervix, or a disturbance of her oestrogen and/or progesterone levels resulting in irregular shedding of her endometrium (DUB = dysfunctional uterine bleeding).
• Is the bleeding from her cervix? For example, a cervical polyp or carcinoma? Check when her last PAP smear was done, whether PAP smears have ever been abnormal, whether there have been previous episodes of abnormal bleeding and whether she has ever had bleeding after sexual activity. Recurrent bleeding, and especially postcoital bleeding, often has a cervical origin.
• Does she have DUB? This would be suggested by the previous menstrual cycles being irregular, or where the definite symptoms associated with ovulatory menstrual cycles (midcycle mucus change, premenstrual bloating of the abdomen, premenstrual dysmenorrhoea) are absent.
• Abnormal bleeding in a woman with uterine fibroids is generally heavy bleeding at the time of the period. Bleeding between the periods is only likely if one of the fibroids is in the submucosal position and is being extruded.
A.3 The investigations required are:
• Threatened abortion with generally a good prognosis: normal sac size, normal fetal size, fetal heart tones present, gestation and estimated due date (EDD) defined.
• Threatened abortion with increased risk of fetal loss: all the above plus a large amount of intrauterine blood clot, or fetal heart rate less than 100 bpm.
• Inevitable abortion: a very small sac, a normal-sized sac with a very small fetus or a sac with no evidence of a fetus (blighted ovum).
• Missed abortion: the gestation sac contains the fetus, but the fetus is dead, i.e. no fetal heart tones are present.
• If the levels were increasing progressively and doubling every second day, a normal intrauterine pregnancy missed on the previous ultrasound examination would need to be considered.