Problem 8 A scrotal swelling in a 27-year-old man
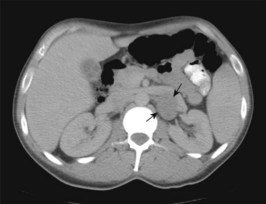
You arrange an urgent ultrasound of the abdomen and testis as well as baseline bloods investigations and testicular tumour markers. In addition, and because of the abdominal findings, you arrange a CT of the chest and abdomen (Figures 8.1, 8.2). The haematological and biochemical values are within normal limits. The tumour marker and imaging studies are shown.
Investigation 8.1 Summary results
| LDH | 922 IU/L | (50–280) |
| AFP | 3 µg/L | (<11) |
| HCG | 7 IU/L | (<5) |
Answers
A.3 Baseline investigations to include the following:
• Full blood count (anaemia from chronic disease), serum electrolytes (possible renal impairment), liver function tests (liver metastases).
• Scrotal imaging with ultrasound to define the testicular mass and to examine the contralateral testis.
• Alpha fetoprotein (AFP) (originates from yolk sac cells and may be produced by pure embryonal carcinoma, teratoma, yolk sac tumour or mixed tumours).
• Human chorionic gonadotropin (hCG) (produced by trophoblastic tissue and seen in all patients with choriocarcinoma and 40–60% of embryonal carcinoma and 5–10% of patients with pure seminomas).
Revision Points