Answers
A.1 She may have poorly controlled essential hypertension or hypertension secondary to underlying kidney disease, and an intercurrent problem such as a viral illness which has produced the headache and nausea. However, she has marked hypertension for a young person and may be in a hypertensive crisis. In this situation encephalopathy can occur which would be suggested by the headache and nausea. Her past medical history will be important as she may give a history of known poorly controlled hypertension or renal disease. You must inquire as to whether she may be pregnant (pre-eclampsia), although such severe hypertension would be very uncommon in early pregnancy.
You should ask her about the severity of her previously diagnosed hypertension, and whether she knows of her recent blood pressure readings – if it has been progressively increasing over several months the immediate risk is lower than if this has been a sudden rise over a few days or weeks.
Ask her about other symptoms associated with hypertensive encephalopathy such as irritability, visual disturbances, confusion, altered consciousness and seizures.
Ask about symptoms that might suggest an underlying disorder to account for her hypertension, such as:
You will also need to ask about symptoms suggestive of hypertensive damage to the retina (visual deterioration) or the cardiovascular system, including acute myocardial ischaemia or cardiac failure (angina, dyspnoea, orthopnoea, ankle swelling), and aortic dissection (back pain).
A drug history is vital, including past use of analgesics (particularly NSAIDs: analgesic nephropathy), current use of drugs associated with hypertension, e.g. oral contraceptive pill, sympathomimetics (e.g. nasal decongestants), steroids, some antidepressants (including venlafaxine) and combinations of antidepressants associated with a risk of serotonergic syndrome (e.g. SSRIs and monoamine oxidase inhibitors). The patient’s use of tobacco, alcohol and illicit drugs, particularly cocaine and amphetamine derivatives, should also be explored.
A.2 On examination you will need to look for evidence of hypertensive damage to:
Note: the presence of any acute features, especially neurological symptoms or signs, retinal haemorrhages, exudates or optic disc swelling, and abnormalities on urinalysis, suggests the presence of accelerated/malignant hypertension requiring emergency treatment.
You also need to look for features to suggest the underlying aetiology if the patient has secondary hypertension:
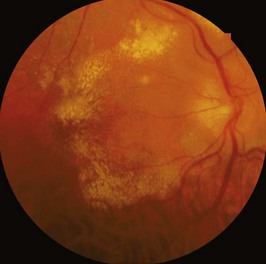
A.3 Figure 38.1 shows:
This is grade 3 hypertensive retinopathy. There is considerable hard exudate in the posterior pole with formation of a partial macular star.
In grade 4 retinopathy optic disc swelling would also be present, but there is no evidence that clinical outcomes differ on the basis of the fundoscopic findings and both grade 3 and grade 4 should be regarded as indicators of hypertensive emergency.
A.4 This is a hypertensive crisis because of the very high blood pressure readings together with symptoms and signs of impending or progressive target organ dysfunction. It is a medical emergency, and requires immediate admission to hospital, preferably to intensive care.
A.5 This woman may have essential (primary) hypertension as she does have a positive family history and the hypertension may be exacerbated by smoking and alcohol. However, the severity of her hypertension at her young age suggests a specific underlying cause. The common causes of secondary hypertension include:
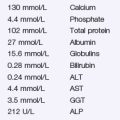
With her anxiety, sweating and resting tachycardia, it is prudent to exclude a phaeochromocytoma, but her abdominal bruit suggests the possibility of renal artery stenosis. Baseline investigations should include:
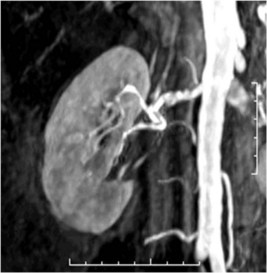
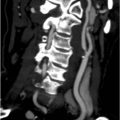
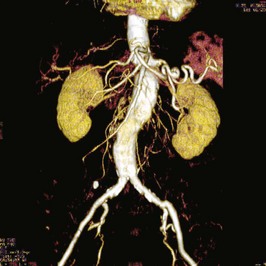
The next investigation of choice would be a non-invasive screening test for renal artery stenosis. Several different tests can be done, and these include, duplex ultrasound scanning (with or without contrast enhancement), spiral CT angiography and gadolinium-enhanced magnetic resonance angiography (MRA), and radionuclidescans with ACE inhibitor challenge. MRI studies are becoming more technologically advanced and are now able to provide details of morphological damage and function of the kidney itself, allowing better prediction of the potential outcomes of reperfusion. Radionuclide studies are no longer recommended as first line screening because of poor sensitivity and specificity. Catheter angiography of the renal arteries is the ‘gold standard’ and can identify disease in the branch vessels as well as in the main renal arteries. The site of stenosis varies depending on the nature of the disease, with atherosclerotic renal artery stenosis being more likely to occur at the origin of the renal artery, and fibromuscular dysplasia more likely to be found in the middle or distal part of the artery.
Given the clinical context, this patient should also be screened for a phaeochromocytoma by assessing production of catecholamines. This is usually done by performing a 24-hour urine collection, assayed for excreted catecholamines and their metabolites (creatinine, total catecholamines, vanillylmandelic acid, and metanephrines). Ideally, uring should be collected during a hypertensive crisis where hormone levels are at their highest. Serum plasma metaneprhines is also a useful test, which is more sensitive but less specific.
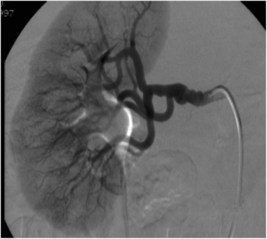
A.6 Figure 38.2 is a CT angiogram defining the abdominal aorta and its main branches, including the two renal arteries. There are several narrowed segments in the left renal artery, with a pattern referred to as ‘beading’. This is typically caused by Fibromuscular Dysplasia. There are no changes to suggest significant atheromatous disease of the renal arteries (although there is mild calcific plaque seen in the aorta below the renal arteries). Figure 38.3 is a close-up image of the left renal CT scan, demonstrating the charactieristic beadin pattern. Figure 38.4 shows a renal MR Angiogram of a different patient with right renal artery fibromuscular dysplasia. MR Angiography is beoming more commonly performed, as gadolinium is less reno-toxic than iodine-based contrast agents (unless the patient has severe renal impairment, in which case all forms of imaging contrast have risks).
The preferred treatment for Fibromuscular Dysplasia is percutaneous balloon angioplasty +/− stenting of the diseased segments.
Figure 38.5 is an invasive renal angiogram of the same patient shown in Figure 38.4, during preparation for balloon angioplasty and stenting procedure.