Problem 45 A 31-year-old woman with vertigo
Q.2
How do you differentiate central from peripheral causes of vertigo? What are some causes of each?
Q.3
How do you interpret this woman’s neurological signs?
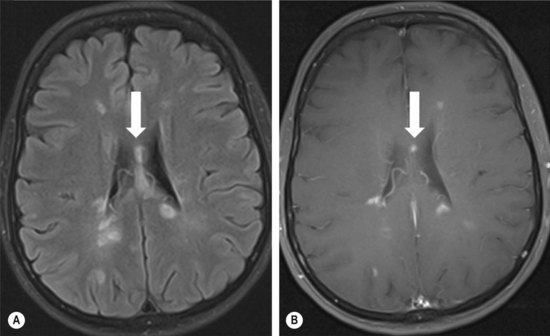
Given the probable site of the problem, the patient is referred to a neurologist. Her vertigo had improved but has not resolved completely. Various tests were performed. Figure 45.1A, B was taken from one of the tests.
Q.5
What is the likely diagnosis and what other tests could be done to further support the diagnosis?
Answers
You will also need to perform a careful general physical examination.
A.2 Signs suggesting central nervous system involvement include:
Examples of central lesions causing vertigo include:
Examples of peripheral causes of vertigo include:
There are multiple hyperintense periventricular FLAIR signal foci, as well as callosal hyperintensities and several juxtacortical lesions. Several lesions were also seen in the posterior fossa and spinal cord (not shown). Some, but not all lesions demonstrated gadolinium enhancement (see Figure 45.1B), suggesting that lesions are of differing stages. This picture is almost pathognomonic for multiple sclerosis (MS), particularly with this clinical presentation.
A.5 This woman has a number of features in her illness that point to central nervous system disease:
Revision Points
Multiple Sclerosis
Diagnosis
The differential diagnosis includes:
Optic Neuritis
Vertigo
Clinical symptoms to assist in deciding whether vertigo is of central or peripheral origin are shown in Table 45.1.
| Peripheral | Central | |
|---|---|---|
| Characteristics | Severe, episodic | Mild to severe, semicontinuous |
| Precipitants | Head movement, typically turning, lying down in bed | May be exacerbated by movement |
| Exacerbating factors | Head movement | Head movement |
| Interval after movement | Few seconds | Immediate |
| Duration | Seconds to continuous | Continuous |
| Nystagmus | Mixed horizontal/torsional, suppressed by fixation | Horizontal, vertical, gaze provoked, not suppressed by fixation |
| Associated features | Deafness, tinnitus | Brainstem signs, e.g. facial numbness, diplopia, ataxia, weakness |
| Causes | Ménière’s disease, vestibular neuronitis, benign paroxysmal positional vertigo, middle ear disease | Ischaemia, demyelination |