Problem 29 A 25-year-old woman with chest pain and breathlessness
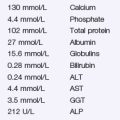
Complete blood picture and baseline electrolytes are normal.
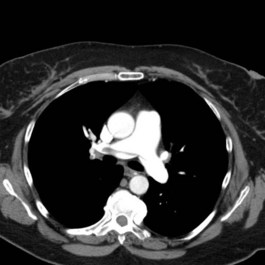
An imaging study is undertaken and two images from the sequence are shown (Figure 29.2). Her left Doppler showed an extensive clot into proximal femoral veins.
Q.4
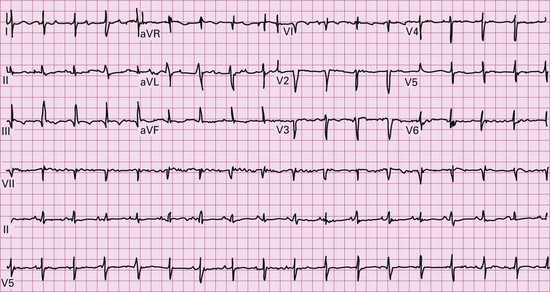
What do these images show? What clinical signs may reflect the underlying severity of the condition?
Answers
Further specific questions should be asked to determine her pre-test probability of DVT/PE:
A.2 The following investigations must be undertaken:
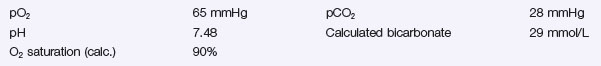
A.3 The arterial blood gases show the following:
Testing for Prothrombotic Disorders
Thrombolysis should be performed in consultation with a major centre experienced in PE management.
Contraindications to Thrombolysis
Relative
She requires ongoing anticoagulation both in the short and long terms.
Revision Points
Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Guidelines on the diagnosis and management of acute pulmonary embolism. European Heart Journal. 2008;29:2276-2315.
Hamilton-Craig C.R., McNeil K., Dunning J.D., et al. Treatment options and strategies for acute severe pulmonary embolism. Internal Medicine Journal. 2008;38:657-667.
McNeil K., Dunning J.D. Chronic thromboembolic pulmonary hypertension (CTEPH). Heart. 2007;93:1152-1158.