Problem 40 A middle-aged man with sudden visual loss
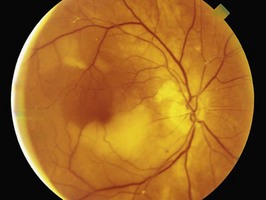
On examination, you measure the blood pressure at 150/95 mmHg. There is no evidence of postural hypotension. Vision, visual fields, pupillary responses, anterior segment examination, gonioscopy and applanation tonometry findings are normal. Visualization of the retina with a direct ophthalmoscope reveals the finding illustrated in Figure 40.1.
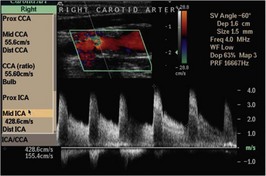
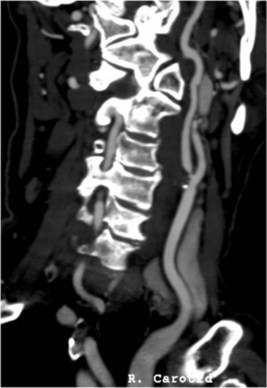
The patient decides in favour of the suggested surgical procedure. In preparation for this, the surgeon orders the radiological study illustrated in Figure 40.2.
Answers
A.2 Figure 40.1 illustrates an embolus at the branch of a retinal artery.
A.3 Essential investigations should include:
Other investigations which may be useful:
Revision Points
Issues to Consider
Amick A., Caplan L.R. Transient monocular visual loss. Comprehensive Ophthalmology Update. 2007;8(2):91-98.
Biousse V., Trobe J.D. Transient monocular vision loss. American Journal of Ophthalmology. 2005;140:717-722.
, http://neurosurgery.mgh.harvard.edu/. The website of the neurosurgical vascular service at Harvard with lots of information about carotid endarterectomy
, www.emedicine.com/emerg/topic604.htm. Transient ischaemic attacks
, www.pvss.org. Website of the Peripheral Vascular Surgical Society with information for patients and professionals including case studies, an atlas and intraoperative photographs