Problem 54 A listless 45-year-old man
A 45-year-old schoolteacher is referred by his GP with deranged liver function tests. He presents with a 1-year history of persistent lethargy. There seem to be no exacerbating or relieving factors. There are no other specific symptoms. Initial blood tests have revealed some abnormalities of his liver enzymes and he has been referred to the hepatology clinic for further investigation. He has never been jaundiced.
On further questioning he admits to having used intravenous heroin in his teens, but says he has been clean since the age of 25. He has never been on a methadone replacement programme.
On examination he appears thin, but looks generally well. There is no evidence of jaundice or lymphadenopathy and he is afebrile. There are several tattoos on his upper torso and you notice some old scars in his antecubital fossae. There are a few spider naevi present on his upper chest, but no other signs of chronic liver disease. Cardiovascular and respiratory examination is unremarkable. The abdomen is soft and non-tender with no evidence of hepatosplenomegaly and no ascites. He is not encephalopathic.
You arrange some further blood tests. The results are as follows:
Investigation 54.1 Summary of results
| White cell count | 7.3 × 109/L | |
| Haemoglobin | 13.5 g/dL | |
| Platelets | 100 × 109/L | |
| INR | 1.3 | |
| Sodium | 138 mmol/L | |
| Potassium | 4.3 mmol/L | |
| Bicarbonate | 24 mmol/L | |
| Urea | 4.6 mmol/L | |
| Creatinine | 67 mmol/L | |
| Glucose | 5.6 mmol/L | |
| Cholesterol | 3.1 mmol/L | |
| Calcium | 2.23 mmol/L | |
| Phosphate | 0.88 mmol/L | |
| Total protein | 65 g/L | |
| Albumin | 43 g/L | |
| Globulin | 22 g/L | |
| ALP | 172 U/L | |
| Bilirubin | 20 mmol/L | |
| AST | 148 U/L | |
| ALT | 136 U/L | |
| GGT | 132 U/L | |
| Autoimmune profile | Negative | |
| IgG | 16.8 | |
| IgA | 3.9 | |
| IgM | 1.3 | |
| Thyroid function | Free T4: 18.1 | TSH: 3.5 |
The following tests are now available:
Investigation 54.2 Summary of results
| Hepatitis B surface antigen | Negative |
| Hepatitis C IgG | Positive |
| Hepatitis C PCR | Positive with a viral load of 1 324 000 IU/mL |
You review him in the outpatient clinic to discuss the results with him.
Investigation 54.3 Summary of results
| White cell count | 2.9 × 109/L |
| Haemoglobin | 10.3 g/dL |
| Platelets | 67 × 109/L |
| INR | 1.9 |
| Albumin | 28 g/L |
| Globulin | 22 g/L |
| ALP | 312 U/L |
| Bilirubin | 87 µmol/L |
| AST | 111 U/L |
| ALT | 165 U/L |
| GGT | 278 U/L |
| Alphafetoprotein 1885 kiu/L (0–5) |
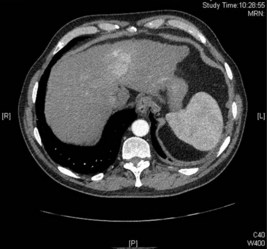
The following investigation is performed:
Answers
• He has hepatitis C. It is likely that he contracted the virus through IV drug use in his teens and has been infected between 15 and 20 years. His viral load is high.
• Hepatitis C is a blood-borne virus that is spread through contact with infected blood. Only 15–20% of people infected with hepatitis C will clear the virus while 80–85% of infected people will develop chronic infection. In order to confirm chronic infection, a positive antibody test must be accompanied with a positive hepatitis C PCR.
• The main complication of chronic hepatitis C is the development of cirrhosis and the subsequent risk of developing hepatocellular carcinoma. Patients with hepatitis C often experience lethargy and the reason for this is not entirely clear. Commonly, people with hepatitis C infection are asymptomatic.
• There are also extra-hepatic complications of hepatitis C including: cryoglobulinaemia, leading to glomerulonephritis and a vasculitic skin rash.
• There are six genotypes of hepatitis C. There is treatment available for hepatitis C and this will depend on his genotype.
• It is important to cut down alcohol use in the context of hepatitis C as concomitant alcohol use may lead to acceleration of his liver disease.
• All patients with a diagnosis of hepatitis C should be screened for other blood-borne viruses including HIV.
He also needs a blood test to check his genotype. This shows him to be genotype 1.
Interferon
Revision Points
Hepatocellular Carcinoma
Treatment
• Traditionally the outcome for most HCCs has been poor with curative resection of transplantation only suitable for 5% of patients. However, treatment options have changed dramatically over the last 10 years.
• Resection is still an option in patients with well-preserved liver function and without portal hypertension. Liver transplantation remains the gold standard but tumours must be small (<5 cm or no more than 3 lesions <3 cm in diameter) and the availability of donor organs is a major limiting factor.
• Small tumours can now be treated very successfully with ablative techniques such as radiofrequency ablation.