Problem 25 A 68-year-old woman with a leg ulcer
A 68-year-old woman attends the outpatient department with an ulcer on her left leg. She tells you it has been present for 2 months. She remembers knocking her leg on the end of her bed. The ulcer on her leg has become fairly painful over the last week. She has had a similar ulcer on her leg in the past which was treated by ‘bandaging’.
She is not a diabetic, but does take tablets for her blood pressure. She is not sure what these are. She is on no other medications. She has had no other illnesses of note, but has had varicose veins ever since the birth of her children. On further questioning, she reveals that the left leg was very swollen for 2 or 3 months after her third pregnancy but she never had any tests to see why. This has been her ‘bad leg’ ever since. Her leg ulcer is shown in Figure 25.1.
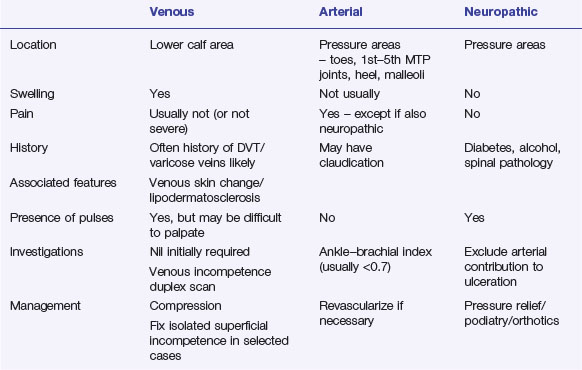
Revision Points