Problem 9 A 63-year-old woman with a screen-detected abnormality
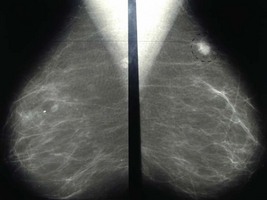
The mammogram is reviewed (Figure 9.1).
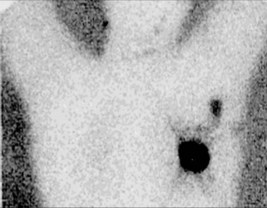
A surgical procedure is planned for the patient. The following investigation is performed immediately before the operation (Figure 9.2).
Answers
A.2 The following features on the mammogram would suggest malignancy:
The following features are more suggestive of a lesion being benign:
The important pathological prognostic factors currently used to determine prognosis are:
, www.cancer.gov. An excellent website from the US National Cancer Institute covering many aspects of cancer including consensus statements on the management of breast cancer
, www.cancerscreening.nhs.uk. An interesting website covering various aspects of cancer screening including for breast cancer in the UK
, www.nbocc.com. The website of the National Breast and Ovarian Cancer Centre. Australia’s most significant breast cancer website providing consumer information, regular breast cancer updates and recommendations to medical practitioners about best clinical practice.
. Breast surgery – a companion to specialist surgical practice. Dixon J.M., editor, third ed. London: Elsevier Saunders. 2006.