Problem 49 A woman with palpitations
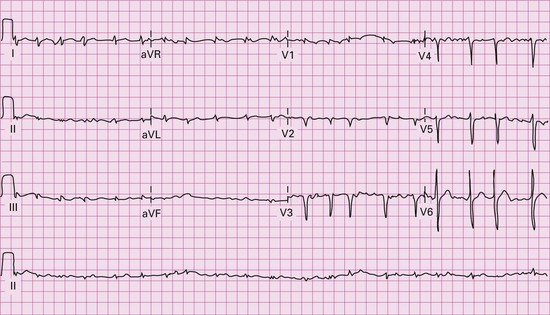
An ECG (Figure 49.1) shows atrial fibrillation.
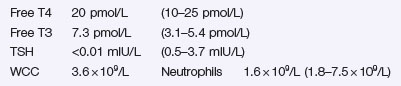
Laboratory investigations include the following:
Investigation 49.1 Summary of results
| Free T4 | 64.8 pmol/L | (10–25 pmol/L) |
| Free T3 | 12.8 pmol/L | (3.1–5.4 pmol/L) |
| TSH | <0.01 mIU/L | (0.5–3.7 mIU/L) |
A thyroid technetium scan (Figure 49.2) shows an enlarged thyroid with generally increased tracer uptake in a patchy distribution consistent with a multinodular goitre.
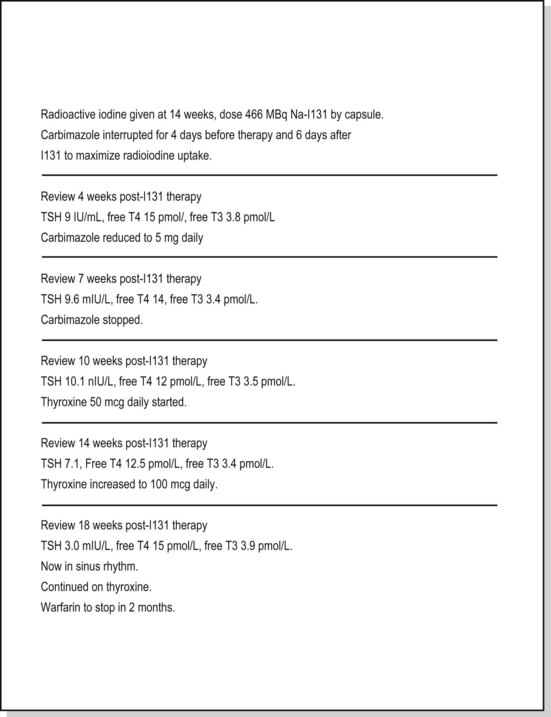
The dose of carbimazole was reduced to 15 mg bd and 3 weeks later to 15 mg daily.
Her subsequent clinical course is described in her notes as follows (Figure 49.3):
www http://www.thyroidmanager.org/. Website covering management of thyroid disease in many sections. Available also via the Endotext website (http://www.endotext.org/)
www http://www.endocrineweb.com. A US based patient centred site but with a lot of well written articles on a whole range of endocrine disorders