Problem 31 A 68-year-old woman with breathlessness and yellow sputum
You ponder the differentials, and move on to examining the patient.
The following result is obtained:
Investigation 31.1 Arterial blood gas analysis on air
| pO2 | 41 mmHg |
| pCO2 | 75 mmHg |
| pH | 7.25 |
| HCO3 | 32 mmol/L |
Investigation 31.2 Arterial blood gas analysis on 3 L/min O2
| pO2 | 58 mmHg |
| pCO2 | 89 mmHg |
| pH | 7.21 |
| HCO3 | 32 mmol/L |
The electrolytes are normal other than bicarbonate.
The chest X-ray is shown in Figure 31.1.
An ECG shows a sinus tachycardia with a right axis deviation and a prominent R wave in lead V1.
Investigation 31.5 Arterial blood gases on air
| pO2 | 50 mmHg |
| pCO2 | 61 mmHg |
| pH | 7.40 |
| HCO3 | 34 mmol/L |
The patient is told firmly that she must stop smoking immediately.
Q.9
What do these results tell you? How will you manage the patient before discharge and in the future?
Answers
The differential diagnosis includes adult-onset asthma and bronchiectasis, and heart failure.
A.2 During the examination of this patient you will focus on:
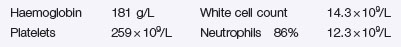
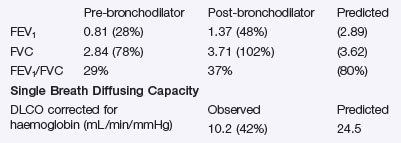
A.3 Initial investigations (and reasons why):
Revision Points
Chronic Obstructive Pulmonary Disease (COPD)
Diagnosis
Treatment
, www.COPDX.org.au. The COPD-X Plan, Australian and New Zealand guidelines for the management of chronic obstructive pulmonary disease
, www.GOLDCOPD.com. GOLD – Global Initiative for Chronic Obstructive Lung Disease
, www.lungfoundation.com.au. The Australian Lung Foundation is a key agent of change in Australia for promoting the understanding, management and relief of lung disease