Problem 23 A 59-year-old man with calf pain
Q.1
What is the likely cause of his symptoms and what other information would you like from the history?
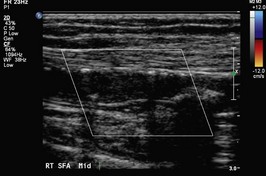
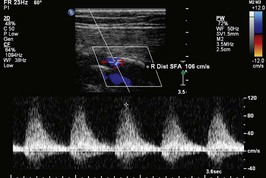
On your advice he agrees to see a vascular surgeon, who recommends that an arterial duplex scan is performed. This is shown in Figures 23.1, 23.2 and 23.3. Figure 23.2 demonstrates an occluded segment of superficial femoral artery (SFA). The waveforms above this lesion (23.1) are normal but the waveforms distally (23.3) are damped consistent with the occlusion just proximal to this segment. Subsequently he recommends a CT angiogram (shown in Figure 23.4). These are AP views with the patient’s right leg on the left side of Figure 23.1.
Answers
Major risk factors which you must ask about are:
Typical cardiovascular co-morbidities are:
A.4 You should advise him in simple language that:
Revision Points
Natural History
Management
Issues to Consider
, www.scvir.org. Home page of the American Society of Cardiovascular and Interventional Radiology. Interesting information and links about peripheral vascular diseases and the role of endovascular therapies
Norgen L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II), TASC II Working Group. Journal of Vascular Surgery, 45. 2007: S1-S67.